Abstract
Background
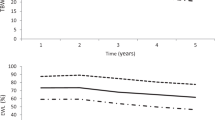
Percentage excess weight loss (%EWL) and percentage total weight loss (%TWL) are used for reporting outcomes after bariatric surgery. However, they are not ideal for comparing outcomes on populations of varied initial body mass index (BMI). This study aimed to validate a recently introduced metric - percentage alterable weight loss (%AWL), after laparoscopic sleeve gastrectomy (LSG) and Roux-en-Y gastric bypass (LRYGB).
Methods
Analysis of weight data of all patients who had undergone LSG and LRYGB until the end of the year 2021. Outcomes for both procedures were analyzed separately. The patients were divided into quartile subgroups Q1 (lowest BMI) to Q4 (highest BMI) and weight loss up to 5 years postoperatively was compared using %EWL, %TWL and %AWL metrics. An intermediary metric was also tested for its effect on the weight loss patterns for both procedures.
Results
The cohort included 1020 LSG and 322 LRYGB patients, with initial mean BMI of 43.5 ± 7.5 and 41.9 ± 8.3 kg/m2, respectively. %EWL significantly favors lower BMI subgroups for both procedures. %TWL is ideal for comparing weight loss during the first 6 months but it then favors higher BMI subgroups beyond 6 months. %AWL with reference BMI of 13 kg/m2 seems the best metric for medium-term comparison of weight loss for LRYGB and an intermediary metric based on BMI 8 kg/m2 provides the best fit for medium-term comparison for LSG.
Conclusions
%TWL is least influenced by initial BMI during short-term follow-up after LSG and LRYGB. For medium-term comparison, %AWL is best suited for LRYGB while an intermediary metric is found to provide the best fit for LSG.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Angrisani L, Santonicola A, Iovino P, Vitiello A, Zundel N, Buchwald H, et al. Bariatric surgery and endoluminal procedures: IFSO worldwide survey 2014. Obes Surg. 2017;27:2279–89.
Hall JC, Watts JM, O’Brien PE, Dunstan RE, Walsh JF, Slavotinek AH, et al. Gastric surgery for morbid obesity. The adelaide study. Ann Surg. 1990;211:419–27.
Mason EE, Amaral J, Cowan GS, Deitel M, Gleysteen JJ, Oria HE. Standards for reporting results. Obes Surg. 1994;4:56–65.
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63.
Ochner CN, Jochner MC, Caruso EA, Teixeira J, Xavier Pi-Sunyer F. Effect of preoperative body mass index on weight loss following obesity surgery. Surg Obes Relat Dis. 2013;9:423–7.
Hatoum IJ, Kaplan LM. Advantages of percent weight loss as a method of reporting weight loss after Roux-en-Y gastric bypass. Obesity. 2013;21:1519–925.
van de Laar AW. Algorithm for weight loss after gastric bypass surgery considering body mass index, gender, and age from the bariatric outcome longitudinal database (BOLD). Surg Obes Relat Dis. 2014;10:55–61.
Park JY, Kim YJ. Efficacy of laparoscopic sleeve gastrectomy in mildly obese patients with body mass index of 30–35 kg/m2. Obes Surg. 2015;25:1351–7.
Brethaeur SA, Kim J, el Chaar M, Papasavas P, Eisenberg D, Rogers A, et al. Standardized outcomes reporting in metabolic and bariatric surgery. Obes Surg. 2015;25:587–606.
Seo DC, Lee CG, Torabi MR, Lohrmann DK. The longitudinal trajectory of post-surgical % total weight loss among middle-aged women who had undergone bariatric surgery. Prev Med Rep. 2017;5:200–4.
van de Laar AW, Dollé MH, de Brauw LM, Bruin SC, Acherman YI. Validating the alterable weight loss (AWL) metric with 2-year weight loss outcome of 500 patients after gastric bypass. Obes Surg. 2014;24:1085–9.
Park JY, Kim YJ. Validation of the alterable weight loss metric in morbidly obese patients undergoing gastric bypass in Korea. Obes Surg. 2018;28:1704–10.
Beisani M, Pereferrer FS, Vilallonga R, López ÓG, López AM. Del Castillo Dejardin D, et.al. Seeking an initial-weight-independent metric in a Mediterranean cohort of gastric bypass patients: the %AWL revisited. Obes Surg. 2021;31:1524–32.
Mechanick JI, Youdim A, Jones DB, Garvey WT, Hurley DL, McMahon M, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient – 2013 update: cosponsored by American association of clinical endocrinologists, The obesity society, and American society for metabolic & bariatric surgery. Obesity (Silver Spring). 2013;21:S1–27.
Cumming G, Fidler F, Vaux DL. Error bars in experimental biology. J Cell Biol. 2007;177:7–11.
Population Trends, 2022. Department of statistics, ministry of trade & industry, Republic of Singapore. ISSN 2591-8028. Available at www.singstat.gov.sg.
National Population Health Survey 2020 (Household Interview and Health Examination). ISBN 978-981-18-1526-3. Epidemiology & disease control division and policy, research & surveillance group, ministry of health and health promotion board, Singapore. Available at www.moh.gov.sg.
van de Laar AW, Emous M, Hazebroek EJ, Boerma EJ, Faneyte IF, Nienhuijs SW. Reporting weight loss 2021: position statement of the Dutch society for metabolic and bariatric surgery (DSMBS). Obes Surg. 2021;31:4607–11.
van de Laar AW, Nienhujis SW, Apers JA, van Rijswijk AS, de Zoete JP, Gadiot RP. The Dutch bariatric weight loss chart: a multicenter tool to assess weight outcome up to 7 years after sleeve gastrectomy and laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2019;15:200–10.
Author information
Authors and Affiliations
Contributions
SSC conceived and designed the analysis, performed the analysis, generated the charts, and wrote the manuscript. SSC, ASYW, AYLN, JLee, PCL, CHL contributed to the data collection. JLin and PCL revised the draft manuscript critically for important intellectual content. All authors were involved in writing the paper and had final approval of the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ching, S.S., Lee, P.C., Lim, C.H. et al. Study on weight loss outcomes after bariatric surgery to determine a metric least influenced by preoperative BMI. Int J Obes 47, 993–999 (2023). https://doi.org/10.1038/s41366-023-01349-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-023-01349-7