Abstract
Blood pressure (BP) management posed great challenge in hemodialysis (HD) population. We conducted a dose-response meta-analysis to investigate the quantitative features and the potential threshold effect of the associations between peridialysis BP levels and all-cause mortality risk in HD population. We searched all of the prospective cohort studies (published before 18 March 2017) on the associations between peridialysis BP levels and all-cause mortality risk. A total of 229,688 prevalent HD patients from 8 studies were included. Significant non-linear associations were noted between peridialytic BP levels and all-cause mortality risk. Significant increased risk of death was found in four peridialysis BP ranges, that is, low levels of predialysis SBP (<135 mmHg, 140 mmHg as the reference), two extremes of predialysis DBP (<55 and >95 mmHg, 90 mmHg as the reference), high levels of postdialysis SBP (>180 mmHg, 130 mmHg as the reference), and low levels of postdialysis DBP (<75 mmHg, 80 mmHg as the reference). Threshold effect was determined in the associations between peridialysis BP and all-cause mortality risk, and potential BP thresholds were identified (149 mmHg for predialysis SBP, 79 mmHg for predialysis DBP, 147 mmHg for postdialysis SBP and 76 mmHg for postdialysis DBP). In conclusion, the proposed peridialysis BP ranges and the threshold values could help clinicians identify high risk HD patients. The interpretation of the peridialysis BP mortality associations should be based on the features of HD population (especially the cardiovascular conditions, volume status and the dialysis vintage).
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Zager PG, Nikolic J, Brown RH, Campbell MA, Hunt WC, Peterson D, et al. “U” curve association of blood pressure and mortality in hemodialysis patients. Kidney Int. 1998;54:561–9.
Port FK, Hulbert-Shearon TE, Wolfe RA, Bloembergen WE, Golper TA, Agodoa LY, et al. Predialysis blood pressure and mortality risk in a national sample of maintenance hemodialysis patients. Am J Kidney Dis. 1999;33:507–17.
Kalantar-Zadeh K, Kilpatrick RD, McAllister CJ, Greenland S, Kopple JD. Reverse epidemiology of hypertension and cardiovascular death in the hemodialysis population: the 58th annual fall conference and scientific sessions. Hypertension . 2005;45:811–7.
Stidley CA, Hunt WC, Tentori F, Schmidt D, Rohrscheib M, Paine S, et al. Changing relationship of blood pressure with mortality over time among hemodialysis patients. J Am Soc Nephrol. 2006;17:513–20.
Myers OB, Adams C, Rohrscheib MR, Servilla KS, Miskulin D, Bedrick EJ, et al. Age, race, diabetes, blood pressure, and mortality among hemodialysis patients. J Am Soc Nephrol. 2010;21:1970–8.
Bansal N, McCulloch CE, Rahman M, Kusek JW, Anderson AH, Xie D, et al. Blood pressure and risk of all-cause mortality in advanced chronic kidney disease and hemodialysis: the chronic renal insufficiency cohort study. Hypertension. 2015;65:93–100.
Shafi T, Zager PG, Sozio SM, Grams ME, Jaar BG, Christenson RH, et al. Troponin I and NT-proBNP and the association of systolic blood pressure with outcomes in incident hemodialysis patients: the Choices for Healthy Outcomes in Caring for ESRD (CHOICE) Study. Am J Kidney Dis. 2014;64:443–51.
Agarwal R. Hypertension and survival in chronic hemodialysis patients—past lessons and future opportunities. Kidney Int. 2005;67:1–13.
Chang TI. Systolic blood pressure and mortality in patients on hemodialysis. Curr Hypertens Rep. 2011;13:362–9.
Khan YH, Sarriff A, Adnan AS, Khan AH, Mallhi TH. Blood pressure and mortality in hemodialysis patients: a systematic review of an ongoing debate. Ther Apher Dial. 2016;20:453–61.
Georgianos PI, Agarwal R. Blood pressure and mortality in long-term hemodialysis-time to move forward. Am J Hypertens. 2017;30:211–22.
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–12.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 10 Mar 2017.
Greenland S, Longnecker MP. Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol. 1992;135:1301–9.
Orsini N, Li R, Wolk A, Khudyakov P, Spiegelman D. Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol. 2012;175:66–73.
Desquilbet L, Mariotti F. Dose-response analyses using restricted cubic spline functions in public health research. Stat Med. 2010;29:1037–57.
Aune D, Saugstad OD, Henriksen T, Tonstad S. Maternal body mass index and the risk of fetal death, stillbirth, and infant death: a systematic review and meta-analysis. JAMA. 2014;311:1536–46.
Wang X, Ouyang Y, Liu J, Zhu M, Zhao G, Bao W, et al. Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: systematic review and dose-response meta-analysis of prospective cohort studies. BMJ. 2014;349:g4490.
K/DOQI Workgroup. K/DOQI clinical practice guidelines for cardiovascular disease in dialysis patients. Am J Kidney Dis. 2005;45:S1–153.
Bekkering GE, Harris RJ, Thomas S, Mayer AM, Beynon R, Ness AR, et al. How much of the data published in observational studies of the association between diet and prostate or bladder cancer is usable for meta-analysis? Am J Epidemiol. 2008;167:1017–26.
Berlin JA, Longnecker MP, Greenland S. Meta-analysis of epidemiologic doseresponse data. Epidemiology. 1993;4:218–28.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Muggeo VM. Estimating regression models with unknown break-points. Stat Med. 2003;22:3055–71.
Muggeo VM. Segmented: an R package to fit regression models with broken-line relationships. R News. 2008;8:20–25.
Saran R, Bragg-Gresham JL, Rayner HC, Goodkin DA, Keen ML, Van Dijk PC, et al. Nonadherence in hemodialysis: associations with mortality, hospitalization, and practice patterns in the DOPPS. Kidney Int. 2003;64:254–62.
Agarwal R. Hypervolemia is associated with increased mortality among hemodialysis patients. Hypertension. 2010;56:512–7.
Chazot C, Wabel P, Chamney P, Moissl U, Wieskotten S, Wizemann V. Importance of normohydration for the long-term survival of haemodialysis patients. Nephrol Dial Transplant. 2012;27:2404–10.
Crippa A, Orsini N. Multivariate dose-response meta-analysis: the dosresmeta R package. J Stat Softw. 2016;72:1–15.
Core Team RR: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2015.
Foley RN, Herzog CA, Collins AJ. United States renal data system. Blood pressure and long-term mortality in United States hemodialysis patients: USRDS Waves 3 and 4 Study. Kidney Int. 2002;62:1784–90.
Li Z, Lacson E Jr, Lowrie EG, Ofsthun NJ, Kuhlmann MK, et al. The epidemiology of systolic blood pressure and death risk in hemodialysis patients. Am J Kidney Dis. 2006;48:606–15.
Molnar MZ, Lukowsky LR, Streja E, Dukkipati R, Jing J, Nissenson AR, et al. Blood pressure and survival in longterm hemodialysis patients with and without polycystic kidney disease. J Hypertens. 2010;28:2475–84.
Chang TI, Friedman GD, Cheung AK, Greene T, Desai M, Chertow GM. Systolic blood pressure and mortality in prevalent haemodialysis patients in the HEMO study. J Hum Hypertens. 2011;25:98–105.
Robinson BM, Tong L, Zhang J, Wolfe RA, Goodkin DA, Greenwood RN, et al. Blood pressure levels and mortality risk among hemodialysis patients in the Dialysis Outcomes and Practice Patterns Study. Kidney Int. 2012;82:570–80.
Inaba M, Karaboyas A, Akiba T, Akizawa T, Saito A, Fukuhara S, et al. Association of blood pressure with all-cause mortality and stroke in Japanese hemodialysis patients: the Japan Dialysis Outcomes and Practice Pattern Study. Hemodial Int. 2014;18:607–15.
Foley RN. Cardiac disease in chronic uremia: can it explain the reverse epidemiology of hypertension and survival in dialysis patients? Semin Dial. 2004;17:275–8.
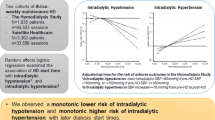
Agarwal R, Light R. Intradialytic hypertension is a marker of volume excess. Nephrol Dial Transplant. 2010;25:3355–61.
Hannedouche T, Roth H, Krummel T, London GM, Jean G, Bouchet JL, et al. Multiphasic effects of blood pressure on survival in hemodialysis patients. Kidney Int. 2016;90:674–84.
Wanner C, Amann K, Shoji T. The heart and vascular system in dialysis. Lancet. 2016;388:276–84.
Agarwal R, Sinha AD. Cardiovascular protection with antihypertensive drugs in dialysis patients: systematic review and meta-analysis. Hypertension. 2009;53:860–6.
Heerspink HJ, Ninomiya T, Zoungas S, de Zeeuw D, Grobbee DE, Jardine MJ, et al. Effect of lowering blood pressure on cardiovascular events and mortality in patients on dialysis: a systematic review and meta-analysis of randomised controlled trials. Lancet. 2009;373:1009–15.
Zoccali C, Moissl U, Chazot C, Mallamaci F, Tripepi G, Arkossy O, et al. Chronic Fluid Overload and Mortality in ESRD. J Am Soc Nephrol. 2017;28:2491–7.
Miskulin DC, Gassman J, Schrader R, Gul A, Jhamb M, Ploth DW, et al. BP in dialysis: results of a pilot study. J Am Soc Nephrol. 2018;29:307–16.
Acknowledgements
This study was supported by grants to Bi-Cheng Liu from Clinic Research Center program of Jiangsu Province (BL2014080).
Code availability
The R code used to generate results can be accessed by contacting Yu-Chen Han (njhanyuchen@163.com).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Han, YC., Tu, Y., Zhou, LT. et al. Peridialysis BP levels and risk of all-cause mortality: a dose-response meta-analysis. J Hum Hypertens 33, 41–49 (2019). https://doi.org/10.1038/s41371-018-0103-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-018-0103-9
This article is cited by
-
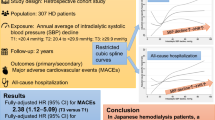
Intradialytic systolic blood pressure variation can predict long-term mortality in patients on maintenance hemodialysis
International Urology and Nephrology (2021)