Abstract
Background
Early prevention of hypertension is important for global cardiovascular disease morbidity and mortality. This study aims to explore better predictors for hypertension incidence related to baseline level or trajectories of adiposity indices, as well as the gender-specific effect.
Methods
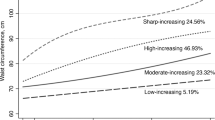
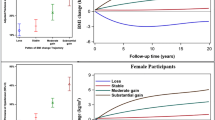
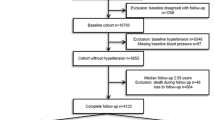
6085 subjects from a functional community cohort in urban Beijing participated in our study. Restricted cubic splines were used to estimate nonlinear associations of body mass index (BMI) and waist-to-height ratio (WHtR) as continuous variable with risk of hypertension. Stepwise logistic regression model was performed to estimate the relative risks (RRs) of adiposity indices and metabolic status, adjusted for covariates. Nomogram models and receiver operating characteristic (ROC) curve analysis was used to evaluate the predictive power of BMI trajectory groups and WHtR trajectory groups on hypertension incidence. Further, all analysis were performed by gender.
Results
The risk of hypertension incidence was related to BMI trajectory groups (persistent overweight: RR = 1.88, 95% CI: 1.48–2.37; persistent obesity: RR = 2.79, 95% CI: 2.18–3.56; persistent the highest: RR = 4.30, 95% CI: 3.20–5.78) and WHtR trajectory groups (persistent medium: RR = 2.69, 95% CI: 2.07–3.50; persistent high: RR = 3.85, 95% CI: 2.92–5.09; increasing to higher: RR = 7.00, 95% CI: 4.96–9.89). In total population, BMI trajectories and WHtR trajectories showed similar ability to predict the risk of hypertension incidence with AUC 0.723 and 0.726, respectively. After stratified by gender, both BMI trajectories and WHtR trajectories showed higher power in female than male (BMI trajectories: 0.762 vs. 0.661; WHtR trajectories: 0.768 vs. 0.661).
Conclusions
BMI and WHtR trajectories have higher predictive power for hypertension incidence compared to baseline data. Females are more vulnerable to obesity than males.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Data are available on reasonable request to the corresponding author.
References
Luo D, Cheng Y, Zhang H, Ba M, Chen P, Li H, et al. Association between high blood pressure and long term cardiovascular events in young adults: systematic review and meta-analysis. BMJ. 2020;370:m3222.
Saiz LC, Gorricho J, Garjon J, Celaya MC, Erviti J, Leache L. Blood pressure targets for the treatment of people with hypertension and cardiovascular disease. Cochrane Database Syst Rev. 2020;9:CD010315.
Yang CY, Liu JS, Tseng WC, Tsai MT, Lin MH, Kao ZK, et al. Effect of renin-angiotensin-aldosterone system blockade on long-term outcomes in postacute kidney injury patients with hypertension. Crit Care Med. 2020.
Wu X, Duan X, Gu D, Hao J, Tao S, Fan D. Prevalence of hypertension and its trends in Chinese populations. Int J Cardiol. 1995;52:39–44.
Gao Y, Chen G, Tian H, Lin L, Lu J, Weng J, et al. Prevalence of hypertension in China: a cross-sectional study. PLoS ONE. 2013;8:e65938.
Ke L, Ho J, Feng J, Mpofu E, Dibley MJ, Li Y, et al. Prevalence, awareness, treatment and control of hypertension in Macau: results from a cross-sectional epidemiological study in Macau, China. Am J Hypertens. 2015;28:159–65.
Ezzati M, Vander Hoorn S, Lawes CM, Leach R, James WP, Lopez AD, et al. Rethinking the “diseases of affluence” paradigm: global patterns of nutritional risks in relation to economic development. PLoS Med. 2005;2:e133.
Heianza Y, Kodama S, Arase Y, Hsieh SD, Yoshizawa S, Tsuji H, et al. Role of body mass index history in predicting risk of the development of hypertension in Japanese individuals: Toranomon Hospital Health Management Center Study 18 (TOPICS 18). Hypertension. 2014;64:247–52.
Wang S, Liu Y, Li F, Jia H, Liu L, Xue F. A novel quantitative body shape score for detecting association between obesity and hypertension in China. BMC Public Health. 2015;15:7.
Bohn B, Muller MJ, Simic-Schleicher G, Kiess W, Siegfried W, Oelert M, et al. BMI or BIA: is body mass index or body fat mass a better predictor of cardiovascular risk in overweight or obese children and adolescents? A German/Austrian/Swiss Multicenter APV analysis of 3,327 children and adolescents. Obes Facts. 2015;8:156–65.
Xie D, Bollag WB. Obesity, hypertension and aldosterone: is leptin the link? J Endocrinol. 2016;230:F7–F11.
Chen Y, Liang X, Zheng S, Wang Y, Lu W. Association of body fat mass and fat distribution with the incidence of hypertension in a population-based Chinese Cohort: a 22-year follow-up. J Am Heart Assoc. 2018;7.
Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D. Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: a cohort study. Lancet. 2001;358:1682–6.
Ishikawa-Takata K, Ohta T, Moritaki K, Gotou T, Inoue S. Obesity, weight change and risks for hypertension, diabetes and hypercholesterolemia in Japanese males. Eur J Clin Nutr. 2002;56:601–7.
Juntunen M, Niskanen L, Saarelainen J, Tuppurainen M, Saarikoski S, Honkanen R. Changes in body weight and onset of hypertension in perimenopausal females. J Hum Hypertens. 2003;17:775–9.
Droyvold WB, Midthjell K, Nilsen TI, Holmales J. Change in body mass index and its impact on blood pressure: a prospective population study. Int J Obes (Lond). 2005;29:650–5.
Williams PT. Increases in weight and body size increase the odds for hypertension during 7 years of follow-up. Obesity (Silver Spring). 2008;16:2541–8.
He J, Whelton PK, Appel LJ, Charleston J, Klag MJ. Long-term effects of weight loss and dietary sodium reduction on incidence of hypertension. Hypertension. 2000;35:544–9.
Stevens VJ, Obarzanek E, Cook NR, Lee IM, Appel LJ, Smith West D, et al. Long-term weight loss and changes in blood pressure: results of the Trials of Hypertension Prevention, phase II. Ann Intern Med. 2001;134:1–11.
Moore LL, Visioni AJ, Qureshi MM, Bradlee ML, Ellison RC, D’Agostino R. Weight loss in overweight adults and the long-term risk of hypertension: the Framingham study. Arch Intern Med. 2005;165:1298–303.
Despres JP. Body fat distribution and risk of cardiovascular disease: an update. Circulation. 2012;126:1301–13.
Choi JR, Koh SB, Choi E. Waist-to-height ratio index for predicting incidences of hypertension: the ARIRANG study. BMC Public Health. 2018;18:767.
Chua EY, Zalilah MS, Haemamalar K, Norhasmah S, Geeta A. Obesity indices predict hypertension among indigenous adults in Krau Wildlife Reserve, Peninsular Malaysia. J Health Popul Nutr. 2017;36:24.
Maffeis C, Banzato C, Talamini G, Obesity Study Group of the Italian Society of Pediatric E, Diabetology. Waist-to-height ratio, a useful index to identify high metabolic risk in overweight children. J Pediatr. 2008;152:207–13.
Wang XH, Lin JN, Liu GZ, Fan HM, Huang YP, Li CJ, et al. Females are at a higher risk of chronic metabolic diseases compared to males with increasing body mass index in China. Front Endocrinol (Lausanne). 2020;11:127.
Hu L, Hu G, Huang X, Zhou W, You C, Li J, et al. Different adiposity indices and their associations with hypertension among Chinese population from Jiangxi province. BMC Cardiovasc Disord. 2020;20:115.
Karelis AD, Faraj M, Bastard JP, St-Pierre DH, Brochu M, Prud’homme D, et al. The metabolically healthy but obese individual presents a favorable inflammation profile. J Clin Endocrinol Metab. 2005;90:4145–50.
Karelis AD. Metabolically healthy but obese individuals. Lancet. 2008;372:1281–3.
Marini MA, Succurro E, Frontoni S, Hribal ML, Andreozzi F, Lauro R, et al. Metabolically healthy but obese females have an intermediate cardiovascular risk profile between healthy nonobese females and obese insulin-resistant females. Diabetes Care. 2007;30:2145–7.
Zhang T, Zhang H, Li S, Li Y, Liu Y, Fernandez C, et al. Impact of adiposity on incident hypertension is modified by insulin resistance in adults: longitudinal observation from the Bogalusa Heart Study. Hypertension. 2016;67:56–62.
Saki SA, Nessa A, Salma MU, Begum A. Relationship of HDL-C and triglyceride with hypertension in adult males. Mymalessingh Med J. 2019;28:298–301.
Colman I, Ataullahjan A. Life course perspectives on the epidemiology of depression. Can J Psychiatry. 2010;55:622–32.
Guo B, Shi Z, Zhang W, Zhao H, He K, Hu X, et al. Trajectories of body mass index (BMI) and hypertension risk among middle-aged and elderly Chinese people. J Hum Hypertens. 2021;35:537–45.
Zeng Q, Sun L, Zeng Q. Trajectories of mid-life to elderly adulthood BMI and incident hypertension: the China Health and Nutrition Survey. BMJ Open. 2021;11:e047920.
Xi B, Liang Y, He T, Reilly KH, Hu Y, Wang Q, et al. Secular trends in the prevalence of general and abdominal obesity among Chinese adults, 1993–2009. Obes Rev. 2012;13:287–96.
Mi YJ, Zhang B, Wang HJ, Yan J, Han W, Zhao J, et al. Prevalence and secular trends in obesity among chinese adults, 1991–2011. Am J Prev Med. 2015;49:661–9.
Yan YX, Dong J, Liu YQ, Yang XH, Li M, Shia G, et al. Association of suboptimal health status and cardiovascular risk factors in urban Chinese workers. J Urban Health. 2012;89:329–38.
Zhang M, Zhao Y, Sun H, Luo X, Wang C, Li L, et al. Effect of dynamic change in body mass index on the risk of hypertension: results from the Rural Chinese Cohort Study. Int J Cardiol. 2017;238:117–22.
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–52.
Andruff H, Carraro Natasha, Thompson Amanda, Gaudreau Patrick, Louvet Benoît. Latent class growth modelling: a tutorial. Tutorials in Quantitative Methods for Psychology. 2009;5:11–24.
Moon S, Chung HS, Yu JM, Ko KJ, Choi DK, Kwon O, et al. The association between obesity and the nocturia in the U.S. population. Int Neurourol J. 2019;23:169–76.
Mertens IL, Van Gaal LF. Overweight, obesity, and blood pressure: the effects of modest weight reduction. Obes Res. 2000;8:270–8.
Fantin F, Giani A, Zoico E, Rossi AP, Mazzali G, Zamboni M. Weight loss and hypertension in obese subjects. Nutrients. 2019;11.
Xu J, Zhang R, Guo R, Wang Y, Dai Y, Xie Y, et al. Trajectories of body mass index and risk of incident hypertension among a normal body mass index population: A prospective cohort study. J Clin Hypertens (Greenwich). 2021;23:1212–20.
Funding
This work was supported by Grants Nos. 81573214 and 81773511 to investigator Yu-Xiang Yan from the National Natural Science Foundation of China.
Author information
Authors and Affiliations
Contributions
Ya-Ke Lu, Jing Dong, and Yu-Xiang Yan designed and conducted the study. Ya-Ke Lu cleared the data with the help of Li-Kun Hu, Yue Sun and Yu-Hong Liu. Ya-Ke Lu and Jing Dong analyzed the data and wrote the manuscript with support from Yu-Xiang Yan and Xi Chu. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Lu, YK., Dong, J., Sun, Y. et al. Gender-specific predictive ability for the risk of hypertension incidence related to baseline level or trajectories of adiposity indices: a cohort study of functional community. Int J Obes 46, 1036–1043 (2022). https://doi.org/10.1038/s41366-022-01081-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-022-01081-8