Abstract
Background
Increased weight-related stigma during the COVID-19 pandemic has amplified the need to minimise the impacts on mental wellbeing. We investigated the relationship between the perceived changes in the representation of obesity in the media and mental wellbeing during the pandemic in a sample of people with obesity across 10 European countries. We also investigated the potential moderating effect of loneliness.
Methods
Between September to December 2020 during the COVID-19 pandemic, participants reported data on demographics, mental wellbeing (measured by World Health Organisation Five Wellbeing Index and Patient Health Questionaire-4), loneliness (measured by De Jong Gierveld short scale), and perceived change in the representation of obesity in media (measured by a study-specific question) using the online, cross-sectional EURopean Obesity PatiEnt pANdemic Survey (EUROPEANS). Data were analysed using linear mixed-effects models, controlling for age, gender, body mass index, and shielding status, with random incept for country.
Results
The survey was completed by 2882 respondents. Most identified as female (56%) and reported their ethnicity as White or White-mix (92%). The total sample had a mean age of 41 years and a BMI of 35.4 kg/m2. During the peak of the pandemic, compared to pre-pandemic, perceiving more negative representation of people with obesity on social media was associated with worse psychological distress, depression, and wellbeing. Perceiving more positive representation, compared to no change in representation, of people with obesity on television was associated with greater wellbeing, yet also higher psychological distress and anxiety. Loneliness, as a moderator, explained ≤0.3% of the variance in outcomes in any of the models.
Conclusions
Perceiving negative representation of obesity on social media was associated with poorer mental wellbeing outcomes during the pandemic; positive representation on television was associated with both positive and negative mental wellbeing outcomes. We encourage greater media accountability when representing people with obesity.
Similar content being viewed by others
Introduction
Many organisations recognise obesity as a disease, including the American Medical Association, Canadian Obesity Network, World Obesity Federation, and World Health Organisation [1,2,3,4]. The European Association for the Study of Obesity (EASO) describes obesity as an adiposity-based chronic disease which is frequent, serious, complex, relapsing, and chronic [5]. Many factors influence the development of obesity, including genetics, gene-lifestyle interactions, and the obesogenic environment [6]. However, societal beliefs and attitudes commonly deem obesity to be due to individual choices and behaviour, resulting in people with obesity often being stereotyped as lazy, greedy, unmotivated, and lacking willpower [7, 8]. These harmful beliefs and attitudes are known as weight-related stigma [9, 10]. Experiences of weight-related stigma are associated with a deterioration in mental wellbeing in people with obesity, including psychological distress, increased social isolation and exclusion, and avoidance of psychologically supportive activities (e.g., healthcare services, physical activity) [7, 9, 11, 12]. Addressing weight-related stigma requires action across multiple levels of influence, including government and policymakers, and is likely to be a long-term process [13, 14]. However, given the short-term impacts of experiencing weight-related stigma, more immediate action is required to mitigate the risk of harm to the mental wellbeing of people with obesity.
Research suggests that the COVID-19 pandemic may have had a negative impact on people with obesity in terms of health-related behaviours and mental wellbeing [15,16,17,18,19,20]. Multiple factors may have contributed to worsening mental wellbeing in this group, including fear of contracting COVID-19 and potential severity of symptoms, shielding and social isolation, and reduced/no access to services and support [21]. In addition, extensive media coverage and public discourse on television and social media focused on the links between obesity and COVID-19 symptom severity, which many with obesity may have found stigmatising [21, 22]. When covering obesity during the pandemic, the media has been accused of using stigmatising language, promoting a blame culture, and employing tactics to instil both shame and fear in those with obesity [23]. Such a culture of additional stigma and blame is a risk for mental wellbeing in people with obesity, which may occur as a result of internalised blame, shame, and self-stigma [24, 25]. The positioning of media within society – specifically its highly persuasive and influential effect on social norms, beliefs, and attitudes—is thought to play a role in the relationship between media and mental wellbeing in those living with obesity [26,27,28,29]. Researchers suggest that the media may exacerbate weight stigma through reinforcing the idea of the ‘ideal’ body shape or size, resulting in the devaluation of those with overweight or obesity and, consequentially, reduced mental wellbeing of these individuals. For example, the media often portrays a person with a thin or muscular physique receiving positive reinforcement and feedback, whilst a person with overweight or obesity is ridiculed and demeaned via negative and degrading comments and weight-related “humour” [26,27,28,29].
Therefore, given the short-term adverse impacts of experiencing weight-related stigma, more immediate action is required to mitigate the risk of harm to the mental wellbeing of people with obesity. Some factors, such as loneliness (or lack thereof), may influence the effect of weight-related stigma on the mental wellbeing of people with obesity. The introduction of COVID-19 restrictions (e.g., stay at home orders and social distancing guidelines) reduced individuals’ access to their usual support networks [18,19,20], with recent research showing that feelings of loneliness were substantially higher during the pandemic [30,31,32,33]. Loneliness has been described as “a subjective, negative feeling related to the deficient social relations” and “a feeling of disconnectedness or isolation” [34]. De Jong proposed that loneliness is multidimensional, including emotional (i.e., absence of an intimate relationship) and social loneliness (i.e., absence of a broader social network) [35, 36]. Greater feelings of loneliness may reduce a persons’ ability to regulate emotions and manage the impact of a distressing event, such as weight-related stigma, on their mental wellbeing [37,38,39]. Alternatively, lower feelings of loneliness may be protective of mental wellbeing in response to experiences such as weight-related stigma. Loneliness during the pandemic may have been particularly important to consider when explaining poor mental wellbeing among individuals living with obesity as, for example, in the United Kingdom many people with more complex obesity were advised to shield and to socially isolate from other members of the population [40].
We investigated the relationship between the perceived representation of obesity in the media (as an indicator of perceived experiences of weight-related stigma) and mental wellbeing during the COVID-19 pandemic in a sample of people with obesity across 10 European countries. We proposed that loneliness may moderate the relationship between perceived experiences of weight-related stigma and mental wellbeing. Specifically, we anticipated that the relationship between perceived experiences of weight-related stigma and poor mental wellbeing (compared to good mental wellbeing) would be most pronounced in people with higher as opposed to lower levels of loneliness. We viewed mental wellbeing as a broad spectrum spanning poor mental health and disorders (e.g., low mood, clinical depression, anxiety) through to positive mental wellbeing. Defining mental wellbeing in this way is associated with reduced stigma, and enables the investigation of a broader range of mental wellbeing outcomes [41,42,43].
Methods
Data source
EURopean Obesity PatiEnt pANdemic Survey (EUROPEANS) was a large international consortium study commissioned to understand the lived experience of obesity during the COVID-19 pandemic. Data from the EUROPEANS study were collected from September 3rd to December 19th 2020. The survey was created using QualtricsTM (a commercial survey sampling and administrative company). Participants were recruited using several methods: (1) through QualtricsTM using their existing participant recruitment panels, (2) inviting individuals who had previously opted in to be contacted for research studies (i.e., notified through emails, applications & text message notifications), and (3) via several patient-led obesity advocacy organisations (e.g., European Collaboration for People with obesity (ECPO)). Participants were eligible to take part in the study if they had the following characteristics: self-reported body mass index [BMI] ≥ 30 kg/m2, aged ≥18 years, and a resident of one of the specified 10 European countries. We also stratified recruitment by age in years (18–30, 30–50, 50+). Participants were invited to take part and opted in by activating the EUROPEANS survey link which directied them to the study information, consent pages, and survey instrument. Ineligible respondents were immediately exited from the survey after providing a response that did not meet the eligibility criteria or exceeded set quotas (e.g., did not provide consent, BMI was outside the threshold). The survey was completed directly on the QualtricsTM portal and participants received an honorarium (e.g., reimbursement for their time via cash, gift cards, redeemable points, vouchers).
To ensure data quality, responses were checked for (i) speeding (i.e., respondents with a survey duration of ≤ one-third of the median duration of the survey) and (ii) poor quality [e.g., selecting the first option for every question, bad verbatims (answering open-end questions by way of keyboard banging or typing illogical gibberish answers), duplicate responses and bots (software created to take surveys multiple times for incentives), incomplete data sets] (see Supplementary Materials for greater detail). Respondents who failed any of these quality checks were excluded from the final sample. The study was approved by the University of Liverpool Research Ethics Committee (ref no: 7932 - EUROPEANS study). Written informed consent was obtained electronically from each participant.
Participant eligibility
Upon clicking on the EUROPEANS survey link, individuals provided informed consent and were asked to complete a self-screening tool to assess their eligibility. Eligibility criteria were: people who were living with obesity during COVID-19 who had a self-reported BMI ≥ 30 kg/m2, aged 18 years and above, and were a resident of one of the following countries at the time of completing the survey: England, Greece, Germany, France, Sweden, Israel, Portugal, Italy, Denmark and Spain. The number of participants recruited from each country ranged from 276 to 297.
Outcomes
The survey collected self-reported demographic information from participants. Pertinent to this study, participants self-reported gender, ethnicity, BMI, and shielding status. The survey collected information about weight management, exposure to media, perceived change in the representation of obesity in media, health behaviours, emotional wellbeing, food security, and COVID-19 exposure. In the following sections, we detail the outcomes relevant to the present study. Prefer not to say options were included for all questions.
Perceived changes in the representation of people with obesity in the media
Participants self-reported whether they perceived a change in the representation of people with obesity during the self-defined peak exposure of the outbreak compared to before the COVID-19 pandemic. Participants reported whether they perceived more positive representation, more negative representation, or no change in representation on (i) television and (ii) social media (See Supplementary Materials for specific question wording). Self-reported perceived changes in the representation of people with obesity in the media was used as an indicator of perceived experiences of weight stigma (i.e., perceiving more negative change in media representation was interpreted as experiencing a higher level of weight-related stigma).
Depression and anxiety
The Patient Health Questionnaire-4 (PHQ-4) was used as a brief measure of depression and anxiety symptoms over the previous 2 weeks [44]. The PHQ-4 is a 4-item, 4-point self-report Likert scale consisting of 2-items for depression and 2-items for anxiety. Higher PHQ-4 scores indicate a greater burden of depression and anxiety symptoms. It is important to note that the PHQ-4 is not diagnostic, yet can be an indicator of symptom burden [44, 45]. Evidence supports the reliability and validity of this very brief scale to measure depression and anxiety symptoms [44, 45]. In the current sample, the full scale had good reliability (McDonald’s omega (ω) = 0.91). As both subscales consist of two items, reliability was calculated using the Spearman–Browne coefficient [46]; both had good reliability (anxiety rsb = 0.87, depression rsb = 0.82).
Psychological wellbeing
The World Health Organisation Five Wellbeing Index (WHO-5) is a short self-report measure of subjective psychological wellbeing over the previous 2 weeks [47]. It consists of five items on a 5-point Likert scale, with higher scores representing better psychological wellbeing. Evidence from a systematic review supports the validity of the measure and reports that the scale has been used successfully across a wide range of study fields [47]. In the current sample, internal reliability was good with McDonald’s omega (ω) of 0.93 [48].
Loneliness
The De Jong Gierveld (DJG) short scale is a 6-item measure of overall, emotional, and social loneliness. Emotional loneliness relates to the absence of an intimate relationship, whilst social loneliness refers to the absence of a broader social network [35, 36]. The items are answered on a 5-point Likert scale about respondents’ experiences over the previous 2 weeks. Higher scores on the De Jong Gierveld short-scale represent a greater degree of loneliness. Previous research has shown the measure to be a reliable and valid scale [35, 36]. In the current sample, internal reliability was good with ω of 0.87.
Statistical analysis
Statistical analyses were performed using R version 4.0.5 (Vienna, Austria). Data were analysed using linear mixed-effects models, with total distress (total PHQ score with subscales for depression and anxiety symptoms) or wellbeing as outcome variables. Perceived change in the representation of obesity on social media and TV (positive change/no change/negative change) were used as explanatory variables, whilst age (years), gender (male vs. female), BMI (kg/m2), shielding (yes vs. no), socioeconomic status (education status), ethnicity (White vs. BAME), and total loneliness (total score) were control variables. In all models, we added a random intercept for country which significantly improved the fit compared to the models without random effects for all outcomes (Χ2 (1) >19.88, p < 0.001, Akaike’s Information Criterion (AIC) differences >17).
We ran the models with the control variables and then compared the fit of these control models to those with perceived change in the representation of obesity on social media and television added; in all models, the inclusion of the perceived change in representation variables facilitated better fit (Table 1). The two perceived change in representation variables (i.e., social media and television) were added as a fixed effect with “no change” used as the reference group. Residuals had a normal distribution and there was no evidence of multicollinearity (all variance inflation factors (VIFs) <2.89). As there was some evidence for a small degree of heteroscedasticity in the total distress (total PHQ score) models, we re-ran all models with robust standard errors (RSE). The pattern of results was identical (see Tables S1–S3 in Supplementary Materials for models with RSE).
To explore the effect of loneliness as a moderator of the impact of perceived representation on distress, we computed interaction terms between loneliness (mean-centred) and dummy-coded “more negative” and ‘more positive representation’ for both television and social media. These were added to the regression models described in “Association of changes in the perceived representation of people with obesity on television before and during COVID-19 with mental wellbeing” and “Association of perceived changes in the representation of people with obesity on social media before and during COVID-19 with mental wellbeing”.
Results
Participant characteristics
In total, 2882 adults with obesity completed the EUROPEANS survey. Fifty-six percent of survey respondents identified as female, and the total sample had a mean age of 40.6 years and BMI of 35.4 kg/m2. The majority of survey respondents reported their ethnicity as White or a White-mix (92%). Table 2 presents further details of participant characteristics. Participant characteristics for key study outcomes by country of residence are presented in Table S4 in the Supplementary Materials.
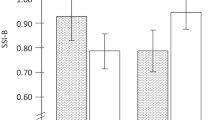
Association of changes in the perceived representation of people with obesity on television before and during COVID-19 with mental wellbeing
Compared to before COVID-19, perceiving more negative representation of people with obesity on television during peak exposure of the outbreak was not associated with depression symptoms (B 0.09, 95% CI: −0.13, 0.31), anxiety symptoms (B 0.19, 95% CI: −0.04, 0.41), or wellbeing (B 0.99, 95% CI: −1.79, 3.78) when compared to perceiving no change in representation (Table 3). Conversely, compared to before COVID-19, perceiving more positive representation of people with obesity on television during peak exposure of the outbreak was associated with higher levels of anxiety symptoms (B 0.26; 95% CI: 0.06, 0.46) and wellbeing (B 4.52; 95% CI: 2.01, 7.02) when compared to perceiving no change in representation (Table 3).
When compared to before COVID-19, perceiving more negative representation of people with obesity on television during peak exposure of the outbreak was not associated with total distress when compared to perceiving no change in representation (B 0.27, 95% CI: −0.13, 0.68) (Table S5 in Supplementary materials). Conversely, compared to before COVID-19, perceiving more positive representation of people with obesity on television during peak exposure of the outbreak was associated with higher levels of total distress (B 0.45; 95% CI: 0.09, 0.81) when compared to perceiving no change in representation (Table S5 in Supplementary Materials). Tables S6–8 in the Supplementary Materials present the effect of the control variables on the models.
Association of perceived changes in the representation of people with obesity on social media before and during COVID-19 with mental wellbeing
Compared to before COVID-19, perceiving more negative representation of people with obesity on social media during peak exposure of the outbreak was associated with higher levels of depression (B 0.50; 95% CI: 0.29, 0.71) and anxiety symptoms (B 0.31; 95% CI: 0.10, 0.52), and lower levels of wellbeing (B −3.52; 95% CI: −6.19, −0.86) when compared to perceiving no change in representation (Table 3). Conversely, compared to before COVID-19, perceiving more positive representation of people with obesity on social media during peak exposure of the outbreak was not associated with changes in depression symptoms, anxiety symptoms, or wellbeing when compared to perceiving no change in representation (Table 3).
When compared to before COVID-19, perceiving more negative representation of people with obesity on social media during peak exposure of the outbreak was associated with higher levels of total distress (B 0.8; 95% CI: 0.42, 1.19) when compared to perceiving no change in representation (Table S5 in Supplementary materials). In contrast, when compared to before COVID-19, perceiving more positive representation of people with obesity on social media during peak exposure of the outbreak was not associated with total distress (B 0.34; 95% CI: −0.02, 0.70) when compared to perceiving no change in representation (Table S5 in Supplementary materials). Tables S6–8 in the Supplementary Materials present the effect of the control variables on the models.
The moderating effect of loneliness on the association between the representation of people with obesity and mental wellbeing
There was limited evidence to suggest that loneliness moderated the impact of perceived experiences of weight-related stigma on mental wellbeing. For depression symptoms, the moderation model was a marginally better fit (Χ2 (4) = 10.92, p = 0.028), although it is notable the AIC difference was minor (<4; moderation model AIC = 10864, previous model AIC = 10867), with the R2 difference also being minimal (R2 change = 0.003). This is due to the significant (p = 0.024) moderating effect of loneliness on the association between the positive representation of people with obesity on social media and depression scores (Table 4). Simple slopes suggest that the association between more positive social media representation and higher depression symptoms was significant when loneliness was lower (−1SD, B 0.41, SE = 0.14; 95% CI: 0.13 to 0.70), but not at mean or +1 SD. For anxiety, there was no difference between the moderation model (AIC = 10952) and the previous model (AIC = 10948, Χ2 (4) = 4.06 p = 0.397), with the R2 difference being minimal (R2 change <0.001). Likewise, there was no difference between the wellbeing model (AIC = 25520) and the previous model (AIC = 25521, Χ2 (4) = 8.61, p = 0.072), with the R2 difference being minimal (R2 change = 0.002). Overall, we found limited evidence to suggest that loneliness moderated the relationship between representation of people with obesity of TV or social media and mental wellbeing, with the addition of loneliness as a moderator explaining less than ≤0.3% of the variance in outcomes in any of the three models.
Discussion
We investigated the relationship between the perceived representation of obesity on television and social media and mental wellbeing during the COVID-19 pandemic in a sample of people with obesity across 10 European countries. We found that perceiving more negative representation of people with obesity on social media during peak exposure of the pandemic was associated with higher levels of psychological distress and depression symptoms as well as lower levels of wellbeing. During the peak of the COVID-19 pandemic, compared to pre-pandemic, perceiving more positive representation of people with obesity on television was associated with greater symptoms of psychological distress and anxiety, and also higher levels of wellbeing. We also found marginal evidence to suggest that there was a stronger association between the positive representation of obesity on social media and greater depression symptoms when loneliness was lower; However, this association was small in size and not consistent across study findings. Due to the minimal effect and inconsistency across findings, we deemed it inappropriate to base implications or conclusions on this.
A recent systematic review of 105 studies conducted before the COVID-19 pandemic reported that experiencing weight-related stigma (i.e., negative representation of people with obesity) was associated with low mental wellbeing, including poor quality of life, depressive symptoms, and dissatisfaction with body image [7]. This finding aligns with the review of recent research by Ata and colleagues – in this review, the authors concluded that the stigmatising negative portrayals of obesity in wide ranging medias (e.g., television and social media) can be linked to psychological harm for both viewers and those with obesity [26]. Similarly, we found that perceiving more negative representation on social media during the COVID-19 pandemic compared to pre-pandemic was associated with reduced mental wellbeing. However, we also found that perceiving increased negative representation on television appeared to have no impact on mental wellbeing. This may be explained by the differences in how we experience television and social media [27, 49,50,51,52]. Clark and colleagues describe the weight stigma impacts of interacting with these medias as structural (i.e., beliefs encoded into society through consumed media), interpersonal (i.e., person-to-person interactions), and intrapersonal (i.e., internalised bias) [27]. Television is suggested to be associated with structured stigma as it is viewed but not interacted with, whereas social media contributes to structured, inter-, and intra-personal stigma as it is both viewed and interacted with via, for example, publicly posted comments [27]. The difference in how we interact with each type of media may contribute to explaining the differences by platform [26, 27]. For example, it is possible that viewing a television advert representing adults with obesity as “lazy” or “greedy” may have a lesser negative impact on mental wellbeing than viewing the same advert on social media alongside potentially stigmatising comments posted by the public. Furthermore, there are several regulations covering the content of television media (e.g., Ofcom Broadcasting Code) [53], whilst social media remains unregulated in comparison; this may further explain the differences by platform. Future research may wish to further investigate why the impact of stigma appears to differ by media platform to better understand the potential reasons for these findings.
Interestingly, we found that experiencing more positive representation of people with obesity on television during the pandemic, compared to before the pandemic, was associated with better psychological wellbeing, yet also higher psychological distress and anxiety. This may be due to the increased media reporting on (i) obesity as a risk factor for more severe COVID-19 complications and death and (ii) the introduction of a new obesity strategies and policies aiming to support those living with obesity (e.g., the new Obesity Strategy in the UK) [21, 23, 54]. Television reporting on the association between COVID-19 and obesity may have increased distress and anxiety; these reports may have reduced an individuals’ sense of perceived control over their weight and health, contributing to increased feelings of worry, anxiety, and concern. However, alongside this, reporting of the new strategies may have increased feelings of psychological wellbeing through feeling supported.
Addressing weight-related stigma requires action from multiple levels of influence and is likely to be a long-term process [13], and introducing relevant policies for media organisations would be a step forward in this process. We recommend and encourage greater media accountability when representing people with obesity, such as the introduction of legislation and regulations to avoid negative portrayals and stigmatising representation. Greater media accountability may also include highlighting the non-individual determinants of obesity (e.g., environmental, marketing) and using accurate, non-biased, respectful images which may be sourced, for example, from the EASO Obesity Image Bank or the World Obesity Image Bank [55, 56]. The use of non-biased and respectful images is noted to reduce weight-related stigma in the media [56].
We proposed that the relationship between perceiving more negative representation of obesity on television and social media and lower well-being may be particularly pronounced among participants with higher levels of loneliness. We found limited and inconsistent evidence suggesting that feelings of loneliness moderated the association between perceived representation on media and mental wellbeing. A recent systematic review, conducted before the COVID-19 pandemic, found that social support did not moderate the relationship between weight-related stigma and mental wellbeing, aligning with the findings of this study [7]. Social support and loneliness are strongly correlated, yet it is possible to have good social support and experience loneliness [7, 34]. Authors of the systematic review identified that there was a considerable lack of research assessing the moderating effects of social support on the relationship between weight-related stigma and mental wellbeing; similar can be noted for the evidence base assessing the moderating effect of loneliness. Future research should aim to investigate the influence of loneliness and social support separately on the impact of weight-related stigma to strengthen the evidence base, as well as investigating various other potential moderators (e.g., history of psychological treatment could protect mental wellbeing).
Strengths and limitations
This study is strengthened by the large sample of participants across 10 European countries, thus supporting the generalisability of the study findings. Whilst experiences of key study outcomes (perceived representation of obesity in media, mental wellbeing, and loneliness) differed across countries (see supplementary materials), the potential confounding effect of this was controlled for in statistical analyses, mitigating the risk of bias. Relevant control variables were included in statistical analyses to minimise the potential impact of confounders, reducing the likelihood of drawing inaccurate conclusions from the analyses. However, we were restricted by the variables available to control for. For example, we included highest educational attainment to control for the potential confounding effect of socioeconomic status (SES) and acknowledge that alternative measures (e.g., Index of Multiple Deprivation) may represent SES more accurately. Education status is one of the most commonly used measures of SES and is recognised as a suitable measure of SES [57].
We assessed changes in perceived representations of obesity in media (i.e., as an indicator of perceived stigmatising experiences) based on data collected at one-time point, often asking participants to compare their experiences during the peak of the pandemic to pre-pandemic. Consideration should be taken of this when interpreting findings due to the retrospective, cross-sectional and subjective nature of this measure. As the situation relating to the pandemic differed within and between countries, the phrasing of the “peak” of the pandemic allowed participants to self-define when the context of pandemic was most heightened; consideration of this should be taken when interpreting the findings. The measure used was study-specific due to the lack of a COVID-19 specific validated measure of changes in the perceived representation of obesity in media. Future research should consider using mixed methods longitudinal research designs to quantify the relationships between the key factors as well as exploring the thoughts, feelings, and meanings underpinning these findings.
Additionally, reverse causality may in part explain the observed findings as poorer mental wellbeing is associated with distorted interpretations [58,59,60,61]. For example, it is possible that those experiencing poor mental wellbeing during the pandemic may have perceived greater negative representations of obesity where there were none, or may be more likely to focus on any true negative representations they observed. Finally, it should be noted that the ethnicity of the participant population was 92% White or White mixed, therefore this should be considered when interpreting the data and determining generalisability of the findings to other situations or contexts.
Conclusion
During the peak of the COVID-19 pandemic, compared to pre-pandemic, perceiving more positive representation of people with obesity on television with associated with greater symptoms of total distress and anxiety, and greater wellbeing among adults living with obesity. Conversely, perceiving more negative representation of people with obesity on social media was associated with higher levels of total distress and depression, and lower levels of wellbeing. Feelings of loneliness did not appear to moderate the relationship between the perceived representation of obesity in media (i.e., perceived experiences of weight-related stigma) and mental wellbeing. We encourage greater media accountability when representing people with obesity to reduce the stigmatisation of this group.
Data availability
The dataset analysed during the current study is publicly available on the Open Science Framework (https://doi.org/10.17605/OSF.IO/VK3RC).
References
Bray GA, Kim KK, Wilding JPH. Obesity: a chronic relapsing progressive disease process. A position statement of the World Obesity Federation. Obes Rev. 2017;18:715–23.
American Medical Association. Report of the council on science and public health: Is obesity a disease? 2013;(Cdc):1–14. https://www.ama-assn.org/sites/default/files/media-browser/public/about-ama/councils/CouncilReports/council-on-science-public-health/a13csaph3.pdf.
James WPT. WHO recognition of the global obesity epidemic. Int J Obes. 2008;32:S120–6.
Canadian Obesity Network-Réseau canadien en obésité. Report Card on Access to Obesity Treatment for Adults in Canada 2017. Edmonton, AB: Canadian Obesity Network Inc.; 2017, April. https://obesitycanada.ca/wp-content/uploads/2017/07/Report-Card-Full-Version-PDF.pdf.
Frühbeck G, Busetto L, Dicker D, Yumuk V, Goossens GH, Hebebrand J, et al. The ABCD of obesity: An EASO position statement on a diagnostic term with clinical and scientific implications. Obes Facts. 2019;12:131–6.
Hruby A, Manson JAE, Qi L, Malik VS, Rimm EB, Sun Q, et al. Determinants and consequences of obesity. Am J Public Health. 2016;106:1656–62.
Emmer C, Bosnjak M, Mata J. The association between weight stigma and mental health: A meta‐analysis. Obes Rev. 2019;21:e12935. https://onlinelibrary.wiley.com/doi/abs/10.1111/obr.12935?af=R&utm_source=researcher_app&utm_medium=referral&utm_campaign=RESR_MRKT_Researcher_inbound.
Salas XR, Forhan M, Caulfield T, Sharma AM, Raine KD. Addressing internalized weight bias and changing damaged social identities for people living with obesity. Front Psychol. 2019;10:1–17.
World Health Organization. Weight bias and obesity stigma: considerations for the WHO European Region [Internet]. 2017 [cited 2018 Nov 22]. http://www.euro.who.int/__data/assets/pdf_file/0017/351026/WeightBias.pdf.
World Health Organization. The European Mental Health Action Plan 2013-2020 [Internet]. 2013. https://www.euro.who.int/__data/assets/pdf_file/0004/194107/63wd11e_MentalHealth-3.pdf.
Pudney EV, Himmelstein MS, Puhl RM, Foster GD. Distressed or not distressed? A mixed methods examination of reactions to weight stigma and implications for emotional wellbeing and internalized weight bias. Soc Sci Med [Internet]. 2020;14:112854. https://www.sciencedirect.com/science/article/pii/S0277953620300733?dgcid=rss_sd_all&utm_source=researcher_app&utm_medium=referral&utm_campaign=RESR_MRKT_Researcher_inbound.
Kane JC, Elafros MA, Murray SM, Mitchell EMH, Augustinavicius JL, Causevic S, et al. A scoping review of health-related stigma outcomes for high-burden diseases in low- and middle-income countries. BMC Med. 2019;17:17. https://doi.org/10.1186/s12916-019-1250-8.
Friedman RR, Puhl RM. Weight bias - A social justice issue: A policy brief. Yale Rudd Centre for Food Policy and Obesity. 2012.
Puhl R, CA H. Obesity stigma: important considerations for public health. Am J Public Health. 2010;100:1019–28.
Brown A, Flint S, Kalea AZ, O’Kane M, Williams S, Batterham R. Negative impact of COVID-19 lockdown upon health-related behaviours and psychological wellbeing in people living with severe and complex obesity in the UK. SSRN Electron J [Internet]. 2021;000. https://doi.org/10.1016/j.eclinm.2021.100796.
Rajkumar RP. COVID-19 and mental health: A review of the existing literature. Asian J Psychiatry J. 2020;52:102066. https://doi.org/10.1016/j.ajp.2020.102066.
Shigemura J, Ursano RJ, Morganstein JC, Kurosawa M, Benedek DM. Public responses to the novel 2019 coronavirus (2019-nCoV) in Japan: Mental health consequences and target populations. Psychiatry Clin Neurosci. 2020;74:281–2.
Choi KR, Heilemann MV, Fauer A, Mead M. A Second Pandemic: Mental Health Spillover From the Novel Coronavirus (COVID-19). J Am Psychiatr Nurses Assoc. 2020;26:340–3. https://doi.org/10.1177/1078390320919803.
Shah K, Kamrai D, Mekala H, Mann B, Desai K, Patel RS. Focus on mental health during the coronavirus (COVID-19) pandemic: applying learnings from the past outbreaks. Cureus. 2020;12:e7405. https://doi.org/10.7759/cureus.7405.
Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet [Internet]. 2020;395:912–20. https://doi.org/10.1016/S0140-6736(20)30460-8.
Le Brocq S, Clare K, Bryant M, Roberts K, Tahrani AA. Obesity and COVID-19: a call for action from people living with obesity. Lancet Diabetes Endocrinol. 2020;8:652–4.
Pearl RL. Weight Stigma and the “Quarantine-15.”. Obes (Silver Spring). 2020;28:1180–1.
Flint SW. Stigmatizing media portrayal of obesity during the coronavirus (COVID-19) pandemic. Front Psychol. 2020;11:2124. https://www.frontiersin.org/article/10.3389/fpsyg.2020.02124.
Hayward LE, Vartanian LR, Pinkus RT. Weight stigma predicts poorer psychological well-being through internalized weight bias and maladaptive coping responses. Obesity [Internet]. 2018;26:755–61. https://www.mendeley.com/catalogue/c3d993aa-abb0-38a3-a786-b47c91605056/.
Bidstrup H, Brennan L, Kaufmann L, de la Piedad Garcia X. Internalised weight stigma as a mediator of the relationship between experienced/perceived weight stigma and biopsychosocial outcomes: a systematic review. Int J Obes [Internet]. 2021:1–9. https://doi.org/10.1038/s41366-021-00982-4.
Ata RN, Thompson JK. Weight bias in the media: A review of recent research. Obes Facts. 2010;3:41–6.
Clark O, Lee MM, Jingree ML, O’Dwyer E, Yue Y, Marrero A, et al. Weight stigma and social media: evidence and public health solutions. Front Nutr. 2021;8. https://www.frontiersin.org/article/10.3389/fnut.2021.739056.
Obesity Empowerment Network. Weight stigma in the media. https://oen.org.uk/2021/09/29/weight-stigma-in-the-media/.
Selensky JC, Carels RA. Weight stigma and media: An examination of the effect of advertising campaigns on weight bias, internalized weight bias, self-esteem, body image, and affect. Body Image. 2021;36:95–106. https://doi.org/10.1016/j.bodyim.2020.10.008.
Hwang TJ, Rabheru K, Peisah C, Reichman W, Ikeda M. Loneliness and social isolation during the COVID-19 pandemic. Int Psychogeriatrics. 2020;32:1217–20.
Groarke JM, Berry E, Graham-Wisener L, McKenna-Plumley PE, McGlinchey E, Armour C. Loneliness in the UK during the COVID-19 pandemic: Cross-sectional results from the COVID-19 Psychological Wellbeing Study. PLoS One. 2020;15:1–18. https://doi.org/10.1371/journal.pone.0239698.
Banerjee D, Rai M. Social isolation in Covid-19: The impact of loneliness. Int J Soc Psychiatry. 2020;66:525–7.
Clair R, Gordon M, Kroon M, Reilly C. The effects of social isolation on well-being and life satisfaction during pandemic. Humanit Soc Sci Commun. 2021;8:1–6. https://doi.org/10.1057/s41599-021-00710-3.
Tiwari SC. Loneliness: A disease? Indian J Psychiatry. 2013;55:320–2. https://pubmed.ncbi.nlm.nih.gov/24459300.
De Jong Gierveld J. A 6-item scale for overall, emotional, and social loneliness: Confirmatory tests on survey data. Res Aging. 2006;28:582–98.
de Jong Gierveld J, van Tilburg T. The De Jong Gierveld short scales for emotional and social loneliness: Tested on data from 7 countries in the UN generations and gender surveys. Eur J Ageing. 2010;7:121–30.
Liu CH, Zhang E, Wong GTF, Hyun S, Hahm HC. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Res. 2020;290:113172. https://doi.org/10.1016/j.psychres.2020.113172.
Karami A, Khodarahimi S, Ghazanfari F, Mirdrikvand F, Barigh M. The prediction of distress tolerance based on the feeling of loneliness and self-handicapping in students. Pers Individ Dif. 2020;161:109994. https://doi.org/10.1016/j.paid.2020.109994.
Eres R, Lim MH, Lanham S, Jillard C, Bates G. Loneliness and emotion regulation: Implications of having social anxiety disorder. Aust J Psychol. 2021;73:46–56. https://doi.org/10.1080/00049530.2021.1904498.
NHS England. Who is at high risk from coronavirus (COVID-19). 2020. https://www.nhs.uk/conditions/coronavirus-covid-19/people-at-higher-risk/who-is-at-high-risk-from-coronavirus/.
Seow LSE, Chua BY, Xie H, Wang J, Ong HL, Abdin E, et al. Correct recognition and continuum belief of mental disorders in a nursing student population. BMC Psychiatry. 2017;17:1–8.
Angermeyer MC, Millier A, Rémuzat C, Refaï T, Schomerus G, Toumi M. Continuum beliefs and attitudes towards people with mental illness: Results from a national survey in France. Int J Soc Psychiatry. 2015;61:297–303.
Schomerus G, Angermeyer MC, Baumeister SE, Stolzenburg S, Link BG, Phelan JC. An online intervention using information on the mental health-mental illness continuum to reduce stigma. Eur Psychiatry. 2016;32:21–7. https://doi.org/10.1016/j.eurpsy.2015.11.006.
Kroenke K, Spitzer RL, Williams JBW, Löwe B. An ultra-brief screening scale for anxiety and depression: The PHQ–4. Psychosomatics. 2009;50:613–21.
Löwe B, Wahl I, Rose M, Spitzer C, Glaesmer H, Wingenfeld K, et al. A 4-item measure of depression and anxiety: Validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord. 2010;122:86–95. https://doi.org/10.1016/j.jad.2009.06.019.
Eisinga R, Grotenhuis M, Pelzer B. The reliability of a two-item scale: Pearson, Cronbach, or Spearman-Brown? Int J Public Health. 2013;58:637–42. https://doi.org/10.1007/s00038-012-0416-3.
Topp CW, Østergaard SD, Søndergaard S, Bech P. The WHO-5 well-being index: A systematic review of the literature. Psychother Psychosom. 2015;84:167–76.
Revelle W, Zinbarg RE. Coefficients Alpha, Beta, Omega, and the glb: Comments on Sijtsma. Psychometrika. 2008;74:145 https://doi.org/10.1007/s11336-008-9102-z.
Brownell KD, Puhl RM, Schwartz MB, Rudd L. Weight bias: Nature, consequences, and remedies. Weight bias: Nature, consequences, and remedies. New York, NY, US: Guilford Publications; 2005. xv, 320–xv, 320.
Pearl RL. Weight bias and stigma: public health implications and structural solutions. Soc Issues Policy Rev. 2018;12:146–82.
Greenberg BS, Eastin M, Hofschire L, Lachlan K, Brownell KD. Portrayals of overweight and obese individuals on commercial television. Am J Public Health. 2003;93:1342–8.
Himes SM, Thompson JK. Fat stigmatization in television shows and movies: A content analysis. Obesity. 2007;15:712–8.
Ofcom. The Ofcom Broadcasting Code (with the Cross-promotion Code and the On Demand Programme Service Rules). 2020. https://www.ofcom.org.uk/tv-radio-and-on-demand/broadcast-codes/broadcast-code.
Department of Health and Social Care. New specialised support to help those living with obesity to lose weight. 2021. https://www.gov.uk/government/news/new-specialised-support-to-help-those-living-with-obesity-to-lose-weight.
World Obesity. World Obesity Image Bank [Internet]. 2019 [cited 2022 Mar 9]. https://www.worldobesity.org/resources/image-bank.
European Association for the Study of Obesity. EASO Obesity Image Bank. [cited 2022 Mar 9]. https://easo.org/media-portal/obesity-image-bank/.
Oakes JM, Rossi PH. The measurement of SES in health research: Current practice and steps toward a new approach. Soc Sci Med. 2003;56:769–84.
Everaert J, Bronstein MV, Cannon TD, Joormann J. Looking through tinted glasses: depression and social anxiety are related to both interpretation biases and inflexible negative interpretations. Clin Psychol Sci. 2018;6:517–28. https://doi.org/10.1177/2167702617747968.
Everaert J, Podina IR, Koster EHW. A comprehensive meta-analysis of interpretation biases in depression. Clin Psychol Rev. 2017;58:33–48. https://doi.org/10.1016/j.cpr.2017.09.005.
Everaert J. Interpretation of ambiguity in depression. Curr Opin Psychol. 2021;41:9–14. https://doi.org/10.1016/j.copsyc.2021.01.003.
Krahé C, Whyte J, Bridge L, Loizou S, Hirsch CR. Are different forms of repetitive negative thinking associated with interpretation bias in generalized anxiety disorder and depression? Clin Psychol Sci. 2019;7:969–81. https://doi.org/10.1177/2167702619851808.
Acknowledgements
The authors would like to acknowledge their colleagues on the EUROPEANS study who contributed to ideation, design, and conduct of the EUROPEANS study: Dr Alison Fildes, Professor Emma Boyland, Dr Bethan Mead, Professor Jo Harrold, Vicki Mooney, Ken Clare. We would like to thank the participants of the EUROPEANS study for their participation in the study.
Funding
The EUROPEANS study was funded by the European Association for the Study of Obesity (EASO) and the European Coalition for People with obesity (EPCO). RAJ and ALA are supported by the Medical Research Council (MRC) (Grant MC_UU_00006/6). For the purpose of open access, the author has applied a Creative Commons Attribution (CC BY) licence to any Author Accepted Manuscript version arising.
Author information
Authors and Affiliations
Contributions
RAJ designed the study, interpreted the data, and drafted the manuscript. PC contributed to study design, analysed and interpreted the data, and provided critical appraisal of the manuscript. SHJ, ALA, and JH contributed to study design and provided critical appraisal of the manuscript. NGM contributed to the drafting of the manuscript and provided critical appraisal of the manuscript. JJD, RR, AB, SF, ER, and SB provided critical appraisal of the study and manuscript. CAH supervised the study, contributed to the study design, interpreted the data, and provided critical appraisal of the manuscript. All authors contributed to the design of the survey and read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
CAH, PC, NGM, and JCGH have received research funding from the American Beverage Association. CAH has received speaker fees from the International Sweeteners Association and the International Food Information Council for work outside of the present manuscript. ALA is the chief investigators on two publicly funded (MRC, NIHR) trials where the intervention is provided by WW (formerly Weight Watchers) at no cost. JCGH has received speaker fees from Novo Nordisk and consultancy from Dupont, International Sweeteners Association, Mars, Novo Nordisk for work outside of the present manuscript. AB has received funding for investigator-initiated research, travel grants, speaker fees and support to attend an obesity conference from Novo Nordisk for work outside this present manuscript. and is on the scientific advisory board and shareholder of Reset Health Clinics Ltd. SWF reports research grants from Johnson and Johnson, research grants from Novo Nordisk, and personal fees to support attendance at meetings from Johnson and Johnson and Novo Nordisk, outside of the submitted work. RJ, SHJ, SB, RR, and JD declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jones, R.A., Christiansen, P., Maloney, N.G. et al. Perceived weight-related stigma, loneliness, and mental wellbeing during COVID-19 in people with obesity: A cross-sectional study from ten European countries. Int J Obes 46, 2120–2127 (2022). https://doi.org/10.1038/s41366-022-01220-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-022-01220-1
This article is cited by
-
Prevalence of loneliness and associations with health behaviours and body mass index in 5835 people living with and beyond cancer: a cross-sectional study
BMC Public Health (2024)
-
Association between weight, weight perception, weight teasing and mental health among adolescents
Child and Adolescent Psychiatry and Mental Health (2024)
-
Obesity and the cost of living crisis
International Journal of Obesity (2023)