Abstract
Introduction
Roux-en-Y gastric bypass (RYGB) surgery markedly increases the rate of intestinal nutrient exposure after food intake, accelerates intestinal absorption of dietary glucose and protein, and alters the postprandial gut hormone response. However, our understanding of postprandial fat absorption and metabolism after RYGB is incomplete.
Methods
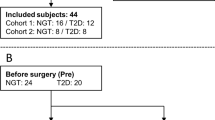
Stable palmitate tracers were administered intravenously (K-[2,2-2H2]palmitate) and orally with a mixed meal ([U-13C16]palmitate) to study fatty acid absorption and metabolism before and 3 months after RYGB in 10 participants with obesity and normal glucose tolerance.
Results
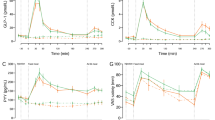
There was a tendency toward reduced fasting plasma nonesterified palmitate concentrations after RYGB, but neither fasting palmitate kinetics nor fasting triacylglycerol (TAG) concentrations changed compared with before surgery. Postprandial TAG concentrations were numerically, but nonsignificantly, reduced 3−4 h after meal intake after compared with before RYGB. However, the postprandial appearance of the oral palmitate tracer in the plasma TAG pool and overflow into the nonesterified palmitate pool were initially faster but overall reduced after RYGB by 50% (median, IQR: [47;64], P = 0.004) and 46% (median, IQR: [33;70], P = 0.041), respectively. The maximal postprandial suppression of plasma nonesterified palmitate concentrations was slightly greater but shorter lasting after RYGB ('time × visit' interaction: P < 0.001), without detectable effects of surgery on the rate of appearance and disappearance of plasma palmitate.
Conclusion
RYGB resulted in an initially accelerated but overall ~50% reduced 4-h postprandial systemic appearance of dietary palmitate in participants with obesity and normal glucose tolerance. This is likely a result of faster but incomplete intestinal fat absorption combined with enhanced chylomicron–TAG clearance, but it needs further investigation in studies specifically designed to investigate these mechanisms.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
Reasonable requests for access to the datasets should be addressed to the corresponding author.
References
Sjöström L, Peltonen M, Jacobson P, Sjöström CD, Karason K, Wedel H, et al. Bariatric surgery and long-term cardiovascular events. JAMA. 2012;307:56–65. https://doi.org/10.1001/jama.2011.1914.
Sjöström L. Review of the key results from the Swedish Obese Subjects (SOS) trial - a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013;273:219–34. https://doi.org/10.1111/joim.12012.
Li J, Lai D, Wu D. Laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy to treat morbid obesity-related comorbidities: a systematic review and meta-analysis. Obes Surg. 2016;26:429–42. https://doi.org/10.1007/s11695-015-1996-9.
Holst JJ, Madsbad S, Bojsen-Møller KN, Svane MS, Jørgensen NB, Dirksen C, et al. Mechanisms in bariatric surgery: gut hormones, diabetes resolution, and weight loss. Surg Obes Relat Dis. 2018;14:708–14. https://doi.org/10.1016/j.soard.2018.03.003.
Heffron SP, Parikh A, Volodarskiy A, Ren-Fielding C, Schwartzbard A, Nicholson J, et al. Changes in lipid profile of obese patients following contemporary bariatric surgery: a meta-analysis. Am J Med. 2016;129:952–9. https://doi.org/10.1016/j.amjmed.2016.02.004.
Bays H, Kothari SN, Azagury DE, Morton JM, Nguyen NT, Jones PH, et al. Lipids and bariatric procedures part 2 of 2: scientific statement from the American Society for Metabolic and Bariatric Surgery (ASMBS), the National Lipid Association (NLA), and Obesity Medicine Association (OMA). Surg Obes Relat Dis. 2016;12:468–95. https://doi.org/10.1016/j.soard.2016.01.007.
Kwok CS, Pradhan A, Khan MA, Anderson SG, Keavney BD, Myint PK, et al. Bariatric surgery and its impact on cardiovascular disease and mortality: a systematic review and meta-analysis. Int J Cardiol. 2014;173:20–8. https://doi.org/10.1016/j.ijcard.2014.02.026.
Douros JD, Tong J, D’Alessio DA. The effects of bariatric surgery on islet function, insulin secretion, and glucose control. Endocr Rev. 2019;40:1394–423. https://doi.org/10.1210/er.2018-00183.
Dirksen C, Jørgensen NB, Bojsen-Møller KN, Kielgast U, Jacobsen SH, Clausen TR, et al. Gut hormones, early dumping and resting energy expenditure in patients with good and poor weight loss response after Roux-en-Y gastric bypass. Int J Obes. 2013;37:1452–9. https://doi.org/10.1038/ijo.2013.15.
Dirksen C, Graff J, Fuglsang S, Rehfeld JF, Holst JJ, Madsen JL. Energy intake, gastrointestinal transit, and gut hormone release in response to oral triglycerides and fatty acids in men with and without severe obesity. Am J Physiol Gastrointest Liver Physiol. 2019;316:G332–7. https://doi.org/10.1152/ajpgi.00310.2018.
Eiken A, Fuglsang S, Eiken M, Svane MS, Kuhre RE, Wewer Albrechtsen NJ, et al. Bilio-enteric flow and plasma concentrations of bile acids after gastric bypass and sleeve gastrectomy. Int J Obes. 2020; https://doi.org/10.1038/s41366-020-0578-7.
Bojsen-Møller KN, Jacobsen SH, Dirksen C, Jørgensen NB, Reitelseder S, Jensen J-EB, et al. Accelerated protein digestion and amino acid absorption after Roux-en-Y gastric bypass. Am J Clin Nutr. 2015;102:600–7. https://doi.org/10.3945/ajcn.115.109298.
Jacobsen SH, Bojsen-Møller KN, Dirksen C, Jørgensen NB, Clausen TR, Wulff BS, et al. Effects of gastric bypass surgery on glucose absorption and metabolism during a mixed meal in glucose-tolerant individuals. Diabetologia. 2013;56:2250–4. https://doi.org/10.1007/s00125-013-3003-0.
Svane MS, Bojsen-Møller KN, Martinussen C, Dirksen C, Madsen JL, Reitelseder S, et al. Postprandial nutrient handling and gastrointestinal secretion of hormones after Roux-en-Y gastric bypass vs sleeve gastrectomy. Gastroenterology. 2019;156:1627–41. https://doi.org/10.1053/j.gastro.2019.01.262.
Jensen CZ, Bojsen-Møller KN, Svane MS, Holst LM, Hermansen K, Hartmann B, et al. Responses of gut and pancreatic hormones, bile acids, and fibroblast growth factor-21 differ to glucose, protein, and fat ingestion after gastric bypass surgery. Am J Physiol Gastrointest Liver Physiol. 2020;318:G661–72. https://doi.org/10.1152/ajpgi.00265.2019.
Griffo E, Cotugno M, Nosso G, Saldalamacchia G, Mangione A, Angrisani L, et al. Effects of sleeve gastrectomy and gastric bypass on postprandial lipid profile in obese type 2 diabetic patients: a 2-year follow-up. Obes Surg. 2016;26:1247–53. https://doi.org/10.1007/s11695-015-1891-4.
Griffo E, Nosso G, Lupoli R, Cotugno M, Saldalamacchia G, Vitolo G, et al. Early improvement of postprandial lipemia after bariatric surgery in obese type 2 diabetic patients. Obes Surg. 2014;24:765–70. https://doi.org/10.1007/s11695-013-1148-z.
Liaskos C, Koliaki C, Alexiadou K, Argyrakopoulou G, Tentolouris N, Diamantis T, et al. Roux-en-Y gastric bypass is more effective than sleeve gastrectomy in improving postprandial glycaemia and lipaemia in non-diabetic morbidly obese patients: a short-term follow-up analysis. Obes Surg. 2018;28:3997–4005. https://doi.org/10.1007/s11695-018-3454-y.
De Giorgi S, Campos V, Egli L, Toepel U, Carrel G, Cariou B, et al. Long-term effects of Roux-en-Y gastric bypass on postprandial plasma lipid and bile acids kinetics in female non diabetic subjects: a cross-sectional pilot study. Clin Nutr. 2015;34:911–7. https://doi.org/10.1016/j.clnu.2014.09.018.
Carswell KA, Belgaumkar AP, Amiel SA, Patel AG. A systematic review and meta-analysis of the effect of gastric bypass surgery on plasma lipid levels. Obes Surg. 2016;26:843–55. https://doi.org/10.1007/s11695-015-1829-x.
Jegatheesan P, Seyssel K, Stefanoni N, Rey V, Schneiter P, Giusti V, et al. Effects of gastric bypass surgery on postprandial gut and systemic lipid handling. Clin Nutr ESPEN. 2020;35:95–102. https://doi.org/10.1016/j.clnesp.2019.11.002.
Moreland AM, Santa Ana CA, Asplin JR, Kuhn JA, Holmes RP, Cole JA, et al. Steatorrhea and hyperoxaluria in severely obese patients before and after Roux-en-Y gastric bypass. Gastroenterology. 2017;152:1055–67e3. https://doi.org/10.1053/j.gastro.2017.01.004.
Odstrcil EA, Martinez JG, Santa Ana CA, Xue B, Schneider RE, Steffer KJ, et al. The contribution of malabsorption to the reduction in net energy absorption after long-limb Roux-en-Y gastric bypass. Am J Clin Nutr. 2010;92:704–13. https://doi.org/10.3945/ajcn.2010.29870.
Van Hall G, Bülow J, Sacchetti M, Al Mulla N, Lyngso D, Simonsen L. Regional fat metabolism in human splanchnic and adipose tissues; the effect of exercise. J Physiol. 2002;543:1033–46. https://doi.org/10.1113/jphysiol.2002.022392.
Sacchetti M, Saltin B, Olsen DB, van Hall G. High triacylglycerol turnover rate in human skeletal muscle. J Physiol. 2004;561:883–91. https://doi.org/10.1113/jphysiol.2004.075135.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9. https://doi.org/10.1007/bf00280883.
Carreau A-M, Noll C, Blondin DP, Frisch F, Nadeau M, Pelletier M, et al. Bariatric surgery rapidly decreases cardiac dietary fatty acid partitioning and hepatic insulin resistance through increased intra-abdominal adipose tissue storage and reduced spillover in type 2 diabetes. Diabetes. 2020;69:567–77. https://doi.org/10.2337/db19-0773.
Heath RB, Karpe F, Milne RW, Burdge GC, Wootton SA, Frayn KN. Selective partitioning of dietary fatty acids into the VLDL TG pool in the early postprandial period. J Lipid Res. 2003;44:2065–72. https://doi.org/10.1194/jlr.M300167-JLR200.
Heath RB, Karpe F, Milne RW, Burdge GC, Wootton SA, Frayn KN. Dietary fatty acids make a rapid and substantial contribution to VLDL-triacylglycerol in the fed state. Am J Physiol Endocrinol Metab. 2007;292:E732–739. https://doi.org/10.1152/ajpendo.00409.2006.
Yoshimura N, Kinoshita M, Teramoto T. Isolation and characterization of apolipoprotein B48-containing lipoproteins with a monoclonal antibody against apolipoprotein B48. J Atheroscler Thromb. 2009;16:740–7. https://doi.org/10.5551/jat.no976.
Magkos F, Fabbrini E, McCrea J, Patterson BW, Eagon JC, Klein S. Decrease in hepatic very-low-density lipoprotein-triglyceride secretion after weight loss is inversely associated with changes in circulating leptin. Diabetes Obes Metab. 2010;12:584–90. https://doi.org/10.1111/j.1463-1326.2009.01191.x.
Padilla N, Maraninchi M, Béliard S, Berthet B, Nogueira J-P, Wolff E, et al. Effects of bariatric surgery on hepatic and intestinal lipoprotein particle metabolism in obese, nondiabetic humans. Arterioscler Thromb Vasc Biol. 2014;34:2330–7. https://doi.org/10.1161/ATVBAHA.114.303849.
Saviana B, Quilliot D, Ziegler O, Bigard MA, Drouin P, Guéant JL. Diagnosis of lipid malabsorption in patients with chronic pancreatitis: a new indirect test using postprandial plasma apolipoprotein B-48. Am J Gastroenterol. 1999;94:3229–35. https://doi.org/10.1111/j.1572-0241.1999.01524.x.
Taskinen M-R, Björnson E, Matikainen N, Söderlund S, Pietiläinen KH, Ainola M, et al. Effects of liraglutide on the metabolism of triglyceride-rich lipoproteins in type 2 diabetes. Diabetes Obes Metab. 2021;23:1191–201. https://doi.org/10.1111/dom.14328.
Bozzetto L, Annuzzi G, Corte GD, Patti L, Cipriano P, Mangione A, et al. Ezetimibe beneficially influences fasting and postprandial triglyceride-rich lipoproteins in type 2 diabetes. Atherosclerosis. 2011;217:142–8. https://doi.org/10.1016/j.atherosclerosis.2011.03.012.
O’Keefe SJD, Rakitt T, Ou J, El Hajj II, Blaney E, Vipperla K, et al. Pancreatic and intestinal function post Roux-en-Y gastric bypass surgery for obesity. Clin Transl Gastroenterol. 2017;8:e112. https://doi.org/10.1038/ctg.2017.39.
Käkelä P, Männistö V, Vaittinen M, Venesmaa S, Kärjä V, Virtanen K, et al. Small intestinal length associates with serum triglycerides before and after LRYGB. Obes Surg. 2018;28:3969–75. https://doi.org/10.1007/s11695-018-3447-x.
Xiao C, Bandsma RHJ, Dash S, Szeto L, Lewis GF. Exenatide, a glucagon-like peptide-1 receptor agonist, acutely inhibits intestinal lipoprotein production in healthy humans. Arterioscler Thromb Vasc Biol. 2012;32:1513–9. https://doi.org/10.1161/ATVBAHA.112.246207.
Vergès B, Duvillard L, Pais de Barros JP, Bouillet B, Baillot-Rudoni S, Rouland A, et al. Liraglutide reduces postprandial hyperlipidemia by increasing ApoB48 (Apolipoprotein B48) catabolism and by reducing ApoB48 production in patients with type 2 diabetes mellitus. Arterioscler Thromb Vasc Biol. 2018;38:2198–206. https://doi.org/10.1161/ATVBAHA.118.310990.
Fielding BA, Frayn KN. Lipoprotein lipase and the disposition of dietary fatty acids. Br J Nutr. 1998;80:495–502. https://doi.org/10.1017/s0007114598001585.
Martinussen C, Dirksen C, Bojsen-Møller KN, Svane MS, Carlsson ER, Hartmann B, et al. Intestinal sensing and handling of dietary lipids in gastric bypass-operated patients and matched controls. Am J Clin Nutr. 2019. https://doi.org/10.1093/ajcn/nqz272.
Acknowledgements
We thank Siv Hesse Jacobsen (Hvidovre Hospital, Denmark) for her important role in the practical conduct of the study. Moreover, this work relied on professional help from Dorthe Baunbjerg Nielsen, Sussi Polmann, and Alis Sloth Andersen (Hvidovre Hospital, Denmark) and Daniel Halling Breiner (Clinical Metabolomics Core Facility, Clinical Biochemistry, Rigshospitalet, Denmark).
M.H. and K.N.B.-M. are funded by a Novo Nordic Foundation Excellence Project Grant (NNF18 OC0032330).
Author information
Authors and Affiliations
Contributions
M.H. performed the statistical data analysis and graphical presentation of the results, wrote the paper, and is primarily responsible for the final content of the paper. K.N.B.-M. contributed to the design and practical conduct of the study, data generation and analysis, and discussion; and reviewed/edited the paper. V.B.K. contributed to data analysis and discussion and reviewed/edited the paper. S.M. initiated the study and together with J.J.H. and G.v.H. contributed to the design of the study, data generation and analysis and discussion, and reviewed/edited the paper. All authors approved the final version of the paper before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Hindsø, M., Bojsen-Møller, K.N., Kristiansen, V.B. et al. Early effects of Roux-en-Y gastric bypass on dietary fatty acid absorption and metabolism in people with obesity and normal glucose tolerance. Int J Obes 46, 1359–1365 (2022). https://doi.org/10.1038/s41366-022-01123-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-022-01123-1