Abstract
Background
Prior studies of early antibiotic use and growth have shown mixed results, primarily on cross-sectional outcomes. This study examined the effect of oral antibiotics before age 24 months on growth trajectory at age 2–5 years.
Methods
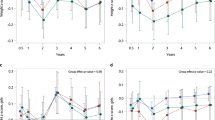
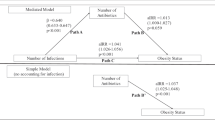
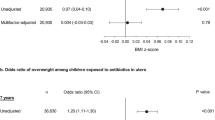
We captured oral antibiotic prescriptions and anthropometrics from electronic health records through PCORnet, for children with ≥1 height and weight at 0–12 months of age, ≥1 at 12–30 months, and ≥2 between 25 and 72 months. Prescriptions were grouped into episodes by time and by antimicrobial spectrum. Longitudinal rate regression was used to assess differences in growth rate from 25 to 72 months of age. Models were adjusted for sex, race/ethnicity, steroid use, diagnosed asthma, complex chronic conditions, and infections.
Results
430,376 children from 29 health U.S. systems were included, with 58% receiving antibiotics before 24 months. Exposure to any antibiotic was associated with an average 0.7% (95% CI 0.5, 0.9, p < 0.0001) greater rate of weight gain, corresponding to 0.05 kg additional weight. The estimated effect was slightly greater for narrow-spectrum (0.8% [0.6, 1.1]) than broad-spectrum (0.6% [0.3, 0.8], p < 0.0001) drugs. There was a small dose response relationship between the number of antibiotic episodes and weight gain.
Conclusion
Oral antibiotic use prior to 24 months of age was associated with very small changes in average growth rate at ages 2–5 years. The small effect size is unlikely to affect individual prescribing decisions, though it may reflect a biologic effect that can combine with others.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Code availability
R code developed for the analyses reported here are available at https://github.com/PEDSnet/pcornet_abx_growth_study/tree/main/lt_trajectory_analysis. Additionally, Daymont et al. have made an implementation of their anthropometric data evaluation algorithm available at https://github.com/carriedaymont/growthcleanr.
References
Chai G, Governale L, McMahon AW, Trinidad JP, Staffa J, Murphy D. Trends of outpatient prescription drug utilization in US children, 2002-2010. Pediatrics. 2012;130:23–31.
Vaz LE, Kleinman KP, Raebel MA, Nordin JD, Lakoma MD, Dutta-Linn MM, et al. Recent trends in outpatient antibiotic use in children. Pediatrics. 2014;133:375–85.
Bailey LC, Forrest CB, Zhang P, Richards TM, Livshits A, DeRusso PA. Association of antibiotics in infancy with early childhood obesity. JAMA Pediatr. 2014;168:1063–9.
Jukes TH, Williams WL. Nutritional effects of antibiotics. Pharmacol Rev. 1953;5:381–420.
Cox LM, Yamanishi S, Sohn J, Alekseyenko AV, Leung JM, Cho I, et al. Altering the intestinal microbiota during a critical developmental window has lasting metabolic consequences. Cell. 2014;158:705–21.
Haight TH, Pierce WE. Effect of prolonged antibiotic administration of the weight of healthy young males. J Nutr. 1955;56:151–61.
Marotz CA, Zarrinpar A. Treating obesity and metabolic syndrome with fecal microbiota transplantation. Yale J Biol Med. 2016;89:383–8.
Skinner AC, Ravanbakht SN, Skelton JA, Perrin EM, Armstrong SC. Prevalence of obesity and severe obesity in US children, 1999-2016. Pediatrics. 2018;141:e20173459.
Kronman MP, Zhou C, Mangione-Smith R. Bacterial prevalence and antimicrobial prescribing trends for acute respiratory tract infections. Pediatrics. 2014;134:e956–65.
Llewellyn A, Simmonds M, Owen CG, Woolacott N. Childhood obesity as a predictor of morbidity in adulthood: a systematic review and meta-analysis. Obes Rev. 2016;17:56–67.
Ajslev TA, Andersen CS, Gamborg M, Sorensen TI, Jess T. Childhood overweight after establishment of the gut microbiota: the role of delivery mode, pre-pregnancy weight and early administration of antibiotics. Int J Obes. 2011;35:522–9.
Trasande L, Blustein J, Liu M, Corwin E, Cox LM, Blaser MJ. Infant antibiotic exposures and early-life body mass. Int J Obes. 2013;37:16–23.
Azad MB, Bridgman SL, Becker AB, Kozyrskyj AL. Infant antibiotic exposure and the development of childhood overweight and central adiposity. Int J Obes. 2014;38:1290–8.
Saari A, Virta LJ, Sankilampi U, Dunkel L, Saxen H. Antibiotic exposure in infancy and risk of being overweight in the first 24 months of life. Pediatrics. 2015;135:617–26.
Gerber JS, Bryan M, Ross RK, Daymont C, Parks EP, Localio AR, et al. Antibiotic exposure during the first 6 months of life and weight gain during childhood. Jama. 2016;315:1258–65.
Rasmussen SH, Shrestha S, Bjerregaard LG, Angquist LH, Baker JL, Jess T, et al. Antibiotic exposure in early life and childhood overweight and obesity: a systematic review and meta-analysis. Diabetes Obes Metab. 2018;20:1508–14.
Shao X, Ding X, Wang B, Li L, An X, Yao Q, et al. Antibiotic exposure in early life increases risk of childhood obesity: a systematic review and meta-analysis. Front Endocrinol. 2017;8:170.
Block JP, Bailey LC, Gillman MW, Lunsford D, Daley MF, Eneli I, et al. Early antibiotic exposure and weight outcomes in young children. Pediatrics. 2018;142:e20180290.
Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. CDC growth charts for the United States: methods and development. Vital Health Stat 11. 2000;2002:1–190.
WHO Multicentre Growth Reference Study Group. WHO Child Growth Standards: Growth velocity based on weight, length and head circumference: Methods and development. Geneva, Switzerland: World Health Organization; 2009.
Rzehak P, Oddy WH, Mearin ML, Grote V, Mori TA, Szajewska H, et al. Infant feeding and growth trajectory patterns in childhood and body composition in young adulthood. Am J Clin Nutr. 2017;106:568–80.
Schwartz BS, Pollak J, Bailey-Davis L, Hirsch AG, Cosgrove SE, Nau C, et al. Antibiotic use and childhood body mass index trajectory. Int J Obes. 2016;40:615–21.
Fleurence RL, Curtis LH, Califf RM, Platt R, Selby JV, Brown JS. Launching PCORnet, a national patient-centered clinical research network. J Am Med Inform Assoc. 2014;21:578–82.
Bailey LC, Milov DE, Kelleher K, Kahn MG, Del Beccaro M, Yu F, et al. Multi-institutional sharing of electronic health record data to assess childhood obesity. PLoS ONE. 2013;8:e66192.
Block JP, Bailey LC, Gillman MW, Lunsford D, Boone-Heinonen J, Cleveland LP, et al. PCORnet antibiotics and childhood growth study: process for cohort creation and cohort description. Acad Pediatr. 2018;18:569–76.
Daymont C, Ross ME, Russell Localio A, Fiks AG, Wasserman RC, Grundmeier RW. Automated identification of implausible values in growth data from pediatric electronic health records. J Am Med Inform Assoc. 2017;24:1080–7.
Aljebab F, Choonara I, Conroy S. Systematic review of the toxicity of short-course oral corticosteroids in children. Arch Dis Child. 2016;101:365–70.
Aljebab F, Choonara I, Conroy S. Systematic review of the toxicity of long-course oral corticosteroids in children. PLoS ONE. 2017;12:e0170259.
Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr. 2014;14:199.
Fleming-Dutra KE, Shapiro DJ, Hicks LA, Gerber JS, Hersh AL. Race, otitis media, and antibiotic selection. Pediatrics. 2014;134:1059–66.
Bryan M, Heagerty PJ. Direct regression models for longitudinal rates of change. Stat Med. 2014;33:2115–36.
Lin PD, Daley MF, Boone-Heinonen J, Rifas-Shiman SL, Bailey LC, Forrest CB, et al. Comparing prescribing and dispensing data of the PCORnet common data model within PCORnet antibiotics and childhood growth study. EGEMS. 2019;7:11.
Acknowledgements
The PCORnet Childhood Antibiotic Study Team includes a diverse group of investigators, research staff, clinicians, community members, and parent caregivers. All members of the team including the study’s Executive Antibiotic Stakeholder Advisory Group (EASAG) contributed to the study design, data acquisition, and interpretation of results. The Study Team would like to thank the leaders of the participating PCORnet Clinical Research Networks (CRNs) and PCORnet Coordinating Center as well as members of the PCORI team for their support and commitment to this project. Finally, the study team is grateful to the patients, families, and clinicians at CDRN member health systems for the sharing of health-related information via PCORnet, without which the study would not have been possible.
Author information
Authors and Affiliations
Consortia
Contributions
LCB, MB, JPB, DL, and CBF conceived the study. LCB, MM, CEH, JER, JLS, and RT contributed to study data acquisition and preparation. MB, MM, LCB, RT, and CBF conducted the analyses. LCB drafted the paper, and MB, MM, and CBF contributed detailed revisions. JPB, DL, and CBF supervised the Antibiotics and Childhood Growth study. All authors contributed to critical assessment of results and provided critical review of the paper.
Corresponding author
Ethics declarations
Competing interests
This work was supported through the Patient-Centered Outcomes Research Institute (PCORI) Program Award (OBS-1505-30699). All statements in this paper are solely those of the authors and do not necessarily represent the views of PCORI, its Board of Governors, or Methodology Committee. The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Bailey, L.C., Bryan, M., Maltenfort, M. et al. Antibiotics prior to age 2 years have limited association with preschool growth trajectory. Int J Obes 46, 843–850 (2022). https://doi.org/10.1038/s41366-021-01023-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-01023-w