Abstract
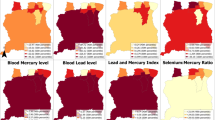
Previous research has found that women and children living in rural, interior communities in Suriname have high concentrations of mercury in hair. Freshwater fish from these areas also have high concentrations of mercury. Artisanal and small-scale gold mining operations in parts of the country use elemental mercury to extract gold from soils and sediments. Total mercury and methylmercury concentrations have been determined in hair and blood from pregnant women across the country. Pregnant women from interior communities have significantly higher concentrations of both total and methylmercury in hair (median total mercury in hair 3.64 µg/g) compared with pregnant women from two urban coastal cities, Paramaribo (0.63 µg/g) and Nickerie (0.74 µg/g). Total and methylmercury concentrations in blood and hair are highly correlated (r = 0.986, r = 0.974) with methylmercury making up 86% of the total in blood and 97% of the total in hair. Most women in the interior regions rely heavily on local fish as part of their regular diet, and many live outsides of areas with active ASGM operations. This study demonstrates that diet and fish consumption largely govern mercury exposures in pregnant women in Suriname.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Clarkson TW. The three modern faces of mercury. Environ Health Perspect. 2002;110(Suppl 1):11–23.
Clarkson TW, Magos L. The toxicology of mercury and its chemical compounds. Crit Rev Toxicol. 2006;36:609–62.
Bakir F, Damluji SF, Amin-Zaki L, Murtadha M, Khalidi A, Al-Rawi NY, et al. Methylmercury poisoning in Iraq. Science. 1973;181:230–41.
Castaño A, Cutanda F, Esteban M, Pärt P, Navarro C, Gómez S, et al. Fish consumption patterns and hair mercury levels in children and their mothers in 17 EU countries. Environ Res. 2015;141:58–68.
Harada M. Minamata disease: methylmercury poisoning in Japan caused by environmental pollution. Crit Rev Toxicol. 1995;25:1–24.
Hawkins WB. Global environmental public health issues related to gold mining and mercury contamination in Indigenous communities in Suriname, South America. School of Public Health and Tropical Medicine. New Orleans, LA: Tulane University; 2012.
Mahaffey KR, Clickner RP, Jeffries RA. Adult women’s blood mercury concentrations vary regionally in the United States: association with patterns of fish consumption (NHANES 1999-2004). Environ Health Perspect. 2008;117:47–53.
Ouboter PE, Landburg GA. Mercury poisoning: a threat to Brownsweg villagers. Paramaribo, Suriname: World Wildlife Foundation; 2010.
Ricketts P, Basu N, Fletcher H, Voutchkov M, Bassaw B. Assessment of fish consumption and mercury exposure among pregnant women in Jamaica and Trinidad and Tobago. Chemosphere. 2016;164:462–8.
Strain J, Yeates AJ, van Wijngaarden E, Thurston SW, Mulhern MS, McSorley EM, et al. Prenatal exposure to methyl mercury from fish consumption and polyunsaturated fatty acids: associations with child development at 20 mo of age in an observational study in the Republic of Seychelles. Am J Clin Nutr. 2015;101:530–7.
vvan Wijngaarden E, Thurston SW, Myers GJ, Harrington D, Cory-Slechta DA, Strain JJ, et al. Methyl mercury exposure and neurodevelopmental outcomes in the Seychelles Child Development Study Main cohort at age 22 and 24 years. Neurotoxicology Teratol. 2017;59:35–42.
Zilversmit L, Wickliffe J, Shankar A, Taylor R, Harville E. Correlations of biomarkers and self-reported seafood consumption among pregnant and non-pregnant women in southeastern Louisiana after the Gulf oil spill: the GROWH study. Int J Environ Res Public Health. 2017;14:784.
Grandjean P, Weihe P, Jorgensen PJ, Clarkson T, Cernichiari E, Videro T. Impact of maternal seafood diet on fetal exposure to mercury, selenium, and lead. Arch Environ Health. 1992;47:185–95.
Dong Z, Jim RC, Hatley EL, Backus ASN, Shine JP, Spengler JD, et al. A longitudinal study of mercury exposure associated with consumption of freshwater fish from a reservoir in rural south central USA. Environ Res. 2015;136:155–62.
UNEP. Global mercury assessment 2018. Geneva: UN Environment Program, Chemicals and Health Branch; 2019.
Lawley R, Curtis L, Davis J. The food safety hazard guidebook. Cambridge: The Royal Society of Chemistry; 2012. 533 p.
Ratcliffe HE, Swanson GM, Fischer LJ. Human exposure to mercury: a critical assessment of the evidence of adverse health effects. J Toxicol Environ Health. 1996;49:221–70.
Crump KS, Kjellström T, Shipp AM, Silvers A, Stewart A. Influence of prenatal mercury exposure upon scholastic and psychological test performance: benchmark analysis of a New Zealand cohort. Risk Anal. 1998;18:701–13.
Grandjean P, Weihe P, Debes F, Choi AL, Budtz-Jørgensen E. Neurotoxicity from prenatal and postnatal exposure to methylmercury. Neurotoxicology Teratol. 2014;43:39–44.
Grandjean P, Weihe P, White RF, Debes F. Cognitive performance of children prenatally exposed to “safe” levels of methylmercury. Environ Res. 1998;77:165–72.
Grandjean P, Weihe P, White RF, Debes F, Araki S, Yokoyama K, et al. Cognitive deficit in 7-year-old children with prenatal exposure to methylmercury. Neurotoxicology Teratol. 1997;19:417–28.
Marsh DO, Clarkson TW, Cox C, Myers GJ, Amin-Zaki L, Al-Tikriti S. Fetal methylmercury poisoning: relationship between concentration in single strands of maternal hair and child effects. Arch Neurol. 1987;44:1017–22.
USEPA. Mercury study report to congress volume v: health effects of mercury and mercury compounds. EPA-452/R-97-007 ed. Washington, D.C.: USEPA; 1997. p. 1-348.
WHO. Evaluation of certain food additives and contaminants: sixty-seventh report of the Joint FAO/WHO Expert Committee on Food Additives. 2006.
USEPA. Resources for mercury science and research. USEPA; 2019. https://www.epa.gov/mercury/resources-mercury-science-and-research.
Donohue A, Wagner CL, Burch JB, Rothenberg SE. Blood total mercury and methylmercury among pregnant mothers in Charleston, South Carolina, USA. J Expo Sci Environ Epidemiol. 2018;28:494–504.
Mortensen ME, Caudill SP, Caldwell KL, Ward CD, Jones RL. Total and methyl mercury in whole blood measured for the first time in the U.S. population: NHANES 2011–2012. Environ Res. 2014;134:257–64.
Mahaffey KR, Clickner RP, Bodurow CC. Blood organic mercury and dietary mercury intake: National Health and Nutrition Examination Survey, 1999 and 2000. Environ health Perspect. 2004;112:562–70.
UNEP. Global mercury assessment: sources, emissions, releases and environmental transport. Geneva: UN Environment Program, Chemicals Branch; 2013.
Manceau A, Enescu M, Simionovici A, Lanson M, Gonzalez-Rey M, Rovezzi M, et al. Chemical forms of mercury in human hair reveal sources of exposure. Environ Sci Technol. 2016;50:10721–9.
Laffont L, Sonke JE, Maurice L, Monrroy SL, Chincheros J, Amouroux D, et al. Hg speciation and stable isotope signatures in human hair as a tracer for dietary and occupational exposure to mercury. Environ Sci Technol. 2011;45:9910–6.
Airey D. Mercury in human hair due to environment and diet: a review. Environ Health Perspect. 1983;52:303–16.
Fitzgerald WF, Clarkson TW. Mercury and monomethylmercury: present and future concerns. Environ Health Perspect. 1991;96:159–66.
Cordy P, Veiga MM, Salih I, Al-Saadi S, Console S, Garcia O, et al. Mercury contamination from artisanal gold mining in Antioquia, Colombia: the world’s highest per capita mercury pollution. Sci Total Environ. 2011;410-411:154–60.
Ha E, Basu N, Bose-O’Reilly S, Dórea JG, McSorley E, Sakamoto M, et al. Current progress on understanding the impact of mercury on human health. Environ Res. 2017;152:419–33.
Seccatore J, Veiga M, Origliasso C, Marin T, De Tomi G. An estimation of the artisanal small-scale production of gold in the world. Sci Total Environ. 2014;496:662–7.
Spiegel S, Keane S, Metcalf S, Veiga M, Yassi A. The Minamata convention on mercury: time to seek solutions with artisanal mining communities. Environ Health Perspect. 2014;122:A203–A4.
Steckling N, Boese-O’Reilly S, Gradel C, Gutschmidt K, Shinee E, Altangerel E, et al. Mercury exposure in female artisanal small-scale gold miners (ASGM) in Mongolia: an analysis of human biomonitoring (HBM) data from 2008. Sci Total Environ. 2011;409:994–1000.
Steckling N, Tobollik M, Plass D, Hornberg C, Ericson B, Fuller R, et al. Global burden of disease of mercury used in artisanal small-scale gold mining. Ann Glob Health. 2017;83:234–47.
Veiga MM, Angeloci-Santos G, Meech JA. Review of barriers to reduce mercury use in artisanal gold mining. Extractive Industries Soc. 2014;1:351–61.
Gibb H, O’Leary KG. Mercury exposure and health impacts among individuals in the artisanal and small-scale gold mining community: a comprehensive review. Environ Health Perspect. 2014;122:667–72.
Legg ED, Ouboter PE, Wright MAP. Small-scale gold mining related mercury contamination in the Guianas: a review. Paramaribo, Suriname: World Wildlife Fund; 2015.
Ouboter PE, Landburg GA, Quik JHM, Mol JHA, van der Lugt F. Mercury levels in pristine and gold mining impacted aquatic ecosystems of Suriname, South America. Ambio. 2012;41:873–82.
Ouboter PE, Landburg GA, White C, Mol J, van der Lugt F, Quik JHM. Final technical report mercury pollution in the greenstone belt. Paramaribo, Suriname: World Wildlife Fund; 2007.
Mohan S, Tiller M, Van der Voet G, Kanhai H. Mercury exposure of mothers and newborns in Surinam: a pilot study. Clin Toxicol. 2005;43:101–4.
Ouboter P, Landburg G, Satnarain G, Starke S, Nanden I, Simon-Friedt B, et al. Mercury levels in women and children from interior villages in Suriname, South America. Int J Environ Res Public Health. 2018;15:1007.
Basu N, Horvat M, Evers DC, Zastenskaya I, Weihe P, Tempowski J. A state-of-the-science review of mercury biomarkers in human populations worldwide between 2000 and 2018. Environ Health Perspect. 2018;126:106001.
Lichtveld MY, Zijlmans CWR, Ouboter PE, Hawkins WB, Wickliffe JK, Abdoel Wahid F, et al. The Caribbean consortium for research in environmental and occupational health: examining the impact of neurotoxicant exposures on maternal and child health in Suriname. NIEHS Environmental Health Science FEST; Durham, NC: NIEHS; 2016.
Pellizzari ED, Fernando R, Cramer GM, Meaburn GM, Bangerter K. Analysis of mercury in hair of EPA Region V population. J Expo Sci Environ Epidemiol. 1999;9:393–401.
Kim B-G, Jo E-M, Kim G-Y, Kim D-S, Kim Y-M, Kim R-B, et al. Analysis of methylmercury concentration in the blood of Koreans by using cold vapor atomic fluorescence spectrophotometry. Ann Lab Med. 2012;32:31–7.
Liang L, Evens C, Lazoff S, Woods JS, Cernichiari E, Horvat M, et al. Determination of methyl mercury in whole blood by ethylation-GC-CVAFS after alkaline digestion-solvent extraction. J Anal Toxicol. 2000;24:328–32.
Hammerschmidt CR, Fitzgerald WF. Bioaccumulation and trophic transfer of methylmercury in Long Island Sound. Arch Environ Contamination Toxicol. 2006;51:416–24.
USEPA. Method 1630, methyl mercury in water by distillation, aqueous ethylation, purge and trap, and CVAFS. EPA-821-R-01-020 ed. Washington, D.C.: U.S. Environmental Protection Agency, Office of Water; 2001.
USGS. Determination of methyl mercury by aqueous phase ethylation, followed by gas chromatographic separation with cold vapor atomic fluorescence detection. Open-File Report 01-445 ed. Reston, VA: U.S. Department of the Interior; 2002.
USEPA. Method 1631, Revision E: mercury in water by oxidation, purge and trap, and cold vapor atomic fluorescence spectrometry. EPA-821-R-02-019 ed. Washington, D.C.: U.S. Environmental Protection Agency, Office of Water; 2002.
CDC. Laboratory procedure manual, cadmium, lead, manganese, mercury, and selenium in whole blood. Blood metals panel 3. DLS 3016.8-04 ed. Atlanta, GA: National Center for Environmental Health, Centers for Disease Control; 2014.
CDC. Laboratory procedure manual, iodine and mercury in urine (MEC and 24-Hour). Iodine and mercury in urine by ICP-DRC-MS. DLS 3002.7-02 ed. Atlanta, GA: National Center for Environmental Health, Centers for Disease Control; 2014.
Yu X, Chandrasekhar TM. Analysis of methyl mercury in sediment and tissue by KOH/CH3OH digestion followed by aqueous phase ethylation. Tallahassee, FL: Florida Department of Environmental Protection, Bureau of Laboratories; 2005.
Davidson PW, Strain JJ, Myers GJ, Thurston SW, Bonham MP, Shamlaye CF, et al. Neurodevelopmental effects of maternal nutritional status and exposure to methylmercury from eating fish during pregnancy. NeuroToxicology. 2008;29:767–75.
Grandjean P, Weihe P, Nielsen F, Heinzow B, Debes F, Budtz-Jorgensen E. Neurobehavioral deficits at age 7 years associated with prenatal exposure to toxicants from maternal seafood diet. Neurotoxicology Teratol. 2012;34:466–72.
Grandjean P, Jørgensen PJ, Weihe P. Human milk as a source of methylmercury exposure in infants. Environ Health Perspect. 1994;102:74–7.
Acknowledgements
Research reported in this publication was supported by the Fogarty International Center of the National Institutes of Health under Award Numbers U01TW010087 and U2RTW010104. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Wickliffe, J.K., Lichtveld, M.Y., Zijlmans, C.W. et al. Exposure to total and methylmercury among pregnant women in Suriname: sources and public health implications. J Expo Sci Environ Epidemiol 31, 117–125 (2021). https://doi.org/10.1038/s41370-020-0233-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41370-020-0233-3
Keywords
This article is cited by
-
Geographic differences in exposures to metals and essential elements in pregnant women living in Suriname
Journal of Exposure Science & Environmental Epidemiology (2023)
-
Total Blood Mercury Predicts Methylmercury Exposure in Fish and Shellfish Consumers
Biological Trace Element Research (2022)
-
Analysis of the Mercury Distribution in Blood as a Potential Tool for Exposure Assessment — Results from Two Artisanal and Small-Scale Gold Mining Areas in Zimbabwe
Biological Trace Element Research (2022)
-
Adequate antenatal care and ethnicity affect preterm birth in pregnant women living in the tropical rainforest of Suriname
BMC Pregnancy and Childbirth (2020)