Abstract
Objectives
We aimed to investigate the relationship of weight change across adulthood with the risk of hearing loss.
Methods
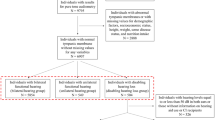
The data from National Health and Nutrition Examination Surveys. Cox proportional hazards models were applied to explore the association between weight change and risk of hearing loss. Kaplan-Meier method was used to plot the survival curves associated with weight change patterns.
Results
Compared with participants who remained at normal weight, those with stable obese participants had increased risks of total hearing loss across adulthood, with hazard ratios of 1.24 (95% confidence intervals 1.11–1.38) from age 25 years to baseline, 1.09 (1.001–1.18) from 10 years before baseline to baseline, and 1.23 (1.10–1.37) from age 25 years to 10 years before baseline. Moving the obese to non-obese weight change pattern from middle to late adulthood was not significantly associated with an increased risk of total hearing loss (1.04, 0.91–1.19) and high-frequency hearing loss (1.02, 0.90–1.17), whereas changing from non-obese to obese body mass index over this period was associated with total hearing loss risk (1.20, 1.11–1.29), and speech- and high-frequency hearing loss (1.21, 1.07–1.36; 1.18, 1.09–1.28). Those moving from the non-obese to obese category between young and middle adulthood had a 16% (1.16, 1.02–1.33) higher risk of speech-frequency hearing loss.
Conclusions
Stable obesity and weight gain across adulthood are both associated with increased risks of hearing loss. Our findings imply that maintaining normal weight across adulthood is of great importance for preventing hearing loss in later life.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
Data are available at https://wwwn.cdc.gov/nchs/nhanes.
References
Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet (London, England) 2017; 390: 2627–42.
Beuther DA, Sutherland ER. Overweight, obesity, and incident asthma: A meta-analysis of prospective epidemiologic studies. American J Resp Critical Care Med. 2007;175:661–6.
Hu Y, Zong G, Liu G, Wang M, Rosner B, Pan A, et al. Smoking Cessation, Weight Change, Type 2 Diabetes, and Mortality. New England J Med. 2018;379:623–32.
Anyanwagu U, Mamza J, Donnelly R, Idris I. Association between insulin-induced weight change and CVD mortality: Evidence from a historic cohort study of 18,814 patients in UK primary care. Diab/Metabol Res Rev. 2018;34:e2945.
Fontana L, Hu FB. Optimal body weight for health and longevity: bridging basic, clinical, and population research. Aging Cell. 2014;13:391–400.
Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K, Lee A, et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. New England J Med. 2017;377:13–27.
Hwang JH, Wu CC, Hsu CJ, Liu TC, Yang WS. Association of central obesity with the severity and audiometric configurations of age-related hearing impairment. Obesity (Silver Spring, Md.). 2009;17:1796–801.
Üçler R, Turan M, Garça F, Acar İ, Atmaca M, Çankaya H. The association of obesity with hearing thresholds in women aged 18–40 years. Endocrine. 2016;52:46–53.
Fransen E, Topsakal V, Hendrickx JJ, Van Laer L, Huyghe JR, Van Eyken E, et al. Occupational noise, smoking, and a high body mass index are risk factors for age-related hearing impairment and moderate alcohol consumption is protective: a European population-based multicenter study. J Assoc Res Otolaryngol: JARO. 2008;9:264–76.
Hu H, Tomita K, Kuwahara K, Yamamoto M, Uehara A, Kochi T, et al. Obesity and risk of hearing loss: A prospective cohort study. Clin Nutr. (Edinburgh, Scotland). 2020;39:870–5.
Cruickshanks KJ, Nondahl DM, Dalton DS, Fischer ME, Klein BE, Klein R, et al. Smoking, central adiposity, and poor glycemic control increase risk of hearing impairment. J American Geriatrics Soc. 2015;63:918–24.
Curhan SG, Eavey R, Wang M, Stampfer MJ, Curhan GC. Body mass index, waist circumference, physical activity, and risk of hearing loss in women. American J Med. 2013;126:1142.e1–8.
Shargorodsky J, Curhan SG, Eavey R, Curhan GC. A prospective study of cardiovascular risk factors and incident hearing loss in men. Laryngoscope. 2010;120:1887–91.
Choi YH, Hu H, Mukherjee B, Miller J, Park SK. Environmental cadmium and lead exposures and hearing loss in U.S. adults: the National Health and Nutrition Examination Survey, 1999 to 2004. Environ Health Perspectives. 2012;120:1544–50.
Agrawal Y, Platz EA, Niparko JK. Prevalence of hearing loss and differences by demographic characteristics among US adults: data from the National Health and Nutrition Examination Survey, 1999-2004. Arch Int Med. 2008;168:1522–30.
Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. WMJ: official publication of the State Medical Society of Wisconsin 1998; 97: 20-1, 24-5, 27-37.
Chen C, Ye Y, Zhang Y, Pan XF, Pan A. Weight change across adulthood in relation to all cause and cause specific mortality: Prospective cohort study. BMJ (Clinical research ed.). 2019;367:15584.
Stokes A, Collins JM, Grant BF, Scamuffa RF, Hsiao CW, Johnston SS, et al. Obesity Progression Between Young Adulthood and Midlife and Incident Diabetes: A Retrospective Cohort Study of U.S. Adults. Diabetes Care. 2018;41:1025–31.
Rao JNK, Scott AJ. On Chi-Squared Tests for Multiway Contingency Tables with Cell Proportions Estimated from Survey Data. J Ann Stat. 1984;15:46–60.
Dietz WH. Obesity and Excessive Weight Gain in Young Adults: New Targets for Prevention. Jama. 2017;318:241–2.
Poirrier AL, Pincemail J, Van Den Ackerveken P, Lefebvre PP, Malgrange B. Oxidative stress in the cochlea: an update. Curr Medicinal Chem. 2010;17:3591–604.
Hwang JH, Hsu CJ, Yu WH, Liu TC, Yang WS. Diet-induced obesity exacerbates auditory degeneration via hypoxia, inflammation, and apoptosis signaling pathways in CD/1 mice. PloS One. 2013;8:e60730.
Makishima K. Arteriolar sclerosis as a cause of presbycusis. Otolaryngology. 1978;86:Orl322–6.
Shi X. Physiopathology of the cochlear microcirculation. Hearing Res. 2011;282:10–24.
De Rubeis V, Bayat S, Griffith LE, Smith BT, Anderson LN. Validity of self-reported recall of anthropometric measures in early life: A systematic review and meta-analysis. Obes Rev. 2019;20:1426–40.
Golubic R, Ekelund U, Wijndaele K, Luben R, Khaw KT, Wareham NJ, et al. Rate of weight gain predicts change in physical activity levels: A longitudinal analysis of the EPIC-Norfolk cohort. Int J Obes. 2013;37:404–9.
Ritchie LD, Spector P, Stevens MJ, Schmidt MM, Schreiber GB, Striegel-Moore RH, et al. Dietary patterns in adolescence are related to adiposity in young adulthood in black and white females. J Nutr. 2007;137:399–406.
Funding
The study was supported by the Hubei Province Key Laboratory of Occupational Hazard Identification and Control, Wuhan University of Science and Technology (OHIC2021Y03) and the Fundamental Research Funds for the Central Universities (2019kfyXJJS032). The funder did not play any role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; nor in the preparation, review, or approval of the manuscript.
Author information
Authors and Affiliations
Contributions
WZL wrote the manuscript and performed statistical analysis. WZL conceived and designed the study, and interpreted data. DJC, YP, ZXL and YQT critically revised the manuscript and approved the final version. WZL is the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, W., Peng, Y., Chen, D. et al. Association of weight change across adulthood with hearing loss: A retrospective cohort study. Int J Obes 46, 1825–1832 (2022). https://doi.org/10.1038/s41366-022-01197-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-022-01197-x