Abstract
Background
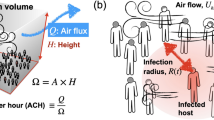
The COVID-19 pandemic was caused by the SARS-CoV-2 coronaviruses transmitted mainly through exposure to airborne respiratory droplets and aerosols carrying the virus.
Objective
To assess the transport and dispersion of respiratory aerosols containing the SARS-CoV-2 virus and other viruses in a small office space using a diffusion-based computational modeling approach.
Methods
A 3-D computational model was used to simulate the airflow inside the 70.2 m3 ventilated office. A novel diffusion model accounting for turbulence dispersion and gravitational sedimentation was utilized to predict droplet concentration transport and deposition. The numerical model was validated and used to investigate the influences of partition height and different ventilation rates on the concentration of respiratory aerosols of various sizes (1, 10, 20, and 50 µm) emitted by continuous speaking.
Results
An increase in the hourly air change rate (ACH) from 2.0 to 5.6 decreased the 1 μm droplet concentration inside the office by a factor of 2.8 and in the breathing zone of the receptor occupant by a factor of 3.2. The concentration at the receptor breathing zone is estimated by the area-weighted average of a 1 m diameter circular disk, with its centroid at the center of the receptor mannequin mouth. While all aerosols were dispersed by airflow turbulence, the gravitational sedimentation significantly influenced the transport of larger aerosols in the room. The 1 and 10 μm aerosols remained suspended in the air and dispersed throughout the room. In contrast, the larger 20 and 50 μm aerosols deposited on the floor quickly due to the gravitational sedimentation. Increasing the partition between cubicles by 0.254 m (10”) has little effect on the smaller aerosols and overall exposure.
Impact
-
This paper provides an efficient computational model for analyzing the concentration of different respiratory droplets and aerosols in an indoor environment. Thus, the approach could be used for assessing the influence of the spatial concentration variations on exposure for which the fully mixed model cannot be used.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout














Similar content being viewed by others
Data availability
Some of the simulation data are available upon request.
References
Boone SA, Gerba CP. Significance of fomites in the spread of respiratory and enteric viral disease. Appl Environ Microbiol. 2007;73:1687–96.
Wang J, Du G. COVID-19 may transmit through aerosol. Ir J Med Sci. 2020;189:1143–4. https://doi.org/10.1007/s11845-020-02218-2.
Morawska L, Cao J. Airborne transmission of SARS-CoV-2: the world should face the reality. Environ Int. 2020;139:105730. https://doi.org/10.1016/j.envint.2020.105730.
Morawska L, Johnson GR, Ristovski ZD, Hargreaves M, Mengersen K, Corbett S. et al. Size distribution and sites of origin of droplets expelled from the human respiratory tract during expiratory activities. J Aerosol Sci. 2009;40:256–69. https://doi.org/10.1016/j.jaerosci.2008.11.002.
Shiu EYC, Leung NHL, Cowling BJ. Controversy around airborne versus droplet transmission of respiratory viruses: implication for infection prevention. Curr Opin Infect Dis. 2019;32:372–9. https://doi.org/10.1097/QCO.0000000000000563.
Wang CC, Prather AK, Sznitman J, Jimenez L, Lakdawala SS, Tufekci Z, et al. Airborne transmission of respiratory viruses. Science. 2021;373:6558. https://doi.org/10.1126/science.abd9149.
Beggs CB. Is There an Airborne Component to the transmission of COVID-19? A Quantitative Analysis Study. 2020, medRxiv. https://doi.org/10.1101/2020.05.22.20109991.
Karimzadeh S, Bhopal R, Tien HN. Review of infective dose, routes of transmission and outcome of COVID-19 caused by the SARS-COV-2: comparison with other respiratory viruses. Epidemiol Infect. 2021;149. https://doi.org/10.1017/S0950268821000790.
Abkarian M, Mendez S, Xue N, Yang F, Stone HA. Speech can produce jet-like transport relevant to asymptomatic spreading of virus. Proc Natl Acad Sci. 2020;117:25237–45. https://doi.org/10.1073/pnas.2012156117.
Bourouiba L. The fluid dynamics of disease transmission. Annu Rev Fluid Mech. 2021;53:473–508. https://doi.org/10.1146/annurev-fluid-060220-113712.
Gregson FKA, Watson NA, Orton CM, Haddrell AE, McCarthy LP, Finnie TJR. et al. Comparing aerosol concentrations and particle size distributions generated by singing, speaking and breathing. Aerosol Sci Technol. 2021;55:681–91. https://doi.org/10.1080/02786826.2021.1883544.
Asadi S, Wexler AS, Cappa CD, Barreda S, Bouvier NM, Ristenpart WD. Aerosol emission and superemission during human speech increase with voice loudness. Sci Rep. 2019;9:2348–57. https://doi.org/10.1038/s41598-019-38808-z.
Puayen Tan Z, Silwal L, Bhatt SP, Raghav V. Experimental characterization of speech aerosol dispersion dynamics. Sci Rep. 2021;11:3953. https://doi.org/10.1038/s41598-021-83298-7.
Asadi S, Bouvier N, Wexler AS, Ristenpart WD. The coronavirus pandemic and aerosols: does COVID-19 transmit via expiratory particles. J Aerosol Sci Technol. 2020;54:635–8. https://doi.org/10.1080/02786826.2020.1749229.
Asadi S, Wexler AS, Cappa CD, Barreda S, Bouvier NM, Ristenpart WD. Effect of voicing and articulation manner on aerosol particle emission during human speech. PLoS ONE. 2020b;15:1–15. https://doi.org/10.1371/journal.pone.0227699.
Gralton J, Tovey ER, McLaws M-L, Rawlinson WD, Respiratory Virus. RNA is detectable in airborne and droplet particles. J Med Virol. 2013;85:2151–9. https://doi.org/10.1002/jmv.23698.
Jones RM, Brosseau LM. Aerosol transmission of infectious disease. J Occupant Environ, Med. 2015;57:501–8. https://doi.org/10.1097/JOM.0000000000000448.
Wei J, Li Y. Airborne spread of infectious agents in the indoor environment. Am J Infect Control. 2016;44:S102–S108. https://doi.org/10.1016/j.ajic.2016.06.003.
Niazi S, Groth R, Spann K, Johnson GR. The role of respiratory droplet physicochemistry in limiting and promoting the airborne transmission of human coronaviruses: a critical review. Environ Pollut. 2021;276:115767. https://doi.org/10.1016/j.envpol.2020.115767.
Vejerano EP, Marr IC. Physico-chemical characteristics of evaporating respiratory fluid droplets. J R Soc Interface. 2018;15:20170939. https://doi.org/10.1098/rsif.2017.0939.
Duguid JP. The size and the duration of air-carriage of respiratory droplets and droplet-nuclei. Epidemio Infect. 1946;44:471–9. https://doi.org/10.1017/S0022172400019288.
Papineni RS, Rosenthal FS. The size distribution of droplets in the exhaled breath of healthy human subjects. J Aerosol Med 1997;10:105–16. https://doi.org/10.1089/jam.1997.10.105.
Morawska L. Droplet fate in indoor environments, or can we prevent the spread of infection? Indoor Air. 2006;16:335–47. https://doi.org/10.1111/j.16000668.2006.
Morawska L, Ayoko G, Bae G, Buonanno G, Chao C, Clifford S. et al. Airborne particles in indoor environment of homes, schools, offices and aged care facilities: the main routes of exposure. Environ Int. 2017;108:75–83. https://doi.org/10.1016/j.envint.2017.07.025.
Zayas G, Chiang MC, Wong E, MacDonald F, Lange CF, Senthilselvan A. et al. Cough aerosol in healthy participants: fundamental knowledge to optimize droplet-spread infectious respiratory disease management. BMC Pulm Med. 2012;12:11. https://doi.org/10.1186/1471-2466-12-11.
Fabian P, Brain J, Houseman EA, Gern J, Milton DK. Origin of exhaled breath particles from healthy and human rhinovirus-infected subjects. J Aerosol Med Pulm Drug Deliv. 2011;24:137–47. https://doi.org/10.1089/jamp.2010.0815.
Holmgren H, Ljungström E, Almstrand A-C, Bake B. Size distribution of exhaled particles in the range from 0.01 to 2.0 μm. J Aerosol Sci. 2010;41:439–46. https://doi.org/10.1016/j.jaerosci.2010.02.011.
Shao S, Zhou D, He R, Li J, Zou S, Mallery K. et al.Risk assessment of airborne transmission of COVID-19 by asymptomatic individuals under different practical settings.J Aerosol Sci. 2021;151:105661. https://doi.org/10.1016/j.jaerosci.2020.105661.
Roy CJ, Milton DK. Airborne transmission of communicable infection—the Elusive pathway. N. Engl J Med. 2004;350:1710–2. https://doi.org/10.1056/NEJMp048051.
Johnson GR, Morawska L, Ristovski ZD, Hargreaves M, Mengersen K, Chao CYH. et al. Modality of human expired aerosol size distributions. J Aerosol Sci. 2011;42:839–51. https://doi.org/10.1016/j.jaerosci.2011.07.009.
Xie X, Li Y, Sun H, Liu L. Exhaled droplets due to talking and coughing. J R Soc Interface. 2009;6:S703–S714. https://doi.org/10.1098/rsif.2009.0388.focus.
Parienta D, Moraska L, Johnson GR, Ristovski ZD, Hargreaves M, Mengersen K. et al. Theoretical analysis of the motion and evaporation of exhaled respiratory droplets of mixed composition. J Aerosol Sci. 2011;42:1–10. https://doi.org/10.1016/j.jaerosci.2010.10.005.
Mittal R, Ni R, Seo JH. The flow physics of COVID-19. J Fluid Mech. 2020;894:1–14. https://doi.org/10.1017/jfm.2020.330.
Bourouiba L. Turbulent gas clouds and respiratory pathogen emissions: potential implications for reducing transmission of COVID-19. J Am Med Assoc JAMA. 2020;323:1837–8. https://doi.org/10.1001/jama.2020.4756.
Kwon SB, Park J, Jang J, Cho Y, Park D-S, Kim C, et al. Study on the initial velocity distribution of exhaled air from coughing and speaking. Chemosphere. 2012;87:1260–4. https://doi.org/10.1016/j.chemosphere.2012.01.032.
Chen H, Guo J, Wang C, Luo F, Yu X, Zhang W. et al. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395:809–15. https://doi.org/10.1016/s0140-6736(20)30360-3.
Vuorinen V, Aarnio M, Alava M, Alopaeus V, Atanasova N, Auvinen M, et al. Modeling aerosol transport and virus exposure with numerical simulations in relation to SARS-CoV-2 transmission by inhalation indoors. J Saf Sci. 2020;130:104866. https://doi.org/10.1016/j.ssci.2020.104866.
Wells WF. On air-borne infection: Study II. Droplets and droplet nuclei. Am J Epidemiol. 1934;20:611–8. https://doi.org/10.1093/oxfordjournals.aje.a118097.
Xie X, Li Y, Chwang ATY, Ho PL, Seto WH. How far droplets can move in indoor environments- revisiting the wells evaporation-falling curve. Indoor Air. 2007;17:211–25. https://doi.org/10.1111/j.1600-0668.2007.00469.x.
Doremalen N, Van, Bushmaker T, Morris DH, Holbrook M, Gamble A, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl J Med. 2020;382:1564–7. https://doi.org/10.1056/NEJMc2004973.
Smither SJ, Eastaugh LS, Findlay JS, Lever MS. Experimental aerosol survival of SARS-CoV-2 in artificial saliva and tissue culture media at medium and high humidity. Emerg Microbes Infect. 2020;9:1415–7. https://doi.org/10.1080/22221751.2020.1777906.
Dabisch P, Schuit M, Herzog A, Beck K, Wood S, Krause M. et al. The influence of temperature, humidity, and simulated sunlight on the infectivity of SARS-CoV-2 in aerosols. Aerosol Sci Technol. 2021;55:142–53. https://doi.org/10.1080/02786826.2020.1829536.
Li Y, Leung G, Tang J, Yang X, Chao CYH, Lin J. et al. Role of ventilation in airborne transmission of infectious agents in the built environment—a multi-disciplinary systematic review. Indoor Air. 2007;17:2–18. https://doi.org/10.1111/j.1600-0668.2006.00445.x.
Ai ZT, Melikov AK. Airborne spread of expiratory droplet nuclei between the occupants of indoor environments: a review. Indoor Air. 2018;28:500–24. https://doi.org/10.1111/ina.12465.
WHO (2021) Roadmap to Improve and Ensure Good Indoor Ventilation in the Context of COVID-19. (2021), www.who.int/publications/i/item/9789240021280.
Peng Z, Pineda Rojas AL, Kropff E, Bahnfleth W, Buonanno G, Dancer SJ. et al. Practical indicators for risk of airborne transmission in shared indoor environments and their application to COVID-19 outbreaks. Environ Sci Technol. 2022;56:1125–1137. https://doi.org/10.1021/acs.est.1c06531.
Li Y, Huang X, Yu ITS, Wong T, Qian H. Role of air distribution in SARS transmission during the largest nosocomial outbreak in Hong Kong. Indoor Air. 2005;15:83–95. https://doi.org/10.1111/j.1600-0668.2004.00317.x.
Olmedo I, Nielsen PV, Ruiz de Adana M, Jensen RL, Grzelecki P. Distribution of exhaled contaminants and personal exposure in a room using three different air distribution strategies. Indoor Air. 2012;22:64–76. https://doi.org/10.1111/j.1600-0668.2011.00736.x.
Cao G, Nielsen PV, Jensen RL, Heiselberg P, Liu L, Heikkinen J. Protected zone ventilation and reduced personal exposure to airborne cross-infection. Indoor Air. 2015;25:307–19. https://doi.org/10.1111/ina.12142.
Li F, Liu J, Ren J, Cao X. Predicting contaminant dispersion using modified turbulent schmidt numbers from different vortex structures. Build Environ. 2018;130:120–7. https://doi.org/10.1016/j.buildenv.2017.12.023.
Ai Z, Hashimoto K, Melikov AK. Airborne transmission between room occupants during short-term events: measurement and evaluation. Indoor Air. 2019;29:63–576. https://doi.org/10.1111/ina.12557.
King MF, Noakes CJ, Sleigh PA. Modeling environmental contamination in hospital single and four-bed rooms. Indoor Air. 2015;25:694–707. https://doi.org/10.1111/ina.12186.
Cho J. Investigation on the contaminant distribution with improved ventilation system in hospital isolation rooms: effect of supply and exhaust air diffuser configurations. Appl Therm Eng. 2019;148:208–18. https://doi.org/10.1016/j.applthermaleng.2018.11.023.
He Q, Niu J, Gao N, Zhu T, Wu J. CFD study of exhaled droplet transmission between occupants under different ventilation strategies in a typical office room. Build Environ. 2011;46:397–408. https://doi.org/10.1016/j.buildenv.2010.08.003.
Hinds WC. Aerosol Technology: Properties, Behavior, and Measurement of Air Borne Particles. Second edition, Hoboken, New Jersey, USA.: John Wiley & Sons; 1999.
Friedlander SK. Smoke, Dust and Haze - Fundamentals of Aerosol Behaviour. New York: 1977; John Wiley & Sons.
Tu J, Inthavong K, Ahmadi G. Computational Fluid and Particle Dynamics in the Human Respiratory System. Netherlands: Springer; 2013. https://doi.org/10.1007/978-94-007-4488-2
Mofakham AA, Ahmadi G. Particles Dispersion and Deposition in Inhomogeneous Turbulent Flows Using Continuous Random Walk Models, Phys Fluids 2019;31:083301-1-13.
Mofakham AA, Ahmadi G. On random walk models for simulation of particle-laden turbulent flows. Int J Multiph Flow. 2020;122:103157. https://doi.org/10.1016/j.ijmultiphaseflow.2019.103157.
Mofakham AA, Ahmadi G. Improved Discrete Random Walk Stochastic Model for Simulating Particle Dispersion and Deposition in Inhomogeneous Turbulent Flows. J Fluids Eng. 2020b;142:101401-1-14. https://doi.org/10.1115/1.4047538.
Liu L, Li Y, Nielsen PV, Wei J, Jensen RL. Short-range airborne transmission of expiratory droplets between two people. Indoor Air. 2017;27:452–62. https://doi.org/10.1111/ina.12314.
Barbosa BPP, Brum NDCL. Validation and assessment of the CFD-0 module of CONTAM software for airborne contaminant transport simulation in laboratory and hospital applications. J Build Environ. 2018;142:139–52. https://doi.org/10.1016/j.buildenv.2018.06.013.
Gilani S, Montazeri H, Blocken B. CFD simulation of stratified indoor environment in displacement ventilation: validation and sensitivity analysis. J Build Environ. 2015;95:299–313. https://doi.org/10.1016/j.buildenv.2015.09.010.
Kotb H, Khalil EE. Sneeze and Cough Pathogens Migration Inside Aircraft Cabins. REHVA J. 2020:36-45. https://www.rehva.eu/rehva-journal/chapter/sneeze-and-coughpathogens-migration-inside-aircraft-cabins.
Ren J, Wang Y, Liu Q, Liu Y.Numerical study of three ventilation strategies in a prefabricated COVID-19 inpatient ward.J Build Environ. 2021;188:107467. https://doi.org/10.1016/j.buildenv.2020.107467.
Liu W, Chen Q. Development of adaptive coarse grid generation methods for fast fluid dynamics in simulating indoor airflow. J Build Perform Simul. 2018;11:470. https://doi.org/10.1080/19401493.2017.1397195.
Yan Y, Li X, Tu J. Thermal effect of human body on cough droplets evaporation and dispersion in an enclosed space. J Build Environ. 2019;148:96–106. https://doi.org/10.1016/j.buildenv.2018.10.039.
Yang X, Ou C, Yang H, Liu L, Song T, Kang M, et al. Transmission of pathogen-laden expiratory droplets in a coach bus. J Hazard Mater. 2020;397:122609. https://doi.org/10.1016/j.jhazmat.2020.122609.
Abuhegazy M, Talaat K, Anderoglu O, Poroseva SV. Numerical investigation of aerosol transport in a classroom with relevance to COVID-19. Phys Fluids. 2020;32:103311. https://doi.org/10.1063/5.0029118.
Mirzaie M, Lakzian S, Khan A, Ebrahimi Warkiani M, Mahian O, Ahmadi G. COVID-19 spread in a classroom equipped with partition—A CFD approach. J Hazard Mater. 2021;420:126587. https://doi.org/10.1016/j.jhazmat.2021.126587.
Foster A, Kinzel M. Estimating COVID-19 exposure in a classroom setting: a comparison between mathematical and numerical models. Phys Fluids. 2021;33:021904. https://doi.org/10.1063/5.0040755.
Ahmed T, Rawat MS, Ferro AR, Mofakham AA, Helenbrook BT, Ahmadi G. et al. Characterizing respiratory aerosol emissions during sustained phonation. J Exposure Environ Epidemiol. 2022;32:689–96. https://doi.org/10.1038/s41370-022-00430-z.
ANSYS, Inc.“Introduction to ANSYS FLUENT 12.0. “Lecture 5 Solver Setting” ANSYS Release 13. Canonsburg, PA, USA: “ANSYS, Inc.; 2010. pp: 8-30.
ANSYS Inc. ANSYS-FLUENT 12.0/12.1 Documentation. Computer program manual. Canonsburg PA: ANSYS Inc.; 2019. https://www.afs.enea.it/project/neptunius/docs/fluent/index.htm.
ANSYS, Inc. Ansys Theory Guide (Release 15), Canonsburg PA: ANSYS Inc.; 2019. http://www.pmt.usp.br/academic/martoran/notasmodelosgrad/ANSYS%20Fluent%20Theory%20Guide%2015.pdf.
Anderson WK, Bonhaus DL. An implicit upwind algorithm for computing turbulent flows on unstructured grids. Computational Fluids. 1994;23:1–21.
Bakker A. Lecture 5- “Solution Methods Applied Computational Fluid Dynamics; Lectures of Fluent Instructor. New York, NY, USA: Fluent Inc.; 2002. pp. 41-43.
Versteeg HK, Malalasekera W. An Introduction to Computational Fluid Dynamics, The Finite Volume Method. Second Edition. Pearson Practice Hall; 1995. http://sutlib2.sut.ac.th/sut_contents/H109101.pdf.
Chitta V, Dhakal TP, Walters DK. Sensitization of a transition-sensitive linear eddy-viscosity model to rotation and curvature effects. J Fluids Eng. 2015;137:031207. https://doi.org/10.1115/1.4028627.
Ramadan AB, Abd El-Rahman AI, Sabry AS. Assessment of the transition k-kL-ω model application to transitional oscillatory pipe flows. J Acoustical Soc Am. 2019;145:1195. https://doi.org/10.1121/1.5092605.
Salimipour E. A modification of the k-kl-ω turbulence model for simulation of short and long separation bubbles. J Computers Fluids. 2019;181:67–76. https://doi.org/10.1016/j.compfluid.2019.01.003.
Liu Z, Lu Y, Wang S, Wang Q, Yan C. Physics-based model for boundary layer transition prediction in a wide speed range. Chin J Aeronautics. 2022;35:143–59. https://doi.org/10.1016/j.cja.2022.02.002.
Tian L, Ahmadi G. Particle deposition in turbulent duct flows—comparisons of different model predictions. J Aerosol Sci. 2007;38:377–97.
Longest PW, Xi JX. Effectiveness of direct lagrangian tracking models for simulating nanoparticle deposition in the upper airways. Aerosol Sci Technol. 2007;41:380–97. https://doi.org/10.1080/02786820701203223.
Chen W, Zhang N, Wei J, Yen H-L, Li Y. Short-range airborne route dominates exposure of respiratory infection during close contact. J Build Environ. 2020;176:106859. https://doi.org/10.1101/2020.03.16.20037291.
Kannan R, Guo P, Przekwas A. Particle Transport in the Human Respiratory Tract: Formulation of a Nodal Inverse Distance Weighted Eulerian-Lagrangian Transport and Implementation of the Wind-Kessel algorithm for an oral delivery. Int J Numer Methods Biomed Eng. 2016;32. https://doi.org/10.1002/cnm.2746.
Tohidi R, Sajadi B, Ahmadi G. The effect of nasal airway obstruction on the dispersion and deposition of inhaled volatile droplets in the human nasal cavity: a numerical study. J Aerosol Sci. 2020;150:105650. https://doi.org/10.1016/j.jaerosci.2020.105650.
D’Alessandro V, Falone M, Giammichele L, Ricci R. Eulerian-Lagrangian Modeling of Cough Droplets Irradiated by Ultraviolet-C Light in Relation to SARS-CoV-2 Transmission. Phys Fluids. 2021;33. https://doi.org/10.1063/5.0039224.
Mitsakou C, Helmis C, Housiadas C. Eulerian modelling of lung deposition with sectional representation of aerosol dynamics. J Aerosol Sci. 2005;36:75–94. https://doi.org/10.1016/j.jaerosci.2004.08.008.
Zhang Z, Chen Q. Comparison of the Eulerian and Lagrangian methods for predicting particle transport in enclosed spaces. Atmos Environ. 2007;41:5236–48. https://doi.org/10.1016/j.atmosenv.2006.05.086.
Peng S, Chen Q, Liu E. Corrigendum to “The Role of Computational Fluid Dynamics Tools on Investigation of Pathogen Transmission: Prevention and control. Sci Total Environ. 764, Article 142090, 746 (2020), (2021). https://doi.org/10.1016/j.scitotenv.2020.142862.
Moshfeghi M, Hur N. Investigation on the Effects of Different Ventilation Scenarios on Spread Patterns and Risk Factor of COVID-19 Virus in Indoor Spaces. In Proceedings of the Asian Symposium on Computational Heat Transfer Fluid Flow. (ASCHT2021), 23–26 September, 2021. Qingdao, China, http://ascht2021.svipmeeting.com/web/en.
Panero J, Zelnik M. Human Dimension & Interior Space: A Source Book of Design Reference Standards. Whitney Library of Design, an imprint of Watson-Guptill Publications. New York: Watson-Guptill Publications, NA2542.4.P356 1979 729 79-20874, New York, 01 January, 1979.
American Society of Heating, Refrigerating, and Air-Conditioning Engineers, in ASHRAE Standard 62.1-2019: Ventilation and acceptable indoor air quality. Atlanta, GA: ASHRAE, Inc.; 2019.
American Society of Heating, Refrigerating, and Air-Conditioning Engineers, in ASHRAE Standard 62.1-2007: Ventilation and acceptable indoor air quality. Atlanta, GA: ASHRAE, Inc.; 2007.
American Society of Heating, Refrigerating, and Air-Conditioning Engineers, in (2012), ASHRAE Handbook - HVAC Systems and Equipment, (Atlanta, GA: ASHRAE, Inc.; 2012.
Lindsley W, Reynolds JS, Szalajda JV, Noti JD, Beezhold DH. A cough aerosol simulator for the study of disease transmission by human cough generated aerosols. Aerosol Sci Technol. 2013;47:937–44. https://doi.org/10.1080/02786826.2013.803019.
Buonanno G, Stabile L, Morawska L. Estimation of airborne viral emission: quanta emission rate of SARS-CoV-2 for infection risk assessment. J Environ Int. 2020a;141:105794. https://doi.org/10.1016/j.envint.2020.105794.
Buonanno G, Morawska L, Stabile L. Quantitative assessment of the risk of airborne transmission of SARS-CoV-2 infection: prospective and retrospective applications. J Environ Int. 2020b;145:106112. https://doi.org/10.1016/j.envint.2020.106112.
Nazaroff WW. Indoor Particle Dynamics. Indoor Air. 2004;14((Suppl. 7):175–83. https://doi.org/10.1111/j.1600-0668.2004.00286.x.
Yalçın N, Özmen A, Balta D. The Use of Mass Balance-Based Model for Indoor Air Pollutant Concentration Modeling Problem. AKADEMiC PLATFORN, (2014): 716-25, t: https://www.Researchgate.net/publication/289520478.
Acknowledgements
The authors gratefully acknowledge the support of the US Environmental Protection Agency (EPA) through contact # 68HE0B21P0037. Thanks, are also given to Dr. Parsa Zamankan of ANSYS Inc. for his assistance in developing the UDF models.
Author information
Authors and Affiliations
Contributions
SO, with contributions from GA, developed the computational model, performed the simulations, and interpreted the results. SO also was responsible for the model validation and drafted the initial manuscript. PW, JRR, and VI contributed to the project’s conceptualization, provided scientific support, and reviewed the manuscript. MSR and ARF performed the simulations for the fully mixed model, provided scientific support, and reviewed the manuscript. Finally, GA and ARF were responsible for the project’s conceptualization, developing the methodologies, supervising the project, data interpretation, and manuscript writing and editing. All authors contributed to the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Obeid, S., White, P., Rosati Rowe, J. et al. Airborne respiratory aerosol transport and deposition in a two-person office using a novel diffusion-based numerical model. J Expo Sci Environ Epidemiol (2023). https://doi.org/10.1038/s41370-023-00546-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41370-023-00546-w