Abstract
Background
Bardet–Biedl syndrome (BBS) is a rare autosomal recessive syndromic obesity of childhood onset among many other features. To date, the excess risk of metabolic complications of severe early-onset obesity in BBS remains controversial. In-depth investigation of adipose tissue structure and function with detailed metabolic phenotype has not been investigated yet.
Objective
To investigate adipose tissue function in BBS.
Design
A prospective cross-sectional study.
Main outcome measure
To determine if there are differences in insulin resistance, metabolic profile, adipose tissue function and gene expression in patients with BBS compared to BMI-matched polygenic obese controls.
Method
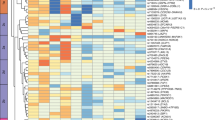
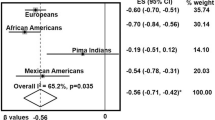
9 adults with BBS and 10 controls were recruited from the national centre for BBS, Birmingham, UK. An in-depth study of adipose tissue structure and function along with insulin sensitivity was performed using hyperinsulinemic-euglycemic clamp studies, adipose tissue microdialysis, histology and RNA sequencing, and measurement of circulating adipokines and inflammatory biomarkers.
Results
Adipose tissue structure, gene expression and in vivo functional analysis between BBS and polygenic obesity cohorts were similar. Using hyperinsulinemic-euglycemic clamp and surrogate markers of insulin resistance, we found no significant differences in insulin sensitivity between BBS and obese controls. Furthermore, no significant changes were noted in an array of adipokines, cytokines, pro-inflammatory markers and adipose tissue RNA transcriptomic.
Conclusion
Although childhood-onset extreme obesity is a feature of BBS, detailed studies of insulin sensitivity and adipose tissue structure and function are similar to common polygenic obesity. This study adds to the literature by suggesting that it is the quality and quantity of adiposity not the duration that drives the metabolic phenotype.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated during and analysed during the current study are available with the corresponding author. We will be happy to share anonymised data on reasonable request.
References
Heon E, Kim G, Qin S, Garrison JE, Tavares E, Vincent A, et al. Mutations in C8ORF37 cause Bardet Biedl syndrome (BBS21). Hum Mol Genet. 2016;25:2283–94.
Forsythe E, Beales PL. Bardet-Biedl syndrome. Eur J Hum Genet. 2013;21:8–13.
Moore SJ, Green JS, Fan Y, Bhogal AK, Dicks E, Fernandez BA, et al. Clinical and genetic epidemiology of Bardet-Biedl syndrome in Newfoundland: a 22-year prospective, population-based, cohort study. Am J Med Genet A. 2005;132A:352–60.
Farag TI, Teebi AS. High incidence of Bardet Biedl syndrome among the Bedouin. Clin Genet. 1989;36:463–4.
Pomeroy J, Krentz AD, Richardson JG, Berg RL, VanWormer JJ, Haws RM. Bardet-Biedl syndrome: weight patterns and genetics in a rare obesity syndrome. Pediatr Obes. 2021;16:e12703.
Muller J, Stoetzel C, Vincent MC, Leitch CC, Laurier V, Danse JM, et al. Identification of 28 novel mutations in the Bardet-Biedl syndrome genes: the burden of private mutations in an extensively heterogeneous disease. Hum Genet. 2010;127:583–93.
Cardenas-Rodriguez M, Badano JL. Ciliary biology: understanding the cellular and genetic basis of human ciliopathies. Am J Med Genet C Semin Med Genet. 2009;151C:263–80.
Baker K, Beales PL. Making sense of cilia in disease: the human ciliopathies. Am J Med Genet C Semin Med Genet. 2009;151C:281–95.
Imhoff O, Marion V, Stoetzel C, Durand M, Holder M, Sigaudy S, et al. Bardet-Biedl syndrome: a study of the renal and cardiovascular phenotypes in a French cohort. Clin J Am Soc Nephrol. 2011;6:22–9.
Badano JL, Mitsuma N, Beales PL, Katsanis N. The ciliopathies: an emerging class of human genetic disorders. Annu Rev Genomics Hum Genet. 2006;7:125–48.
O’Dea D, Parfrey PS, Harnett JD, Hefferton D, Cramer BC, Green J. The importance of renal impairment in the natural history of Bardet-Biedl syndrome. Am J Kidney Dis. 1996;27:776–83.
Beales PL, Elcioglu N, Woolf AS, Parker D, Flinter FA. New criteria for improved diagnosis of Bardet-Biedl syndrome: results of a population survey. J Med Genet. 1999;36:437–46.
Mujahid S, Hunt KF, Cheah YS, Forsythe E, Hazlehurst JM, Sparks K, et al. The endocrine and metabolic characteristics of a large bardet-biedl syndrome clinic population. J Clin Endocrinol Metab. 2018;103:1834–41.
Feuillan PP, Ng D, Han JC, Sapp JC, Wetsch K, Spaulding E, et al. Patients with Bardet-Biedl syndrome have hyperleptinemia suggestive of leptin resistance. J Clin Endocrinol Metab. 2011;96:E528–535.
Stefan N, Häring H-U, Schulze MB. Metabolically healthy obesity: the low-hanging fruit in obesity treatment? Lancet Diabetes Endocrinol. 2018;6:249–58.
Baig S, Veeranna V, Bolton S, Edwards N, Tomlinson JW, Manolopoulos K, et al. Treatment with PBI-4050 in patients with Alström syndrome: study protocol for a phase 2, single-Centre, single-arm, open-label trial. BMC Endocr Disord. 2018;18:88.
Castéra L, Foucher J, Bernard PH, Carvalho F, Allaix D, Merrouche W, et al. Pitfalls of liver stiffness measurement: a 5-year prospective study of 13,369 examinations. Hepatology. 2010;51:828–35.
Galarraga M, Campión J, Muñoz-Barrutia A, Boqué N, Moreno H, Martínez JA, et al. Adiposoft: automated software for the analysis of white adipose tissue cellularity in histological sections. J Lipid Res. 2012;53:2791–6.
Dobin A, Davis CA, Schlesinger F, Drenkow J, Zaleski C, Jha S, et al. STAR: ultrafast universal RNA-seq aligner. Bioinformatics. 2013;29:15–21.
Othonos N, Marjot T, Woods C, Hazlehurst JM, Nikolaou N, Pofi R, et al. Co-administration of 5α-reductase inhibitors worsens the adverse metabolic effects of prescribed glucocorticoids. J Clin Endocrinol Metab. 2020;105:e3316–28.
Søndergaard E, Espinosa De Ycaza AE, Morgan-Bathke M, Jensen MD. How to measure adipose tissue insulin sensitivity. J Clin Endocrinol Metab. 2017;102:1193–99.
Bel Lassen P, Charlotte F, Liu Y, Bedossa P, Le Naour G, Tordjman J, et al. The FAT Score, a Fibrosis Score of Adipose Tissue: Predicting Weight-Loss Outcome After Gastric Bypass. J Clin Endocrinol Metab. 2017;102:2443–53.
Marion V, Mockel A, De Melo C, Obringer C, Claussmann A, Simon A, et al. BBS-induced ciliary defect enhances adipogenesis, causing paradoxical higher-insulin sensitivity, glucose usage, and decreased inflammatory response. Cell Metab. 2012;16:363–77.
Anosov M, Birk R. Bardet-Biedl syndrome obesity: BBS4 regulates cellular ER stress in early adipogenesis. Mol Genet Metab. 2019;126:495–503.
Aksanov O, Green P, Birk RZ. BBS4 directly affects proliferation and differentiation of adipocytes. Cell Mol Life Sci. 2014;71:3381–92.
Forti E, Aksanov O, Birk RZ. Temporal expression pattern of Bardet-Biedl syndrome genes in adipogenesis. Int J Biochem Cell Biol. 2007;39:1055–62.
Lodh S, Hostelley TL, Leitch CC, O’Hare EA, Zaghloul NA. Differential effects on β-cell mass by disruption of Bardet–Biedl syndrome or Alstrom syndrome genes. Hum Mol Genet. 2016;25:57–68.
Wang JS, Lee WJ, Lee IT, Lin SY, Lee WL, Liang KW, et al. Association between serum adipsin levels and insulin resistance in subjects with various degrees of glucose intolerance. J Endocr Soc. 2018;3:403–10.
Aliasghari F, Izadi A, Jabbari M, Imani B, Gargari BP, Asjodi F, et al. Are vaspin and omentin-1 related to insulin resistance, blood pressure and inflammation in NAFLD patients? J Med Biochem. 2018;37:470–5.
Seo S, Guo D-F, Bugge K, Morgan DA, Rahmouni K, Sheffield VC. Requirement of Bardet-Biedl syndrome proteins for leptin receptor signaling. Hum Mol Genet. 2009;18:1323–31.
Davis RE, Swiderski RE, Rahmouni K, Nishimura DY, Mullins RF, Agassandian K, et al. A knockin mouse model of the Bardet-Biedl syndrome 1 M390R mutation has cilia defects, ventriculomegaly, retinopathy, and obesity. Proc Natl Acad Sci USA. 2007;104:19422–7.
Rahmouni K, Fath MA, Seo S, Thedens DR, Berry CJ, Weiss R, et al. Leptin resistance contributes to obesity and hypertension in mouse models of Bardet-Biedl syndrome. J Clin Invest. 2008;118:1458–67.
Guo DF, Cui H, Zhang Q, Morgan DA, Thedens DR, Nishimura D, et al. The BBSome controls energy homeostasis by mediating the transport of the leptin receptor to the plasma membrane. PLoS Genet. 2016;12:e1005890.
Vaisse C, Reiter JF, Berbari NF. Cilia and obesity. Cold Spring Harb Perspect Biol. 2017;9:a028217.
Loos RJF, Yeo GSH. The genetics of obesity: from discovery to biology. Nat Rev Genet. 2022;23:120–33.
Acknowledgements
We acknowledge the support of BBS society. The Research was carried out at the National Institute for Health Research (NIHR)/Welcome Trust Birmingham Clinical Research Facility. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. Funds were also obtained from French National Agency of research (ANR, Captor) and French foundation for medical research (FRM) (to KC and PBL).
Author information
Authors and Affiliations
Contributions
TH and RS conceived the study and drafted the study protocol. SB drafted the manuscript. SB and Vishy Veeranna (VV), Inherited Metabolic Disorders Research Charge Nurse, were involved in data collection and running of the study. All authors made contributions to data generation and analysis and writing and reviewing the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Baig, S., Wanninayake, S., Foggensteiner, L. et al. Adipose tissue function and insulin sensitivity in syndromic obesity of Bardet-Biedl syndrome. Int J Obes 47, 382–390 (2023). https://doi.org/10.1038/s41366-023-01280-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-023-01280-x