Abstract
Introduction
Although most patients with NAFLD are obese or overweight, some are lean with normal BMI. Our aim was to assess differences in clinicopathological profile and liver disease severity among lean and non-lean NAFLD.
Methods
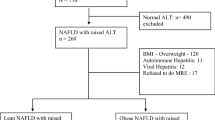
Data of 1040 NAFLD patients over last 10 years was analysed. BMI < 23 kg/m2 categorised lean patients. Non-invasive assessment of steatosis was done by ultrasound and controlled attenuation parameter (CAP) while fibrosis was assessed with FIB-4 and liver stiffness measurement (LSM). FibroScan-AST (FAST) score was used for non-invasive prediction of NASH with significant fibrosis. Histology was reported using NASH-CRN system.
Results
149 (14.3%) patients were lean while 891 (85.7%) patients were non-lean. Diabetes mellitus [25 (16.7%) vs 152 (17.05%), p > 0.99], elevated triglycerides [81 (54.3%) vs 525 (58.9%), p = 0.33] and low HDL [71(47.6%) vs 479(53.7%), p = 0.18] were observed in a similar proportion. Lean patients were less likely to have central obesity [72 (48.3%) vs 788 (88.4%), p < 0.001], hypertension [16 (10.7%) vs 239(26.8%), p < 0.001] and metabolic syndrome [21 (14.09%) vs 290 (32.5%), p < 0.001]. No difference in steatosis assessment was noted using ultrasound (p = 0.55) or CAP (0.11). FAST [0.38 (0.18–0.66) vs 0.39 (0.27–0.73), p = 0.53], FIB-4 [1.08 (0.65–1.91) vs 1.09 (0.66–1.94), p = 0.94] and LSM [6.1 (4.8-7.9) vs 6.2 (4.7–8.6), p = 0.19) were similar.
Liver biopsy was available in 149 patients [lean: 19 (12.7%), non-lean: 130 (87.3%)]. There was no difference in the number of patients with NASH [4 (21.05%) vs 20 (15.3%), p = 0.51], significant fibrosis [2 (10.5%) vs 32 (24.6%), p = 0.25] or advanced fibrosis [1 (5.26%) vs 18 (13.84%), p = 0.47].
Conclusion
Although metabolic co-morbidities are less common, there is no difference in liver disease severity among both groups.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Shalimar, Elhence A, Bansal B, Gupta H, Anand A, Singh T, et al. Prevalence of non-alcoholic fatty liver disease in india: a systematic review and meta-analysis, J Clin Exp Hepatol. 2021. https://doi.org/10.1016/j.jceh.2021.11.010.
Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84. https://doi.org/10.1002/hep.28431.
De A, Duseja A. Natural history of simple steatosis or nonalcoholic fatty liver. J Clin Exp Hepatol. 2020;10:255–62. https://doi.org/10.1016/j.jceh.2019.09.005.
Ekstedt M, Nasr P, Kechagias S. Natural history of NAFLD/NASH. Curr Hepatol Rep. 2017;16:391–7. https://doi.org/10.1007/s11901-017-0378-2.
Young S, Tariq R, Provenza J, Satapathy SK, Faisal K, Choudhry A, et al. Prevalence and profile of nonalcoholic fatty liver disease in lean adults: systematic review and meta-analysis. Hepatol Commun. 2020;4:953–72. https://doi.org/10.1002/hep4.1519.
Ye Q, Zou B, Yeo YH, Li J, Huang DQ, Wu Y, et al. Global prevalence, incidence, and outcomes of non-obese or lean non-alcoholic fatty liver disease: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5:739–52. https://doi.org/10.1016/S2468-1253(20)30077-7.
Alam S, Eslam M, Skm Hasan N, Anam K, Chowdhury MAB, Khan MAS, et al. Risk factors of nonalcoholic fatty liver disease in lean body mass population: a systematic review and meta-analysis. JGH Open. 2021;5:1236–49. https://doi.org/10.1002/jgh3.12658.
Kumar R, Rastogi A, Sharma MK, Bhatia V, Garg H, Bihari C, et al. Clinicopathological characteristics and metabolic profiles of non-alcoholic fatty liver disease in Indian patients with normal body mass index: do they differ from obese or overweight non-alcoholic fatty liver disease? Indian J Endocrinol Metab. 2013;17:665–71. https://doi.org/10.4103/2230-8210.113758.
Alam S, Gupta UD, Alam M, Kabir J, Chowdhury ZR, Alam AK. Clinical, anthropometric, biochemical, and histological characteristics of nonobese nonalcoholic fatty liver disease patients of Bangladesh. Indian J Gastroenterol. 2014;33:452–7. https://doi.org/10.1007/s12664-014-0488-5.
Directorate General of Health Services, MOHFW, Government of India. Operational guidelines for integration of non-alcoholic fatty liver disease (NAFLD) with NPCDCS. 2021. https://main.mohfw.gov.in/newshighlights-42.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. STROBE Initiative. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–7.
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–421..
Misra A, Misra R, Wijesuriya M, Banerjee D. The metabolic syndrome in South Asians: continuing escalation & possible solutions. Indian J Med Res. 2007;125:345–54.
Duseja A, Singh SP, Saraswat VA, Acharya SK, Chawla YK, Chowdhury S, et al. Non-alcoholic fatty liver disease and metabolic syndrome-position paper of the Indian National Association for the study of the liver, endocrine society of India, Indian college of cardiology and Indian society of gastroenterology. J Clin Exp Hepatol. 2015;5:51–68.
Karlas T, Petroff D, Sasso M, Fan JG, Mi YQ, de Lédinghen V, et al. Individual patient data meta-analysis of controlled attenuation parameter (CAP) technology for assessing steatosis. J Hepatol. 2017;66:1022–30.
Newsome PN, Sasso M, Deeks JJ, Paredes A, Boursier J, Chan WK, et al. FibroScan-AST (FAST) score for the non-invasive identification of patients with non-alcoholic steatohepatitis with significant activity and fibrosis: a prospective derivation and global validation study. Lancet Gastroenterol Hepatol. 2020;5:362–73.
De A, Keisham A, Mishra S, Mehta M, Verma N, Premkumar M, et al. FibroScan-AST (FAST) score for nonalcoholic steatohepatitis - validation in an Indian Cohort. J Clin Exp Hepatol. 2022;12:440–7. https://doi.org/10.1016/j.jceh.2021.06.008.
European Association for the Study of the Liver. Electronic address: easloffice@easloffice.eu; Clinical Practice Guideline Panel; Chair; EASL Governing Board representative; Panel members. EASL Clinical Practice Guidelines on non-invasive tests for evaluation of liver disease severity and prognosis - 2021 update. J Hepatol. 2021;75:659–89. https://doi.org/10.1016/j.jhep.2021.05.025.
Papatheodoridi M, Hiriart JB, Lupsor-Platon M, Bronte F, Boursier J, Elshaarawy O, et al. Refining the Baveno VI elastography criteria for the definition of compensated advanced chronic liver disease. J Hepatol. 2021;74:1109–16. https://doi.org/10.1016/j.jhep.2020.11.050.
Kleiner DE, Brunt EM, Van Natta M, Behling C, Contos MJ, Cummings OW, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–21.
Bedossa P, Poitou C, Veyrie N, Bouillot J-L, Basdevant A, Paradis V, et al. Histopathological algorithm and scoring system for evaluation of liver lesions in morbidly obese patients. Hepatology. 2012;56:1751–9.
Duseja A, Singh SP, Mehta M, Shalimar, Venkataraman J, Mehta V, et al. Clinicopathological profile and outcome of a large cohort of patients with nonalcoholic fatty liver disease from South Asia: Interim Results of the Indian Consortium on Nonalcoholic Fatty Liver Disease. Metab Syndr Relat Disord. 2022;20:166–73. https://doi.org/10.1089/met.2021.0104.
De A, Duseja A. Nonalcoholic fatty liver disease: Indian perspective. Clin Liver Dis. 2021;18:158–63. https://doi.org/10.1002/cld.1141.
Duseja A, Singh SP, De A, Madan K, Rao PN, Shukla A, et al. Indian National Association for Study of the Liver (INASL) guidance paper on nomenclature, diagnosis and treatment of nonalcoholic fatty liver disease (NAFLD). J Clin Exp Hepatol. 2022. https://doi.org/10.1016/J.JCEH.2022.11.014.
Ahmed OT, Gidener T, Mara KC, Larson JJ, Therneau TM, Allen AM. Natural history of nonalcoholic fatty liver disease with normal body mass index: a population-based study. Clin Gastroenterol Hepatol. 2022;20:1374–81.e6. https://doi.org/10.1016/j.cgh.2021.07.016.
Younes R, Govaere O, Petta S, Miele L, Tiniakos D, Burt A, et al. Caucasian lean subjects with non-alcoholic fatty liver disease share long-term prognosis of non-lean: time for reappraisal of BMI-driven approach? Gut. 2022;71:382–90. https://doi.org/10.1136/gutjnl-2020-322564.
Vendhan R, Amutha A, Anjana RM, Unnikrishnan R, Deepa M, Mohan V. Comparison of characteristics between nonobese and overweight/obese subjects with nonalcoholic fatty liver disease in a South Indian population. Diabetes TechnolTher. 2014;16:48–55. https://doi.org/10.1089/dia.2013.0165.
Anand A, Elhence A, Vaishnav M, Singh AA, Rajput MS, Banyal V, et al. FibroScan-aspartate aminotransferase score in an Asian cohort of non-alcoholic fatty liver disease and its utility in predicting histological resolution with bariatric surgery. J Gastroenterol Hepatol. 2021;36:1309–16. https://doi.org/10.1111/jgh.15358.
Sookoian S, Pirola CJ. Systematic review with meta-analysis: the significance of histological disease severity in lean patients with nonalcoholic fatty liver disease. Aliment PharmacolTher. 2018;47:16–25. https://doi.org/10.1111/apt.14401.
Akyuz U, Yesil A, Yilmaz Y. Characterization of lean patients with nonalcoholic fatty liver disease: potential role of high hemoglobin levels. Scand J Gastroenterol. 2015;50:341–6. https://doi.org/10.3109/00365521.2014.983160.
Fracanzani AL, Petta S, Lombardi R, Pisano G, Russello M, Consonni D, et al. Liver and cardiovascular damage in patients with lean nonalcoholic fatty liver disease, and association with visceral obesity. Clin Gastroenterol Hepatol. 2017;15:1604–11.e1. https://doi.org/10.1016/j.cgh.2017.04.045.
Honda Y, Yoneda M, Kessoku T, Ogawa Y, Tomeno W, Imajo K, et al. Characteristics of non-obese non-alcoholic fatty liver disease: effect of genetic and environmental factors. Hepatol Res. 2016;46:1011–8. https://doi.org/10.1111/hepr.12648.
Leung JC, Loong TC, Wei JL, Wong GL, Chan AW, Choi PC, et al. Histological severity and clinical outcomes of nonalcoholic fatty liver disease in nonobese patients. Hepatology. 2017;65:54–64. https://doi.org/10.1002/hep.28697.
Margariti A, Deutsch M, Manolakopoulos S, Tiniakos D, Papatheodoridis GV. The severity of histologic liver lesions is independent of body mass index in patients with nonalcoholic fatty liver disease. J Clin Gastroenterol. 2013;47:280–6. https://doi.org/10.1097/MCG.0b013e31826be328.
Hagström H, Nasr P, Ekstedt M, Hammar U, Stål P, Hultcrantz R, et al. Risk for development of severe liver disease in lean patients with nonalcoholic fatty liver disease: a long-term follow-up study. Hepatol Commun. 2017;2:48–57. https://doi.org/10.1002/hep4.1124.
Meeuwsen S, Horgan GW, Elia M. The relationship between BMI and percent body fat, measured by bioelectrical impedance, in a large adult sample is curvilinear and influenced by age and sex. Clin Nutr. 2010;29:560–6. https://doi.org/10.1016/j.clnu.2009.12.011.
Acknowledgements
Part of the manuscript was presented as poster at the annual conference of the Indian National Association for Study of the Liver (INASL) 2022.
Author information
Authors and Affiliations
Contributions
ArD: conceptualisation, patient recruitment, data analysis and manuscript writing; MM: data collection and analysis; PS: data collection; NB: manuscript writing; SM: data collection; AsD: histopathology assessment; AD: conceptualisation, patient recruitment, data curation and critical revision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
De, A., Mehta, M., Singh, P. et al. Lean Indian patients with non-alcoholic fatty liver disease (NAFLD) have less metabolic risk factors but similar liver disease severity as non-lean patients with NAFLD. Int J Obes 47, 986–992 (2023). https://doi.org/10.1038/s41366-023-01346-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-023-01346-w
This article is cited by
-
Lifestyle intervention for metabolic dysfunction-associated fatty liver disease: a 24-h integrated behavior perspective
Hepatology International (2024)