Abstract
Background
Tobacco smoke exposure (TSE) through secondhand and thirdhand smoke is a modifiable risk factor that contributes to childhood morbidity. Limited research has assessed surface TSE pollution in children’s environments as a potential source of thirdhand smoke exposure, and none have examined levels of the tobacco-specific nitrosamine 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK) on surfaces.
Objective
This study measured surface NNK and nicotine in children’s homes and associations with sociodemographics and parent-reported TSE behaviors. We assessed correlations of surface NNK and nicotine with dust NNK, dust nicotine, and child cotinine.
Methods
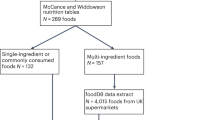
Home surface wipe NNK and nicotine data from 84 children who lived with smokers were analyzed. Tobit and simple linear regression analyses were conducted to assess associations of surface NNK and nicotine with child characteristics. Spearman’s (ρ) correlations assessed the strength of associations between environmental markers and child cotinine.
Results
Nearly half (48.8%) of children’s home surfaces had detectable NNK and 100% had detectable nicotine. The respective geometric means (GMs) of surface NNK and nicotine loadings were 14.0 ng/m2 and 16.4 µg/m2. Surface NNK positively correlated with surface nicotine (ρ = 0.54, p < 0.001) and dust NNK (ρ = 0.30, p = 0.020). Surface nicotine positively correlated with dust NNK (ρ = 0.42, p < 0.001) and dust nicotine (ρ = 0.24, p = 0.041). Children with household incomes ≤$15,000 had higher surface NNK levels (GM = 18.7 ng/m2, p = 0.017) compared to children with household incomes >$15,000 (GM = 7.1 ng/m2). Children with no home smoking bans had higher surface NNK (GM = 18.1 ng/m2, p = 0.020) and surface nicotine (GM = 17.7 µg/m2, p = 0.019) levels compared to children with smoking bans (GM = 7.5 ng/m2, 4.8 µg/m2, respectively).
Impact
Although nicotine on surfaces is an established marker of thirdhand smoke pollution, other thirdhand smoke contaminants have not been measured on surfaces in the homes of children living with smokers. We provide evidence that the potent carcinogenic tobacco-specific nitrosamine NNK was detectable on surfaces in nearly half of children’s homes, and nicotine was detectable on all surfaces. Surface NNK was positively correlated with surface nicotine and dust NNK. Detectable surface NNK levels were found in homes with indoor smoking bans, indicating the role of NNK as a persistent thirdhand smoke pollutant accumulating on surfaces as well as in dust.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Data cannot be shared publicly because of potentially identifying patient information. Data are available from Cincinnati Children’s Hospital Medical Center (contact Dr. Melinda Mahabee-Gittens via melinda.mahabee-gittens@cchmc.org) for researchers who meet the criteria for access to confidential data.
References
U.S. Department of Health and Human Services. The health consequences of involuntary exposure to tobacco smoke: a report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2006.
Rodgman A, Perfetti TA. The chemical components of tobacco and tobacco smoke. 2nd ed. Boca Raton, FL: CRC Press; 2012.
International Agency for Research on Cancer (IARC) Working Group on the Evaluation of Carcinogenic Risks to Humans. A review of human carcinogens. Lyon, France: IARC. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, no. 100B; 2012.
IARC Working Group on the Evaluation of Carcinogenic Risks to Humans. Tobacco smoke and involuntary smoking. Lyon, France: IARC. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, no. 83; 2004.
Matt GE, Quintana PJE, Destaillats H, Gundel LA, Sleiman M, Singer BC, et al. Thirdhand tobacco smoke: emerging evidence and arguments for a multidisciplinary research agenda. Environ Health Perspect. 2011;119:1218–26. https://doi.org/10.1289/ehp.1103500.
Jacob P 3rd, Benowitz NL, Destaillats H, Gundel L, Hang B, Martins-Green M, et al. Thirdhand smoke: new evidence, challenges, and future directions. Chem Res. Toxicol. 2017;30:270–94. https://doi.org/10.1021/acs.chemrestox.6b00343.
Sleiman M, Gundel LA, Pankow JF, Jacob P 3rd, Singer BC, Destaillats H. Formation of carcinogens indoors by surface-mediated reactions of nicotine with nitrous acid, leading to potential thirdhand smoke hazards. Proc Natl Acad Sci USA. 2010;107:6576–81. https://doi.org/10.1073/pnas.0912820107.
Matt GE, Quintana PJE, Hovell MF, Bernert JT, Song S, Novianti N, et al. Households contaminated by environmental tobacco smoke: sources of infant exposures. Tob Control. 2004;13:29–37. https://doi.org/10.1136/tc.2003.003889.
World Health Organization. WHO summary of principles for evaluating health risks in children associated with exposure to chemicals. Geneva, Switzerland: World Health Organization; 2011.
Mahabee-Gittens EM, Merianos AL, Hoh E, Quintana PJE, Matt GE. Nicotine on children’s hands: limited protection of smoking bans and initial clinical findings. Tob Use Insights. 2019;12:1179173X18823493 https://doi.org/10.1177/1179173X18823493.
Ferguson A, Penney R, Solo-Gabriele H. A review of the field on children’s exposure to environmental contaminants: a risk assessment approach. Int J Environ Res Public Health. 2017;14:265 https://doi.org/10.3390/ijerph14030265.
Xue J, Zartarian V, Tulve N, Moya J, Freeman N, Auyeung W, et al. A meta-analysis of children’s object-to-mouth frequency data for estimating non-dietary ingestion exposure. J Expo Sci Environ Epidemiol. 2009;20:536–45. https://doi.org/10.1038/jes.2009.42.
Roberts JW, Wallace LA, Camann DE, Dickey P, Gilbert SG, Lewis RG, et al. Monitoring and reducing exposure of infants to pollutants in house dust. Rev Environ Contam Toxicol. 2009;201:1–39. https://doi.org/10.1007/978-1-4419-0032-6_1.
Hein HO, Suadicani P, Skov P, Gyntelberg F. Indoor dust exposure: an unnoticed aspect of involuntary smoking. Arch Environ Health. 1991;46:98–101. https://doi.org/10.1080/00039896.1991.9937435.
Kim S, Aung T, Berkeley E, Diette GB, Breysse PN. Measurement of nicotine in household dust. Environ Res. 2008;108:289–93. https://doi.org/10.1016/j.envres.2008.07.004.
Matt GE, Quintana PJE, Hoh E, Zakarian JM, Chowdhury Z, Hovell MF, et al. A casino goes smoke free: a longitudinal study of secondhand and thirdhand smoke pollution and exposure. Tob Control. 2018;27:643–9. https://doi.org/10.1136/tobaccocontrol-2017-054052.
Matt GE, Quintana PJE, Zakarian JM, Fortmann AL, Chatfield DA, Hoh E, et al. When smokers move out and non-smokers move in: residential thirdhand smoke pollution and exposure. Tob Control. 2011;20:e1 https://doi.org/10.1136/tc.2010.037382.
Whitehead TP, Havel C, Metayer C, Benowitz NL, Jacob P. 3rd. Tobacco alkaloids and tobacco-specific nitrosamines in dust from homes of smokeless tobacco users, active smokers, and non-tobacco users. Chem Res Toxicol. 2015;28:1007–14. https://doi.org/10.1021/acs.chemrestox.5b00040.
Ramírez N, Özel MZ, Lewis AC, Marcé RM, Borrull F, Hamilton JF. Determination of nicotine and N-nitrosamines in house dust by pressurized liquid extraction and comprehensive gas chromatography—Nitrogen chemiluminiscence detection. J Chromatogr A. 2012;1219:180–7. https://doi.org/10.1016/j.chroma.2011.11.017.
Sleiman M, Logue JM, Luo W, Pankow JF, Gundel LA, Destaillats H. Inhalable constituents of thirdhand tobacco smoke: chemical characterization and health impact considerations. Environ Sci Technol. 2014;48:13093–101. https://doi.org/10.1021/es5036333.
Hoh E, Hunt RN, Quintana PJE, Zakarian JM, Chatfield DA, Wittry BC, et al. Environmental tobacco smoke as a source of polycyclic aromatic hydrocarbons in settled household dust. Environ Sci Technol. 2012;46:4174–83. https://doi.org/10.1021/es300267g.
Northrup TF, Matt GE, Hovell MF, Khan AM, Stotts AL. Thirdhand smoke in the homes of medically fragile children: assessing the impact of indoor smoking levels and smoking bans. Nicotine Tob Res. 2016;18:1290–8. https://doi.org/10.1093/ntr/ntv174.
Thomas JL, Guo H, Carmella SG, Balbo S, Han S, Davis A, et al. Metabolites of a tobacco-specific lung carcinogen in children exposed to secondhand or thirdhand tobacco smoke in their homes. Cancer Epidemiol Biomark Prev. 2011;20:1213–21. https://doi.org/10.1158/1055-9965.EPI-10-1027.
Schick SF, Farraro KF, Perrino C, Sleiman M, van de Vossenberg G, Trinh MP, et al. Thirdhand cigarette smoke in an experimental chamber: evidence of surface deposition of nicotine, nitrosamines and polycyclic aromatic hydrocarbons and de novo formation of NNK. Tob Control. 2014;23:152–9. https://doi.org/10.1136/tobaccocontrol-2012-050915.
Quintana PJE, Matt GE, Chatfield D, Zakarian JM, Fortmann AL, Hoh E. Wipe sampling for nicotine as a marker of thirdhand tobacco smoke contamination on surfaces in homes, cars, and hotels. Nicotine Tob Res. 2013;15:1555–63. https://doi.org/10.1093/ntr/ntt014.
Hood NE, Ferketich AK, Klein EG, Pirie P, Wewers ME. Associations between self-reported in-home smoking behaviours and surface nicotine concentrations in multiunit subsidised housing. Tob Control. 2014;23:27–32. https://doi.org/10.1136/tobaccocontrol-2012-050666.
Kassem NOF, Daffa RM, Liles S, Jackson SR, Kassem NO, Younis MA, et al. Children’s exposure to secondhand and thirdhand smoke carcinogens and toxicants in homes of hookah smokers. Nicotine Tob Res. 2014;16:961–75. https://doi.org/10.1093/ntr/ntu016.
Ge G, Xu T, Chen C. Tobacco carcinogen NNK-induced lung cancer animal models and associated carcinogenic mechanisms. Acta Biochim Biophys Sin. 2015;47:477–87. https://doi.org/10.1093/abbs/gmv041.
Akopyan G, Bonavida B. Understanding tobacco smoke carcinogen NNK and lung tumorigenesis (review). Int J Oncol. 2006;29:745–52. https://doi.org/10.1093/abbs/gmv041.
Aquilina NJ, Havel CM, Benowitz NL, Jacob P 3rd. Tobacco-specific and combustion pollutants in settled house dust in Malta. J Environ Expo Assess. 2022;1:7 https://doi.org/10.20517/jeea.2021.09.
Matt GE, Quintana PJE, Zakarian JM, Hoh E, Hovell MF, Mahabee-Gittens EM, et al. When smokers quit: exposure to nicotine and carcinogens persists from thirdhand smoke pollution. Tob Control. 2016;26:548–56. https://doi.org/10.1136/tobaccocontrol-2016-053119.
Ramírez N, Özel MZ, Lewis AC, Marcé RM, Borrull F, Hamilton JF. Exposure to nitrosamines in thirdhand tobacco smoke increases cancer risk in non-smokers. Environ Int. 2014;71:139–47. https://doi.org/10.1016/j.envint.2014.06.012.
Thomas JL, Hecht SS, Luo X, Ming X, Ahluwalia JS, Carmella SG. Thirdhand tobacco smoke: A tobacco-specific lung carcinogen on surfaces in smokers’ homes. Nicotine Tob Res. 2014;16:26–32. https://doi.org/10.1093/ntr/ntt110.
Tang X, Benowitz N, Gundel L, Hang B, Havel CM, Hoh E, et al. Thirdhand exposures to tobacco-specific nitrosamines through inhalation, dust ingestion, dermal uptake, and epidermal chemistry. Environ Sci Technol. 2022;56:12506–16. https://doi.org/10.1021/acs.est.2c02559.
Mahabee-Gittens EM, Ammerman RT, Khoury JC, Stone L, Meyers GT, Witry JK, et al. Healthy families: study protocol for a randomized controlled trial of screening, brief intervention, and referral to treatment intervention for caregivers to reduce secondhand smoke exposure among pediatric emergency department patients. BMC Public Health. 2017;17:374–87. https://doi.org/10.1186/s12889-017-4278-8.
Mahabee-Gittens EM, Matt GE, Hoh E, Quintana PJE, Stone L, Geraci MA, et al. Contribution of thirdhand smoke to overall tobacco smoke exposure in pediatric patients: study protocol. BMC Public Health. 2019;19:491 https://doi.org/10.1186/s12889-019-6829-7.
Matt GE, Quintana PJE, Hoh E, Zakarian JM, Dodder NG, Record RA, et al. Remediating thirdhand smoke pollution in multiunit housing: temporary reductions and the challenges of persistent reservoirs. Nicotine Tob Res. 2021;23:364–72. https://doi.org/10.1093/ntr/ntaa151.
Jacob P 3rd, Yu L, Duan M, Ramos L, Yturralde O, Benowitz NL. Determination of the nicotine metabolites cotinine and trans-3′-hydroxycotinine in biologic fluids of smokers and non-smokers using liquid chromatography–tandem mass spectrometry: biomarkers for tobacco smoke exposure and for phenotyping cytochrome P450 2A6 activity. J Chromatogr B Anal Technol Biomed Life Sci. 2011;879:267–76. https://doi.org/10.1016/j.jchromb.2010.12.012.
R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2013. http://www.R-project.org/.
United States Environmental Protection Agency. Exposure factors handbook: 2011 edition (final report). EPA/600/R-09/052F ed. Washington, DC: National Center for Environmental Assessment; 2011.
National Center for Biotechnology Information. PubChem compound summary for CID 47289, 4-(N-Nitrosomethylamino)-1-(3-pyridyl)-1-butanone. 2023. https://pubchem.ncbi.nlm.nih.gov/compound/4-_N-Nitrosomethylamino-1-3-pyridyl-1-butanone.
National Center for Biotechnology Information. PubChem compound summary for CID 89594, nicotine. 2023. https://pubchem.ncbi.nlm.nih.gov/compound/Nicotine.
Benowitz NL, Bernert JT, Foulds J, Hecht SS, Jacob P 3rd, Jarvis MJ, et al. Biochemical verification of tobacco use and abstinence: 2019 update. Nicotine Tob Res. 2020;22:1086–97. https://doi.org/10.1093/ntr/ntz132.
Xue J, Yang S, Seng S. Mechanisms of cancer induction by tobacco-specific NNK and NNN. Cancers. 2014;6:1138–56. https://doi.org/10.3390/cancers6021138.
Guo J, Zhou S, Huang P, Xu S, Zhang G, He H, et al. NNK-mediated upregulation of DEPDC1 stimulates the progression of oral squamous cell carcinoma by inhibiting CYP27B1 expression. Am J Cancer Res. 2020;10:1745–60.
Doukas SG, Vageli DP, Lazopoulos G, Spandidos DA, Sasaki CT, Tsatsakis A. The effect of NNK, a tobacco smoke carcinogen, on the miRNA and mismatch DNA repair expression profiles in lung and head and neck squamous cancer cells. Cells. 2020;9:1031 https://doi.org/10.3390/cells9041031.
Foki E, Gangl K, Kranebitter V, Niederberger-Leppin V, Eckl-Dorna J, Wiebringhaus R, et al. Early effects of cigarette smoke extract on human oral keratinocytes and carcinogenesis in head and neck squamous cell carcinoma. Head Neck. 2020;42:2348–54. https://doi.org/10.1002/hed.26247.
Benowitz N, Goniewicz ML, Eisner MD, Lazcano-Ponce E, Zielinska-Danch W, Koszowski B, et al. Urine cotinine underestimates exposure to the tobacco-derived lung carcinogen 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone in passive compared with active smokers. Cancer Epidemiol Biomark Prev. 2010;19:2795–2800. https://doi.org/10.1158/1055-9965.EPI-10-0497.
Hecht SS, Stepanov I, Carmella SG. Exposure and metabolic activation biomarkers of carcinogenic tobacco-specific nitrosamines. Acc Chem Res. 2016;49:106–14. https://doi.org/10.1021/acs.accounts.5b00472.
King BA, Patel R, Babb SD, Hartman AM, Freeman A. National and state prevalence of smoke-free rules in homes with and without children and smokers: two decades of progress. Prev Med. 2016;82:51–58. https://doi.org/10.1016/j.ypmed.2015.11.010.
Drope J, Liber AC, Cahn Z, Stoklosa M, Kennedy R, Douglas CE, et al. Who’s still smoking? disparities in adult cigarette smoking prevalence in the United States. A Cancer J Clin. 2018;68:106–15. https://doi.org/10.3322/caac.21444.
Centers for Disease Control and Prevention. Extinguishing the tobacco epidemic in Ohio. 2023. https://www.cdc.gov/tobacco/stateandcommunity/state-fact-sheets/index.htm#OH.
Centers for Disease Control and Prevention. Extinguishing the tobacco epidemic in California. 2023. https://www.cdc.gov/tobacco/stateandcommunity/state-fact-sheets/index.htm#CA.
Matt GE, Merianos AL, Quintana PJE, Hoh E, Dodder NG, Mahabee-Gittens EM. Prevalence and income-related disparities in thirdhand smoke exposure to children. JAMA Netw Open. 2022;5:e2147184 https://doi.org/10.1001/jamanetworkopen.2021.47184.
Hood NE, Ferketich AK, Klein EG, Wewers ME, Pirie P. Individual, social, and environmental factors associated with support for smoke-free housing policies among subsidized multiunit housing tenants. Nicotine Tob Res. 2013;15:1075–83. https://doi.org/10.1093/ntr/nts246.
Matt GE, Quintana PJE, Hoh E, Zakarian JM, Dodder NG, Record RA, et al. Persistent tobacco smoke residue in multiunit housing: legacy of permissive indoor smoking policies and challenges in the implementation of smoking bans. Prev Med Rep. 2020;18:101088 https://doi.org/10.1016/j.pmedr.2020.101088.
Bekö G, Morrison G, Weschler CJ, Koch HM, Pälmke C, Salthammer T, et al. Dermal uptake of nicotine from air and clothing: experimental verification. Indoor Air. 2018;28:247–57. https://doi.org/10.1111/ina.12437.
Sheu R, Stönner C, Ditto JC, Klüpfel T, Williams J, Gentner DR. Human transport of thirdhand tobacco smoke: a prominent source of hazardous air pollutants into indoor nonsmoking environments. Sci Adv. 2020;6:eaay4109 https://doi.org/10.1126/sciadv.aay4109.
Mahabee-Gittens EM, Han G, Merianos AL. Child tobacco smoke exposure, indoor home characteristics, and housing stability among a national sample of U.S. children. Toxics. 2022;10:639 https://doi.org/10.3390/toxics10110639.
Mahabee-Gittens EM, Merianos AL, Stone L, Wullenweber CA, Quintana PJE, Hoh E, et al. Hand nicotine as an independent marker of thirdhand smoke pollution in children’s environments. Sci Total Environ. 2022;849:157914 https://doi.org/10.1016/j.scitotenv.2022.157914.
Acknowledgements
We would like to thank Linda Chu, Kaylen Wilson, and Mansi Vyas of San Diego State University for their assistance with environmental sample analysis.
Funding
This study was funded by the National Institute on Drug Abuse (NIH Grant Number K01DA044313), Eunice Kennedy Shriver National Institute of Child Health and Human Development (NIH Grant Number R01HD083354), and National Institute of Environmental Health Sciences (NIH Grant Number R01ES027815, R01ES030743, and R21ES032161). Instrumentation and other analytical chemistry laboratory resources for the urine analyses at the University of California at San Francisco were supported by the National Institutes of Health (P30DA012393 and S10RR026437). This work was also supported by the California Tobacco-Related Disease Research Program (TRDRP Grant Numbers 28PT-0078 and 28PT-0079).
Author information
Authors and Affiliations
Contributions
Concept and design: ALM, GEM, TMS, RAJ, EH, NGD, PJEQ, NLG, LS, EMMG. Acquisition, analysis or interpretation of data: ALM, GEM, TMS, RAJ, EH, NGD, PJEQ, NLG, LS, EMMG. Statistical analysis: ALM, GEM, TMS, RAJ. Drafting of manuscript: ALM. Critical revision of the manuscript for important intellectual content: GEM, TMS, RAJ, EH, NGD, PJEQ, NLG, LS, EMMG. Final approval of the version to be published: ALM, GEM, TMS, RAJ, EH, NGD, PJEQ, NLG, LS, EMMG.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
All protocols relating to human subjects involved in the study were reviewed and approved by the Cincinnati Children’s Hospital Medical Center’s Institutional Review Board (#2017-5157).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Merianos, A.L., Matt, G.E., Stone, T.M. et al. Contamination of surfaces in children’s homes with nicotine and the potent carcinogenic tobacco-specific nitrosamine NNK. J Expo Sci Environ Epidemiol (2023). https://doi.org/10.1038/s41370-023-00629-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41370-023-00629-8