Abstract
Background/Objectives
Sleep measures, such as duration and onset timing, are associated with adiposity outcomes among children. Recent research among adults has considered variability in sleep and wake onset times, with the Sleep Regularity Index (SRI) as a comprehensive metric to measure shifts in sleep and wake onset times between days. However, little research has examined regularity and adiposity outcomes among children. This study examined the associations of three sleep measures (i.e., sleep duration, sleep onset time, and SRI) with three measures of adiposity (i.e., body mass index [BMI], waist circumference, and waist-to-height ratio [WHtR]) in a pediatric sample.
Subjects/Methods
Children (ages 4–13 years) who were part of the U.S. Newborn Epigenetic STudy (NEST) participated. Children (N = 144) wore an ActiGraph for 1 week. Sleep measures were estimated from actigraphy data. Weight, height, and waist circumference were measured by trained researchers. BMI and WHtR was calculated with the objectively measured waist and height values. Multiple linear regression models examined associations between child sleep and adiposity outcomes, controlling for race/ethnicity, child sex, age, mothers’ BMI and sleep duration.
Results
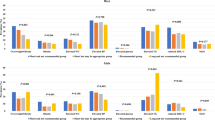
When considering sleep onset timing and duration, along with demographic covariates, sleep onset timing was not significantly associated with any of the three adiposity measures, but a longer duration was significantly associated with a lower BMI Z-score (β = −0.29, p < 0.001), waist circumference (β = −0.31, p < 0.001), and WHtR (β = −0.38, p < 0.001). When considering SRI and duration, duration remained significantly associated with the adiposity measures. The SRI and adiposity associations were in the expected direction, but were non-significant, except the SRI and WHtR association (β = −0.16, p = 0.077) was marginally non-significant.
Conclusions
Sleep duration was consistently associated with adiposity measures in children 4–13 years of age. Pediatric sleep interventions should focus first on elongating nighttime sleep duration, and examine if this improves child adiposity outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Morrissey B, Taveras E, Allender S, Strugnell C. Sleep and obesity among children: a systematic review of multiple sleep dimensions. Pediatr Obes. 2020;15:e12619.
Miller MA, Bates S, Ji C, Cappuccio FP. Systematic review and meta-analyses of the relationship between short sleep and incidence of obesity and effectiveness of sleep interventions on weight gain in preschool children. Obes Rev. 2021;22:e13113.
Ash T, Taveras EM. Associations of short sleep duration with childhood obesity and weight gain: summary of a presentation to the National Academy of Science’s Roundtable on Obesity Solutions. Sleep Health. 2017;3:389–92.
Fatima Y, Doi SaR, Mamun AA. Longitudinal impact of sleep on overweight and obesity in children and adolescents: a systematic review and bias-adjusted meta-analysis. Obes Rev. 2015;16:137–49.
Ruan H, Xun P, Cai W, He K, Tang Q. Habitual sleep duration and risk of childhood obesity: systematic review and dose-response meta-analysis of prospective cohort studies. Sci Rep. 2015;5:16160.
Golley RK, Maher CA, Matricciani L, Olds TS. Sleep duration or bedtime? Exploring the association between sleep timing behaviour, diet and BMI in children and adolescents. Int J Obes. 2013;37:546–51.
Jarrin DC, McGrath JJ, Drake CL. Beyond sleep duration: distinct sleep dimensions are associated with obesity in children and adolescents. Int J Obes. 2013;37:552–8.
Miller AL, Lumeng JC, LeBourgeois MK. Sleep patterns and obesity in childhood. Curr Opin Endocrinol Diabetes Obes. 2015;22:41–7.
Scharf RJ, DeBoer MD. Sleep timing and longitudinal weight gain in 4- and 5-year-old children. Pediatr Obes. 2015;10:141–8.
Spruyt K, Molfese DL, Gozal D. Sleep duration, sleep regularity, body weight, and metabolic homeostasis in school-aged children. Pediatrics. 2011;127:e345–52.
Chung K-F, Kan K-K, Yeung W-F. Sleep duration, sleep–wake schedule regularity, and body weight in Hong Kong Chinese adolescents. Biol Rhythm Res. 2012;44:169–79.
Fischer D, Klerman EB, Phillips AJK. Measuring sleep regularity: theoretical properties and practical usage of existing metrics. Sleep. 2021:zsab103. https://doi.org/10.1093/sleep/zsab103.
Wittmann M, Dinich J, Merrow M, Roenneberg T. Social jetlag: misalignment of biological and social time. Chronobiol Int. 2006;23:497–509.
Fischer D, Vetter C, Roenneberg T. A novel method to visualise and quantify circadian misalignment. Sci Rep. 2016;6:38601.
Phillips AJK, Clerx WM, O’Brien CS, Sano A, Barger LK, Picard RW, et al. Irregular sleep/wake patterns are associated with poorer academic performance and delayed circadian and sleep/wake timing. Sci Rep. 2017;7:3216.
Lunsford-Avery JR, Engelhard MM, Navar AM, Kollins SH. Validation of the Sleep Regularity Index in older adults and associations with cardiometabolic risk. Sci Rep. 2018;8:14158.
Bustamante CMV, Rodman AM, Dennison MJ, Flournoy JC, Mair P, McLaughlin KA. Within-person fluctuations in stressful life events, sleep, and anxiety and depression symptoms during adolescence: a multiwave prospective study. J Child Psychol Psychiatry. 2020;61:1116–25.
Lunsford-Avery JR, Damme KSF, Engelhard MM, Kollins SH, Mittal VA. Sleep/wake regularity associated with default mode network structure among healthy adolescents and young adults. Sci Rep. 2020;10:509.
Westenhoefer J. Establishing dietary habits during childhood for long-term weight control. Ann Nutr Metab. 2002;46:18–23.
Dahl RE, Lewin DS. Pathways to adolescent health sleep regulation and behavior. J Adolesc Health. 2002;31:175–84.
Dennison BA, Russo TJ, Burdick PA, Jenkins PL. An intervention to reduce television viewing by preschool children. Arch Pediatr Adolesc Med. 2004;158:170.
Janssen I. Combined influence of body mass index and waist circumference on coronary artery disease risk factors among children and adolescents. Pediatrics. 2005;115:1623–30.
Khoury M, Manlhiot C, McCrindle BW. Role of the waist/height ratio in the cardiometabolic risk assessment of children classified by body mass index. J Am Coll Cardiol. 2013;62:742–51.
Lo K, Wong M, Khalechelvam P, Tam W. Waist-to-height ratio, body mass index and waist circumference for screening paediatric cardio-metabolic risk factors: a meta-analysis. Obes Rev. 2016;17:1258–75.
Brambilla P, Bedogni G, Heo M, Pietrobelli A. Waist circumference-to-height ratio predicts adiposity better than body mass index in children and adolescents. Int J Obes. 2013;37:943–6.
Liu Y, Murphy SK, Murtha AP, Fuemmeler BF, Schildkraut J, Huang Z, et al. Depression in pregnancy, infant birth weight and DNA methylation of imprint regulatory elements. Epigenetics. 2012;7:735–46.
Hoyo C, Murtha AP, Schildkraut JM, Forman MR, Calingaert B, Demark-Wahnefried W, et al. Folic acid supplementation before and during pregnancy in the Newborn Epigenetics STudy (NEST). BMC Public Health. 2011;11:1–8.
Barry CM, Sabhlok A, Saba VC, Majors AD, Schechter JC, Levine EL, et al. An automated text-messaging platform for enhanced retention and data collection in a longitudinal birth cohort: cohort management platform analysis. JMIR Public Health Surveill. 2019;5:e11666.
Chen S, Perera R, Engelhard M, Lunsford-Avery J, Kollins S, Fuemmeler B. A generic algorithm for sleep-wake cycle detection using unlabeled actigraphy data. In: 2019 IEEE EMBS International Conference on Biomedical & Health Informativs (BHI). 2019. p. 1–4.
Marler MR, Gehrman P, Martin JL, Ancoli-Israel S. The sigmoidally transformed cosine curve: a mathematical model for circadian rhythms with symmetric non-sinusoidal shapes. Stat Med. 2006;25:3893–904.
Centers for Disease Control and Prevention. Centers for Disease Control and Prevention. Anthropometry procedures manual. 2021. http://www.cdc.gov/nchs/data/nhanes/bm.pdf.
Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Ser B Methodol. 1995;57:289–300.
Eisenmann JC, Ekkekakis P, Holmes M. Sleep duration and overweight among Australian children and adolescents. Acta Paediatr. 2006;95:956–63.
Carson V, Tremblay MS, Chaput JP, Chastin SFM. Associations between sleep duration, sedentary time, physical activity, and health indicators among Canadian children and youth using compositional analyses. Appl Physiol Nutr Metab. 2016;41:S294–302.
Gong QH, Li SX, Li H, Cui J, Xu GZ. Insufficient sleep duration and overweight/obesity among adolescents in a Chinese population. Int J Environ Res Public Health. 2018;15:997.
Nam GE, Han K, Kim DH, Lee JH, Seo WH. Sleep duration is associated with body fat and muscle mass and waist-to-height ratio beyond conventional obesity parameters in Korean adolescent boys. J Sleep Res. 2017;26:444–52.
Dashti HS, Scheer FA, Jacques PF, Lamon-Fava S, Ordovás JM. Short sleep duration and dietary intake: epidemiologic evidence, mechanisms, and health implications. Adv Nutr. 2015;6:648–59.
Pattinson CL, Smith SS, Staton SL, Trost SG, Thorpe KJ. Investigating the association between sleep parameters and the weight status of children: night sleep duration matters. Sleep Health. 2018;4:147–53.
Lo K, Keung V, Cheung C, Tam W, Lee A. Associations between sleep pattern and quality and cardiovascular risk factors among Macao school students. Child Obes. 2019;15:387–96.
Roane B, Seifer R, Sharkey K, Van Reen E, Bond T, Raffray T, et al. What role does sleep play in weight gain in the first semester of university? Behav Sleep Med. 2015;13:491–505.
Bei B, Seeman TE, Carroll JE, Wiley JF. Sleep and physiological dysregulation: a closer look at sleep intraindividual variability. Sleep. 2017;40. https://doi.org/10.1093/sleep/zsx109.
Dong L, Martinez AJ, Buysse DJ, Harvey AG. A composite measure of sleep health predicts concurrent mental and physical health outcomes in adolescents prone to eveningness. Sleep Health. 2019;5:166–74.
Zhou M, Lalani C, Banda JA, Robinson TN. Sleep duration, timing, variability and measures of adiposity among 8‐ to 12‐year‐old children with obesity. Obes Sci Pract. 2018;4:535–44.
Guidolin M, Gradisar M. Is shortened sleep duration a risk factor for overweight and obesity during adolescence? A review of the empirical literature. Sleep Med. 2012;13:779–86.
Quist JS, Sjödin A, Chaput JP, Hjorth MF. Sleep and cardiometabolic risk in children and adolescents. Sleep Med Rev. 2016;29:76–100.
Poston WSC, Jitnarin N, Haddock CK, Jahnke SA, Day RS. Accuracy of self-reported weight, height and BMI in US firefighters. Occup Med. 2014;64:246–54.
Girschik J, Fritschi L, Heyworth J, Waters F. Validation of self-reported sleep against actigraphy. J Epidemiol. 2012;22:462–8.
Zabinski MF, Saelens BE, Stein RI, Hayden-Wade HA, Wilfley DE. Overweight children’s barriers to and support for physical activity. Obes Res. 2003;11:238–46.
Goldfield GS, Moore C, Henderson K, Buchholz A, Obeid N, Flament MF. Body dissatisfaction, dietary restraint, depression, and weight status in adolescents. J Sch Health. 2010;80:186–92.
Stein MB, Belik SL, Jacobi F, Sareen J. Impairment associated with sleep problems in the community: relationship to physical and mental health comorbidity. Psychosom Med. 2008;70:913–9.
Buysse DJ. Sleep health: can we define it? Does It matter? Sleep. 2014;37:9–17.
Meltzer LJ, Williamson AA, Mindell JA. Pediatric sleep health: it matters, and so does how we define it. Sleep Med Rev. 2021;57:101425.
Arora T, Gad H, Omar OM, Choudhury S, Chagoury O, Sheikh J, et al. The associations among objectively estimated sleep and obesity indicators in elementary schoolchildren. Sleep Med. 2018;47:25–31.
Wing YK, Li SX, Li AM, Zhang J, Kong APS. The effect of weekend and holiday sleep compensation on childhood overweight and obesity. Pediatrics. 2009;124:e994–1000.
Acknowledgements
This research was supported by the National Institute of Environmental Health Sciences (R01ES016772, P30ES011961 pilot project, R21ES014947, P01ES022831, and R24ES028531), the US Environmental Protection Agency (RD-83543701), the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R01HD084487), the National Institute of Diabetes and Digestive and Kidney Diseases (R01DK085173), and the Duke Cancer Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders. Further, USEPA does not endorse the purchase of any commercial products or services mentioned in the publication. In addition, this research was supported in part by the Intramural Research Program of the NIH, National Institute of Environmental Health Sciences. This work was also supported, in part, by the National Cancer Institute (T32CA093423) for ELA postdoctoral effort and by the National Institute of General Medical Sciences (2K12GM093857-10) for TEG postdoctoral effort.
Author information
Authors and Affiliations
Contributions
TEG, ELA, AK, DJB, JLA, SC, SK, JCS and BFF contributed to the conceptualization of the study. JCS, RM and BFF supervised data collection. TEG, SC, AK and ME analyzed the data. All authors contributed to writing and editing of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Glasgow, T.E., Adams, E.L., Ksinan, A. et al. Sleep onset, duration, or regularity: which matters most for child adiposity outcomes?. Int J Obes 46, 1502–1509 (2022). https://doi.org/10.1038/s41366-022-01140-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-022-01140-0