Abstract
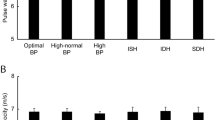
Many unexplained sex differences have been observed in blood pressure (BP) related morbidity. However, there has been little research about the most obvious difference between men and women—body size. Given that blood vessels are organs of tubular shape, we hypothesized that correction of BP for body surface area (BSA), a two-dimensional measurement of body size, would allow comparison of BP load between men and women. We assessed the relationship of 24-h ambulatory BP measurements and BSA in 534 participants (mean age 61 ± 3 years, 51% women) from the Helsinki Birth Cohort Study. The study subjects had no previous medication affecting vasculature or BP. When BP values were adjusted for age, smoking, physical activity, and body fat percentage, males had higher ambulatory daytime mean systolic BP (131 mmHg vs. 127 mmHg, p < 0.001), diastolic BP (83 mmHg vs. 78 mmHg, p < 0.001), and mean arterial pressure (100 mmHg vs. 96 mmHg, p < 0.001) than females. However, all BP components per unit of BSA were significantly lower in males: daytime mean systolic BP (65 mmHg vs. 71 mmHg, p < 0.001), diastolic BP (41 mmHg vs. 44 mmHg, p < 0.001), pulse pressure (24 mmHg vs. 28 mmHg, p = 0.013), and mean arterial pressure (49 mmHg vs. 54 mmHg, p < 0.001). The same phenomenon was observed in night-time BP values. BP load per BSA is higher in women than in men, which may explain many reported sex differences in cardiovascular morbidity. Relatively small-sized individuals might benefit from a more aggressive therapeutic strategy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Go A, Mozaffarian D, Roger V.on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee et al. Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation. 2013;127:e77–86.
Robitaille C, Dai S, Waters C, Loukine L, Bancej C, Quach S, et al. Diagnosed hypertension in Canada: incidence, prevalence and associated mortality. CMAJ. 2012;184:E49–56.
Prince M, Ebrahim S, Acosta D, Ferri CP, Guerra M, Huang Y, et al. Hypertension prevalence, awareness, treatment and control among older people in Latin America, India and China: a 10/66 cross-sectional population-based survey. J Hypertens. 2011;30:177–87.
Gee M, Bienek A, McAlister F, Robitaille C, Joffres M, Tremblay MS, et al. Factors associated with lack of awareness and uncontrolled high blood pressure among Canadian adults with hypertension. Can J Cardiol. 2012;28:375–82.
Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA 2010;303:2043–50.
Piro M, Della Bona R, Abbate A, Biasucci LM, Crea F. Sex-related differences in myocardial remodeling. J Am Coll Cardiol. 2010;55:1057–65.
Borlaug BA, Redfield MM. Diastolic and systolic heart failure are distinct phenotypes within the heart failure spectrum. Circulation. 2011;123:2006–14.
Okin P, Gerdts E, Kjeldsen S, Stevo J, Edelman JM, Dahlof B, Devereux RB, for the Losartan Intervention for Endpoint Reduction in Hypertension Study Investigators. Gender difference in regression of electrocardiographic left ventricular hypertrophy during antihypertensive therapy. Hypertension. 2008;52:100–6.
Rossi P, Frances Y, Kingwell BA, Ahimastos AA. Gender differences in artery wall biomechanical properties throughout life. J Hypertens. 2011;29:1023–33.
Shim CY, Park S, Choi D, Yang WI, Cho IJ, Choi EY, et al. Sex differences in central hemodynamics and their relationship to left ventricular diastolic function. J Am Coll Cardiol. 2011;57:1226–33.
Hamburg NM, Palmisano J, Larson MG, Sullivan LM, Lehman BT, Vasan RS, et al. Relation of brachial and digital measures of vascular function in the community: the Framingham heart study. Hypertension. 2011;57:390–6.
Benetos A, Thomas A, Joly L, Blacher J, Pannier B, Labat C, et al. Pulse pressure amplification, a mechanical biomarker of cardiovascular risk. J Am Coll Cardiol. 2010;55:1032–7.
Emerging Risk Factors Collaboration. Adult height and the risk of cause-specific death and vascular morbidity in 1 million people: individual participant meta-analysis. Int J Epidemiol. 2012;41:1419–33.
Korhonen PE, Kautiainen H, Eriksson JG. The shorter the person, the higher the blood pressure: a birth-cohort study. J Hypertens. 2017;35:1170–7.
Barker DJP, Osmond C, Forsen T, Kajantie E, Eriksson JG. Trajectories of growth among children who have coronary events as adults. N Engl J Med. 2005;353:1802–9.
Mosteller RD. Simplified calculation of body surface area. N Engl J Med. 1987;317:1098.
Ahn Y, Garruto RM. Estimations of body surface area in newborns. Acta Paediatr. 2008;97:366–70.
O’Brien E, Asmar R, Beilin L, Imai Y, Mallion JM, Mancia G.On behalf of the European Society of Hypertension Working Group on Blood Pressure Monitoring et al. European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens. 2003;21:821–48.
Woolcott OO, Bergman RN. Relative fat mass (RFM) as a new estimator of whole-body far percentage—a cross-sectional study in American adult individuals. Sci Rep. 2018;8:10980.
Lakka TA, Venäläinen JM, Rauramaa R, Tuomilehto J, Salonen JT. Relation of leisure-time physical activity and cardiorespiratory fitness to the risk of acute myocardial infarction. N Engl J Med. 1994;330:1549–54.
Wasenius N, Venojärvi M, Manderoos S, Surakka J, Lindholm H, Heinonen OJ, et al. Unfavorable influence of structured exercise program on total leisure-time physical activity. Scand J Med Sci Sports. 2014;24:404–13.
Guyton AG, Hall JE. Textbook of Medical Physiology. 9th ed., W.B. Saunders Co; 1996. p. 166.
Lemos PA, Ribeiro EE, Perin MA, Kajita LJ, de Magalhaes MA, Falcao JLAA, et al. Angiographic segment size in patients referred for coronary intervention is influenced by constitutional, anatomical, and clinical features. Int J Cardiovasc Imaging. 2007;23:1–7.
Hiteshi AK, Li D, Gao Y, Chen A, Flores F, Mao SS, et al. Gender differences in coronary artery diameter are not related to body habitus or left ventricular mass. Clin Cardiol. 2014;37:605–9.
Orshal JM, Khalil RA. Gender, sex hormons, and vascular tone. Am J Physiol Regul Integr Comp Physiol. 2004;286:R233–249.
Reeves MJ, Bushnell CD, Howard G, Gargano JW, Duncan PW, Lynch G, et al. Sex differences in stroke: epidemiology, clinical presentation, medical care, and outcomes. Lancet Neurol. 2008;7:915–26.
Sara JD, Widmer RJ, Matsuzawa Y, Lennon RJ, Lerman LO, Lerman A. Prevalence of coronary microvascular dysfunction among patients with chest pain and nonobstructive coronary artery disease. JACC Cardiovasc Interv. 2015;8:1445–53.
Neugarten J, Acharaya A, Silbiger S. Effect of gender on the progression of nondiabetic renal disease: a meta-analysis. J Am Soc Nephrol. 2000;11:319–29.
Paton JF, Dickinson CJ, Mitchell G. Harvey Cushing and the regulation of blood pressure in giraffe, rat and man: Introducing Cushing´s mechanism. Exp Physiol. 2009;94:11–17.
Stramba-Badiale M, Fox KM, Priori SG, Collins P, Daly C, Graham I, et al. Cardiovascular diseases in women: a statement from the policy conference of the European Society of Cardiology. Eur Heart J. 2006;27:994–1005.
Zafrir B, Salman N, Crespo-Leiro MG, Anker SD, Coats AJ, Ferrari R.on behalf of the Heart Failure Long-Term Registry Investigators et al. Body surface area as a prognostic marker in chronic heart failure patients: results from the Heart Failure Registry of the Heart Failure Association of the European Society of Cardiology. Eur Heart J. 2016;18:859–68.
Futter JE, Cleland JG, Clark AL. Body mass indices and outcome in patients with chronic heart failure. Eur Heart J. 2011;13:207–13.
Tarnoki AD, Tarnoki DL, Bogl LH, Medda E, Fagnani C, Nistico L, et al. Association of body mass index with arterial stiffness and blood pressure components: a twin study. Atherosclerosis. 2013;229:388–95.
Verbraecken J, Van de Heyning P, De Backer W, Van Gaal L. Body surface area in normal weight, overweight, and obese adults. A comparison study. Metabolism. 2006;55:515–24.
Funding
The Helsinki Birth Cohort Study has been supported by grants from Finska Läkaresällskapet, the Finnish Special Governmental Substudy for Health Sciences, Academy of Finland, Samfundet Folkhälsan, Liv och Hälsa, and Signe and Ane Gyllenbergs Foundation. The funding sources did not participate in the design of the study, the analysis or the interpretation of the data, the writing of this paper, or the process to submit this article for publication. The independence of the researchers from funders is declared.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The Ethics Committee for Epidemiology of Helsinki and Uusimaa Hospital District approved the study.
Informed consent
Written informed consent was obtained from each subject before any procedures were carried out.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Korhonen, P.E., Palmu, S., Kautiainen, H. et al. Blood pressure load per body surface area is higher in women than in men. J Hum Hypertens 35, 371–377 (2021). https://doi.org/10.1038/s41371-020-0339-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-020-0339-z