Abstract
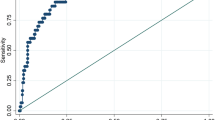
Blood pressure-to-height ratio (BPHR) has been reported to perform well for identifying hypertension (HTN) in adolescents but not in young children. Our study was aimed to evaluate the performance of BPHR and modified BPHR (MBPHR) for screening HTN in children. A total of 5268 Chinese children (boys: 53.1%) aged 6–12 years and 5024 American children (boys: 48.1%) aged 8–12 years were included in the present study. BPHR was calculated as BP/height (mmHg/cm). MBPHR7 was calculated as BP/(height + 7*(13-age)). MBPHR3 was calculated as BP/(height + 3*(13-age)). We used receiver-operating characteristic curve analysis to assess the performance of the three ratios for identifying HTN in children as compared to the 2017 U.S. clinical guideline as the “gold standard”. The prevalence of HTN in Chinese and American children was 9.4% and 5.4%, respectively, based on the 2017 U.S. guideline. The AUC was larger for MBPHR3 than BPHR and MBPHR7. All three ratios had optimal negative predictive value (~100%). The positive predictive value (PPV) was higher for MBPHR3 than BPHR in both Chinese (43.9% vs. 37.9%) and American (39.1% vs. 26.3%) children. In contrast, the PPV was higher for MBPHR7 than BPHR in Chinese children (47.4% vs. 37.9%) but not in American children (24.8% vs. 26.3%). In summary, MBPHR3 overall performed better than MBPHR7 and BPHR for identifying HTN in children. However, the three ratios had low PPV (<50%) as compared to the 2017 U.S. guidelines, which makes these ratios of limited use for HTN screening in children.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Xi B, Bovet P, Hong YM, Zong X, Chiolero A, Kim HS, et al. Recent blood pressure trends in adolescents from China, Korea, Seychelles and the United States of America, 1997-2012. J Hypertens. 2016;34:1948–58.
Kit BK, Kuklina E, Carroll MD, Ostchega Y, Freedman DS, Ogden CL. Prevalence of and trends in dyslipidemia and blood pressure among US children and adolescents, 1999-2012. JAMA Pediatr. 2015;169:272–9.
Chen X, Wang Y. Tracking of blood pressure from childhood to adulthood: a systematic review and meta-regression analysis. Circulation. 2008;117:3171–80.
Kollias A, Dafni M, Poulidakis E, Ntineri A, Stergiou GS. Out-of-office blood pressure and target organ damage in children and adolescents: a systematic review and meta-analysis. J Hypertens. 2014;32:2315–31.
Gray L, Lee IM, Sesso HD, Batty GD. Blood pressure in early adulthood, hypertension in middle age, and future cardiovascular disease mortality: HAHS (Harvard Alumni Health Study). J Am Coll Cardiol. 2011;58:2396–403.
Sundstrom J, Neovius M, Tynelius P, Rasmussen F. Association of blood pressure in late adolescence with subsequent mortality: cohort study of Swedish male conscripts. BMJ. 2011;342:d643.
Flynn JT, Kaelber DC, Baker-Smith CM, Blowey D, Carroll AE, Daniels SR, et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics. 2017;140:e20171904.
Lu Q, Ma CM, Yin FZ, Liu BW, Lou DH, Liu XL. How to simplify the diagnostic criteria of hypertension in adolescents. J Hum Hypertens. 2011;25:159–63.
Kelishadi R, Heshmat R, Ardalan G, Qorbani M, Taslimi M, Poursafa P, et al. First report on simplified diagnostic criteria for pre-hypertension and hypertension in a national sample of adolescents from the Middle East and North Africa: the CASPIAN-III study. J Pediatr. 2014;90:85–91.
Xi B, Zhang M, Zhang T, Li S, Steffen LM. Simplification of childhood hypertension definition using blood pressure to height ratio among US youths aged 8-17years, NHANES 1999-2012. Int J Cardiol. 2015;180:210–3.
Galescu O, George M, Basetty S, Predescu I, Mongia A, Ten S, et al. Blood pressure over height ratios: simple and accurate method of detecting elevated blood pressure in children. Int J Pediatr. 2012;2012:253497.
Rabbia F, Rabbone I, Totaro S, Testa E, Covella M, Berra E, et al. Evaluation of blood pressure/height ratio as an index to simplify diagnostic criteria of hypertension in Caucasian adolescents. J Hum Hypertens. 2011;25:623–4.
Ahmed A, Ali SW, Massodi S, Bhat MA. Blood pressure-to-height ratio as a screening tool for hypertension in children. Indian Pediatr. 2016;53:137–9.
Xi B, Zhang M, Zhang T, Liang Y, Li S, Steffen LM. Hypertension screening using blood pressure to height ratio. Pediatrics. 2014;134:e106–111.
Guo X, Zheng L, Li Y, Zhang X, Yu S, Sun Y. Blood pressure to height ratio: a novel method for detecting hypertension in paediatric age groups. Paediatr Child Health. 2013;18:65–69.
Mourato FA, Nadruz W Jr, Moser LR, de Lima Filho JL, Mattos SS. A modified blood pressure to height ratio improves accuracy for hypertension in childhood. Am J Hypertens. 2015;28:409–13.
Ma C, Lu Q, Yin F. The performance of modified blood pressure-to-height ratio as a screening measure for identifying children with hypertension. Clin Exp Hypertens. 2016;38:155–9.
Dong B, Wang Z, Wang HJ, Ma J. Improving hypertension screening in childhood using modified blood pressure to height ratio. J Clin Hypertens. 2016;18:557–64.
Ma C, Lu Q, Wang R, Liu X, Lou D, Yin F. A new modified blood pressure-to-height ratio simplifies the screening of hypertension in Han Chinese children. Hypertens Res. 2016;39:893–8.
Popkin BM, Du S, Zhai F, Zhang B. Cohort profile: The China Health and Nutrition Survey--monitoring and understanding socio-economic and health change in China, 1989-2011. Int J Epidemiol. 2010;39:1435–40.
National Center for Health Statistics, Centers for Disease Control and Prevention: National health and nutrition examination survey. https://www.cdc.gov/nchs/nhanes/ (2017).
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–3.
Zou KH, O’Malley AJ, Mauri L. Receiver-operating characteristic analysis for evaluating diagnostic tests and predictive models. Circulation. 2007;115:654–7.
Youngstrom EA. A primer on receiver operating characteristic analysis and diagnostic efficiency statistics for pediatric psychology: we are ready to ROC. J Pediatr Psychol. 2014;39:204–21.
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(2 Suppl 4th Report):555–76.
Somu S, Sundaram B, Kamalanathan AN. Early detection of hypertension in general practice. Arch Dis Child. 2003;88:302.
Chiolero A, Paradis G, Simonetti GD, Bovet P. Absolute height-specific thresholds to identify elevated blood pressure in children. J Hypertens. 2013;31:1170–4.
Mitchell CK, Theriot JA, Sayat JG, Muchant DG, Franco SM. A simplified table improves the recognition of paediatric hypertension. J Paediatr Child Health. 2011;47:22–26.
Kaelber DC, Pickett F. Simple table to identify children and adolescents needing further evaluation of blood pressure. Pediatrics. 2009;123:e972–974.
Ma C, Kelishadi R, Hong YM, Bovet P, Khadilkar A, Nawarycz T, et al. Performance of eleven simplified methods for the identification of elevated blood pressure in children and adolescents. Hypertension. 2016;68:614–20.
Koebnick C, Black MH, Wu J, Martinez MP, Smith N, Kuizon B, et al. High blood pressure in overweight and obese youth: implications for screening. J Clin Hypertens. 2013;15:793–805.
Falkner B, Gidding SS, Ramirez-Garnica G, Wiltrout SA, West D, Rappaport EB. The relationship of body mass index and blood pressure in primary care pediatric patients. J Pediatr. 2006;148:195–200.
Sun J, Steffen LM, Ma C, Liang Y, Xi B. Definition of pediatric hypertension: are blood pressure measurements on three separate occasions necessary? Hypertens Res. 2017;40:496–503.
Acknowledgements
The study was supported by the National Nature Science Foundation of China (81673195).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Zhang, Y., Ma, C., Yang, L. et al. Performance of modified blood pressure-to-height ratio for identifying hypertension in Chinese and American children. J Hum Hypertens 32, 408–414 (2018). https://doi.org/10.1038/s41371-018-0056-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41371-018-0056-z
This article is cited by
-
A new simple formula built on the American Academy of Pediatrics criteria for the screening of hypertension in overweight/obese children
European Journal of Pediatrics (2019)