Abstract
Background
Residential mobility can introduce exposure misclassification in pediatric epidemiology studies using birth address only.
Objective
We examined whether residential mobility varies by sociodemographic factors and urbanicity/rurality among children with cancer.
Methods
Our study included 400 children born in Pennsylvania during 2002–2015 and diagnosed with leukemia at ages 2–7 years. Addresses were obtained from state registries at birth and diagnosis. We considered three aspects of mobility between birth and diagnosis: whether a child moved, whether a mover changed census tract, and distance moved. We evaluated predictors of these aspects in urban- and rural-born children using chi-square, t-tests, and regression analyses.
Results
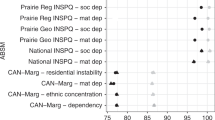
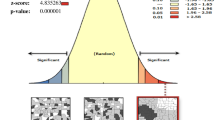
Overall, 58% of children moved between birth and diagnosis; suburban/rural-born children were more likely to move than urban-born children (67% versus 57%). The mean distance moved was 16.7 km in suburban/rural-born and 14.8 km in urban-born movers. In urban-born children, moving between birth and diagnosis was associated with race, education, participation in the Nutrition Program for Women, Infants and Children (WIC), and census tract-level income (all χ2 p < 0.01). Urban-born movers tended to be born in a census tract with a higher Social Vulnerability Index than non-movers (t-test p < 0.01). No factors were statistically significantly associated with any of the residential mobility metrics in suburban/rural-born children, although the sample size was small.
Impact Statement
In this study of a vulnerable population of children with cancer, we found that rural-born children were more likely to move than urban-born children, however, the frequency of movers changing census tracts was equivalent. Mobility in urban-born children, but not rural-born, was associated with several social factors, although the sample size for rural-born children was small. Mobility could be an important source of misclassification depending on the spatial heterogeneity and resolution of the exposure data and whether the social factors are related to exposures or health outcomes. Our results highlight the importance of considering differences in mobility between urban and rural populations in spatial research.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Data for this study were obtained from the Pennsylvania Cancer Registry and the Pennsylvania Department of Health Bureau of Health Statistics and Registries. The authors do not own these data and are not permitted to share them.
References
Bell ML, Banerjee G, Pereira G. Residential mobility of pregnant women and implications for assessment of spatially-varying environmental exposures. J Expo Sci Environ Epidemiol. 2018;28:470–80.
Bell ML, Belanger K. Review of research on residential mobility during pregnancy: consequences for assessment of prenatal environmental exposures. J Expo Sci Environ Epidemiol. 2012;22:429–38.
Hodgson S, Lurz PW, Shirley MD, Bythell M, Rankin J. Exposure misclassification due to residential mobility during pregnancy. Int J Hyg Environ Health. 2015;218:414–21.
Ling C, Heck JE, Cockburn M, Liew Z, Marcotte E, Ritz B. Residential mobility in early childhood and the impact on misclassification in pesticide exposures. Environ Res. 2019;173:212–20.
Urayama KY, Von Behren J, Reynolds P, Hertz A, Does M, Buffler PA. Factors Associated With Residential Mobility in Children With Leukemia: Implications For Assigning Exposures. Ann Epidemiol. 2009;19:834–40.
Barrington-Trimis JL, Cockburn M, Metayer C, Gauderman WJ, Wiemels J, McKean-Cowdin R. Trends in childhood leukemia incidence over two decades from 1992 to 2013. Int J Cancer. 2017;140:1000–8.
Poole C, Greenland S, Luetters C, Kelsey JL, Mezei G. Socioeconomic status and childhood leukaemia: a review. Int J Epidemiol. 2006;35:370–84.
Brokamp C, LeMasters GK, Ryan PH. Residential mobility impacts exposure assessment and community socioeconomic characteristics in longitudinal epidemiology studies. J Expo Sci Environ Epidemiol. 2016;26:428–34.
Tee Lewis PG, Chen T-Y, Chan W, Symanski E. Predictors of residential mobility and its impact on air pollution exposure among children diagnosed with early childhood leukemia. J Expo Sci Environ Epidemiol. 2019;29:510–9.
Canfield MA, Ramadhani TA, Langlois PH, Waller DK. Residential mobility patterns and exposure misclassification in epidemiologic studies of birth defects. J Expo Sci Environ Epidemiol. 2006;16:538–43.
Saucy A, Gehring U, Olmos S, Delpierre C, de Bont J, Gruzieva O, et al. Effect of residential relocation on environmental exposures in European cohorts: An exposome-wide approach. Environ Int. 2023;173:107849.
Bennett EE, Lynch KM, Xu X, Park ES, Ying Q, Wei J, et al. Characteristics of movers and predictors of residential mobility in the Atherosclerosis Risk in Communities (ARIC) cohort. Health Place. 2022;74:102771.
South SJ, Deane GD. Race and Residential Mobility: Individual Determinants and Structural Constraints. Soc Forces. 1993;72:147–67.
James WL. All Rural Places Are Not Created Equal: Revisiting the Rural Mortality Penalty in the United States. Am J Public Health. 2014;104:2122–9.
Cosby AG, Neaves TT, Cossman RE, Cossman JS, James WL, Feierabend N, et al. Preliminary Evidence for an Emerging Nonmetropolitan Mortality Penalty in the United States. Am J Public Health. 2008;98:1470–2.
Cossman JS, James WL, Cosby AG, Cossman RE. Underlying Causes of the Emerging Nonmetropolitan Mortality Penalty. Am J Public Health. 2010;100:1417–9.
Haines MR. The urban mortality transition in the united states, 1800-1940. Annales de démographie historique. 2001;101:33–64.
Pampel FC, Rogers RG. Socioeconomic Status, Smoking, and Health: A Test of Competing Theories of Cumulative Advantage. J Health Soc Behav. 2004;45:306–21.
Cockerham WC. Health Lifestyle Theory and the Convergence of Agency and Structure. J Health Soc Behav. 2005;46:51–67.
Hartley D. Rural Health Disparities, Population Health, and Rural Culture. Am J Public Health. 2004;94:1675–8.
Adler NE, Boyce, T, Chesney, MA, Cohen, S, Folkman, S, Kahn, et al. Socioeconomic status and health: The challenge of the gradient. Am Psychol. 1994;49:15–24.
Clark CJ, Johnson NP, Soriano M, Warren JL, Sorrentino KM, Kadan-Lottick NS, et al. Unconventional Oil and Gas Development Exposure and Risk of Childhood Acute Lymphoblastic Leukemia: A Case & Control Study in Pennsylvania, 2009-2017. Environ Health Perspect. 2022;130:087001.
Doerrenberg M, Kloetgen A, Hezaveh K, Wössmann W, Bleckmann K, Stanulla M, et al. T-cell acute lymphoblastic leukemia in infants has distinct genetic and epigenetic features compared to childhood cases. Genes, Chromosomes Cancer 2017;56:159–67.
Wiemels J. Chromosomal translocations in childhood leukemia: natural history, mechanisms, and epidemiology. J Natl Cancer Inst Monogr. 2008;39:87–90.
United States Census Bureau. 2000-2010. https://data.census.gov/cedsci/.
Agency for Toxic Substances and Disease Registry (ATSDR). The social vulnerability index 2021. https://www.atsdr.cdc.gov/placeandhealth/svi/index.html.
United States Department of Agriculture ERS. Rural-Urban Commuting Area Codes. 2020. https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx.
Salvati L. Residential mobility and the local context: Comparing long-term and short-term spatial trends of population movements in Greece. Socio-Econ Plan Sci 2020;72:100910.
Pui C-H. Acute Lymphoblastic Leukemia. In: Schwab M, editor. Encyclopedia of Cancer. Berlin, Heidelberg: Springer Berlin Heidelberg; 2011. p. 23-6.
Acknowledgements
This research was supported in part by National Priority Research Project under Assistance Agreement No. CR839249 awarded by the U.S. Environmental Protection Agency (EPA) to Yale University. The publication has not been formally reviewed by EPA. The views expressed in this document are solely those of the authors and do not reflect those of the Agency. EPA does not endorse any products or commercial services mentioned in this publication. Research reported in this publication was supported in part by the National Institute On Minority Health And Health Disparities of the National Institutes of Health under Award Number R01MD016054. CJC was supported by a T32 training grant from the National Cancer Institute (T32 CA250803). The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health. Some data were supplied by the Bureau of Health Statistics & Registries, Pennsylvania Department of Health, Harrisburg, Pennsylvania. The Pennsylvania Department of Health specifically disclaims responsibility for any analyses, interpretations or conclusions.
Author information
Authors and Affiliations
Contributions
CJC: Conceptualization, funding acquisition, formal analysis, visualization, writing—original draft and review and editing; JLW: Conceptualization, methodology, writing: review and editing, MLB: Methodology, writing: review and editing, JES: Writing: review and editing, funding acquisition, XM: Supervision, writing: review and editing, funding acquisition, and NCD: Conceptualization, supervision, writing—review and editing, funding acquisition.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study protocol was approved by the Institutional Review Board of Yale University (HIC #2000021809) and the Pennsylvania Department of Health (IF-0430) and reviewed and approved by the US Environmental Protection Agency (HSR-001162).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Clark, C.J., Warren, J.L., Saiers, J.E. et al. Predictors of early life residential mobility in urban and rural Pennsylvania children with acute lymphoblastic leukemia and implications for environmental exposure assessment. J Expo Sci Environ Epidemiol (2023). https://doi.org/10.1038/s41370-023-00636-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41370-023-00636-9