Abstract
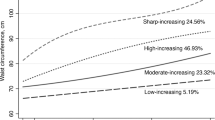
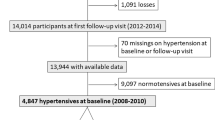
Whether dynamic change in waist circumference is associated with progression from prehypertension to hypertension is not well understood. We explored this issue. A total of 4221 prehypertensive adults ≥18 years were enrolled during 2007–2008 and followed up during 2013–2014. Participants were classified by percentage waist-circumference change at follow-up: ≤−2.5, −2.5 to ≤2.5, 2.5 to ≤5.0, and >5.0%. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated with logistic regression models, with stable waist-circumference change (−2.5 to 2.5%) as the reference. During the 6 years of follow-up, 1464 prehypertensive patients (851 women) showed progression to hypertension, with an incidence rate of 32.7% for men and 36.3% for women. As compared with stable waist circumference, a waist-circumference gain > 5.0% was associated with increased hypertension risk: adjusted ORs (95% CI) were 1.08 (1.01–1.14) for men and 1.09 (1.04–1.15) for women. The risk also decreased significantly for men with ≥2.5% waist-circumference loss (OR = 0.94, 95% CI 0.88–1.00). We found a linear association between percentage waist-circumference gain and risk of progression from prehypertension to hypertension for both sexes by restricted cubic splines (pnonlinearity = 0.772 for men and 0.779 for women). For each 10% gain in waist circumference, the risk increased by 8% for men and 5% for women. The association remained significant for both sexes in a subgroup analysis by abdominal obesity at baseline. The long-term gain in waist circumference significantly increased the risk of progression from prehypertension to hypertension for both sexes in a rural Chinese population, regardless of abdominal obesity status at baseline.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr., et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–52.
Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D. Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: a cohort study. Lancet. 2001;358:1682–6.
Julius S, Nesbitt SD, Egan BM, Weber MA, Michelson EL, Kaciroti N, et al. Feasibility of treating prehypertension with an angiotensin-receptor blocker. N. Engl J Med. 2006;354:1685–97.
Mullican DR, Lorenzo C, Haffner SM. Is prehypertension a risk factor for the development of type 2 diabetes? Diabetes Care. 2009;32:1870–2.
Kokubo Y, Kamide K, Okamura T, Watanabe M, Higashiyama A, Kawanishi K, et al. Impact of high-normal blood pressure on the risk of cardiovascular disease in a Japanese urban cohort: the Suita study. Hypertension. 2008;52:652–9.
Egan BM, Julius S. Prehypertension: risk stratification and management considerations. Curr Hypertens Rep. 2008;10:359–66.
Huang Y, Su L, Cai X, Mai W, Wang S, Hu Y, et al. Association of all-cause and cardiovascular mortality with prehypertension: a meta-analysis. Am Heart J. 2014;167:160–168.e1.
Guo X, Zou L, Zhang X, Li J, Zheng L, Sun Z, et al. Prehypertension: a meta-analysis of the epidemiology, risk factors, and predictors of progression. Tex Heart Inst J. 2011;38:643–52.
Guo X, Zheng L, Zhang X, Zou L, Li J, Sun Z, et al. The prevalence and heterogeneity of prehypertension: A meta-analysis and meta-regression of published literature worldwide. Cardiovasc J Afr. 2012;23:44–50.
Gallagher D, Visser M, Sepulveda D, Pierson RN, Harris T, Heymsfield SB. How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups? Am J Epidemiol. 1996;143:228–39.
Folsom AR, Kushi LH, Anderson KE, Mink PJ, Olson JE, Hong CP, et al. Associations of general and abdominal obesity with multiple health outcomes in older women: the Iowa Women’s Health Study. Arch Intern Med. 2000;160:2117–28.
Rexrode KM, Carey VJ, Hennekens CH, Walters EE, Colditz GA, Stampfer MJ, et al. Abdominal adiposity and coronary heart disease in women. Jama. 1998;280:1843–8.
Yalcin BM, Sahin EM, Yalcin E. Which anthropometric measurements is most closely related to elevated blood pressure? Fam Pract. 2005;22:541–7.
Deng WW, Wang J, Liu MM, Wang D, Zhao Y, Liu YQ, et al. Body mass index compared with abdominal obesity indicators in relation to prehypertension and hypertension in adults: the CHPSNE study. Am J Hypertens. 2013;26:58–67.
Pitsavos C, Chrysohoou C, Panagiotakos DB, Lentzas Y, Stefanadis C. Abdominal obesity and inflammation predicts hypertension among prehypertensive men and women: the ATTICA Study. Heart Vessel. 2008;23:96–103.
Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM. Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2003;42:878–84.
Balkau B, Picard P, Vol S, Fezeu L, Eschwege E, Group DS. Consequences of change in waist circumference on cardiometabolic risk factors over 9 years: data from an Epidemiological Study on the Insulin Resistance Syndrome (DESIR). Diabetes Care. 2007;30:1901–3.
Chuang SY, Chou P, Hsu PF, Cheng HM, Tsai ST, Lin IF, et al. Presence and progression of abdominal obesity are predictors of future high blood pressure and hypertension. Am J Hypertens. 2006;19:788–95.
Luo WS, Guo ZR, Hu XS, Zhou ZY, MingWu, Zhang LJ, et al. A prospective study on association between 2 years change of waist circumference and incident hypertension in Han Chinese. Int J Cardiol. 2013;167:2781–5.
Miyatake N, Matsumoto S, Fujii M, Numata T. Reducing waist circumference by at least 3 cm is recommended for improving metabolic syndrome in obese Japanese men. Diabetes Res Clin Pract. 2008;79:191–5.
Williams PT. Increases in weight and body size increase the odds for hypertension during 7 years of follow-up. Obesity. 2008;16:2541–8.
Luo WS, Guo ZR, Hu XS, Zhou ZY, Wu M, Zhang LJ, et al. A prospective study on the association between dynamic change of waist circumference and incident hypertension. Zhonghua liu xing bing xue za zhi = Zhonghua liuxingbingxue zazhi. 2012;33:28–31.
Zhao Y, Zhang M, Luo X, Wang C, Li L, Zhang L, et al. Association of 6-year waist circumference gain and incident hypertension. Heart. 2017;103:1347–52.
Luo W, Chen F, Guo Z, Wu M, Hao C, Zhou Z, et al. Comparison of the suitability of 2 years change in waist circumference and body mass index in predicting hypertension risk: a Prospective Study in Chinese-Han. Iran J Public Health. 2014;43:1212–20.
Yang G, Wang Y, Zeng Y, Gao GF, Liang X, Zhou M, et al. Rapid health transition in China, 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet. 2013;381:1987–2015.
Zhao Y, Zhang M, Luo X, Yin L, Pang C, Feng T, et al. Association of obesity categories and high blood pressure in a rural adult Chinese population. J Hum Hypertens. 2016;30:613–8.
Bondy SJ, Victor JC, Diemert LM. Origin and use of the 100 cigarette criterion in tobacco surveys. Tob Control. 2009;18:317–23.
Alberti KG, Zimmet P, Shaw J. The metabolic syndrome—a new worldwide definition. Lancet. 2005;366:1059–62.
Bairaktari E, Hatzidimou K, Tzallas C, Vini M, Katsaraki A, Tselepis A, et al. Estimation of LDL cholesterol based on the Friedewald formula and on apo B levels. Clin Biochem. 2000;33:549–55.
Vague J. Sexual differentiation. A factor affecting the forms of obesity. Presse Med. 1947;30:339–40.
Okosun IS, Cooper RS, Rotimi CN, Osotimehin B, Forrester T. Association of waist circumference with risk of hypertension and type 2 diabetes in Nigerians, Jamaicans, and African-Americans. Diabetes Care. 1998;21:1836–42.
Gus M, Cichelero FT, Moreira CM, Escobar GF, Moreira LB, Wiehe M, et al. Waist circumference cut-off values to predict the incidence of hypertension: an estimation from a Brazilian population-based cohort. Nutr Metab Cardiovasc Dis. 2009;19:15–9.
Seo DC, Choe S, Torabi MR. Is waist circumference ≥102/88cm better than body mass index ≥30 to predict hypertension and diabetes development regardless of gender, age group, and race/ethnicity? Meta-analysis. Prev Med. 2017;97:100–8.
Schwingshackl L, Schwedhelm C, Hoffmann G, Knuppel S, Iqbal K, Andriolo V, et al. Food groups and risk of hypertension: a systematic review and dose-response meta-analysis of prospective studies. Adv Nutr. 2017;8:793–803.
Acknowledgements
We thank Mrs Laura Smales for proofreading of the paper.
Funding
This work was supported by the National Natural Science Foundation of China [grant nos. 81373074, 81402752, and 81673260]; the Natural Science Foundation of Guangdong Province [grant no. 2017A030313452]; the Medical Research Foundation of Guangdong Province [grant no. A2017181]; and the Science and Technology Development Foundation of Shenzhen [grant nos. CYJ20140418091413562, JCYJ20160307155707264, JCYJ20170412110537191, and JCYJ20170302143855721]. The funding body has no role in the design of the study, collection and analysis of data, or decision to publish.
Author information
Authors and Affiliations
Contributions
PQ, DH, and MZ conceived, designed, and performed the work. PQ performed data analysis and drafted the paper. QC, TW, XC, YZ, QZ, QL, CG, DL, GT, XW, RQ, MH, SH, LL, and YL acquired the data and revised the paper. MZ has had full access to the data in the study and final responsibility for the decision to submit for publication. All authors approved the final paper and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Qin, P., Chen, Q., Wang, T. et al. Association of 6-year waist-circumference change with progression from prehypertension to hypertension: the Rural Chinese Cohort Study. J Hum Hypertens 35, 215–225 (2021). https://doi.org/10.1038/s41371-020-0322-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-020-0322-8
This article is cited by
-
Associations of the baseline level and change in glycosylated hemoglobin A1c with incident hypertension in non-diabetic individuals: a 3-year cohort study
Diabetology & Metabolic Syndrome (2022)
-
Hypertriglyceridemic-waist phenotype is strongly associated with cardiovascular risk factor clustering in Chinese adolescents
Scientific Reports (2022)