Abstract
Background
Little is known about the impact of timing as opposed to frequency and intensity of daily physical activity on metabolic health. Therefore, we assessed the association between accelerometery-based daily timing of physical activity and measures of metabolic health in sedentary older people.
Methods
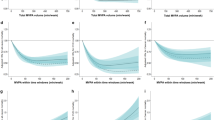
Hourly mean physical activity derived from wrist-worn accelerometers over a 6-day period was collected at baseline and after 3 months in sedentary participants from the Active and Healthy Ageing study. A principal component analysis (PCA) was performed to reduce the number of dimensions (e.g. define periods instead of separate hours) of hourly physical activity at baseline and change during follow-up. Cross-sectionally, a multivariable-adjusted linear regression analysis was used to associate the principal components, particularly correlated with increased physical activity in data-driven periods during the day, with body mass index (BMI), fasting glucose and insulin, HbA1c and the homeostatic model assessment for insulin resistance (HOMA-IR). For the longitudinal analyses, we calculated the hourly changes in physical activity and change in metabolic health after follow-up.
Results
We included 207 individuals (61.4% male, mean age: 64.8 [SD 2.9], mean BMI: 28.9 [4.7]). Higher physical activity in the early morning was associated with lower fasting glucose (−2.22%, 95% CI: −4.19, −0.40), fasting insulin (−13.54%, 95%CI: −23.49, −4.39), and HOMA-IR (−16.07%, 95%CI: −27.63, −5.65). Higher physical activity in the late afternoon to evening was associated with lower BMI (−2.84%, 95% CI: −4.92, −0.70). Higher physical activity at night was associated with higher BMI (2.86%, 95% CI: 0.90, 4.78), fasting glucose (2.57%, 95% CI: 0.70, 4.30), and HbA1c (2.37%, 95% CI: 1.00, 3.82). Similar results were present in the prospective analysis.
Conclusion
Specific physical activity timing patterns were associated with more beneficial metabolic health, suggesting particular time-dependent physical activity interventions might maximise health benefits.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Kohl HW 3rd, Craig CL, Lambert EV, Inoue S, Alkandari JR, Leetongin G, et al. The pandemic of physical inactivity: global action for public health. Lancet. 2012;380:294–305.
WHO. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:1–253. i-xii.
WHO. Global recommendations on physical activity for health. Switserland:WHO;2010.
Sun F, Norman IJ, While AE. Physical activity in older people: a systematic review. BMC Public Health. 2013;13:449.
Braskie MN, Boyle CP, Rajagopalan P, Gutman BA, Toga AW, Raji CA, et al. Physical activity, inflammation, and volume of the aging brain. Neuroscience. 2014;273:199–209.
Notthoff N, Reisch P, Gerstorf D. Individual Characteristics and Physical Activity in Older Adults: a systematic review. Gerontology. 2017;63:443–59.
Lewis P, Korf HW, Kuffer L, Gross JV, Erren TC. Exercise time cues (zeitgebers) for human circadian systems can foster health and improve performance: a systematic review. BMJ Open Sport Exerc Med. 2018;4:e000443.
Marinac CR, Quante M, Mariani S, Weng J, Redline S, Cespedes Feliciano EM, et al. Associations Between Timing of Meals, Physical Activity, Light Exposure, and Sleep With Body Mass Index in Free-Living Adults. J Phys Act Health. 2019;16:214–21.
Rijks Instituut voor Volksgezondheid en Milieu (RIVM): Volwassenen met overgewicht en obesitas 2020. https://www.volksgezondheidenzorg.info/onderwerp/overgewicht/cijfers-context/huidige-situatie#node-overgewicht-volwassenen. (last assessed November 12, 2021).
Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, et al. The Physical Activity Guidelines for Americans. JAMA. 2018;320:2020–8.
Chomistek AK, Shiroma EJ, Lee IM. The Relationship Between Time of Day of Physical Activity and Obesity in Older Women. J Phys Act Health. 2016;13:416–8.
Reid KJ, Santostasi G, Baron KG, Wilson J, Kang J, Zee PC. Timing and intensity of light correlate with body weight in adults. PLoS ONE. 2014;9:e92251.
Garaulet M, Gomez-Abellan P. Timing of food intake and obesity: a novel association. Physiol Behav. 2014;134:44–50.
Garaulet M, Gomez-Abellan P, Alburquerque-Bejar JJ, Lee YC, Ordovas JM, Scheer FA. Timing of food intake predicts weight loss effectiveness. Int J Obes (Lond). 2013;37:604–11.
Dashti HS, Scheer F, Saxena R, Garaulet M. Timing of Food Intake: Identifying Contributing Factors to Design Effective Interventions. Adv Nutr. 2019;10:606–20.
de Cabo R, Mattson MP. Effects of Intermittent Fasting on Health, Aging, and Disease. N Engl J Med. 2019;381:2541–51.
Lu TC, Fu CM, Ma MH, Fang CC, Turner AM. Healthcare Applications of Smart Watches. A Systematic Review. Appl Clin Inform. 2016;7:850–69.
Piwek L, Ellis DA, Andrews S, Joinson A. The Rise of Consumer Health Wearables: Promises and Barriers. PLoS Med. 2016;13:e1001953.
Jim HSL, Hoogland AI, Brownstein NC, Barata A, Dicker AP, Knoop H, et al. Innovations in Research and Clinical Care Using Patient-Generated Health Data. CA Cancer J Clin. 2020;70:182–99.
Migueles JH, Rowlands A, Huber F, Sabia S, van Hees VT. GGIR: A Research Community–Driven Open Source R Package for Generating Physical Activity and Sleep Outcomes From Multi-Day Raw Accelerometer Data. J Measurement Phys Behav. 2019;2:188–96.
van Kuppevelt D, Heywood J, Hamer M, Sabia S, Fitzsimons E, van Hees V. Segmenting accelerometer data from daily life with unsupervised machine learning. PLoS ONE. 2019;14:e0208692.
Willis EA, Creasy SA, Honas JJ, Melanson EL, Donnelly JE. The effects of exercise session timing on weight loss and components of energy balance: midwest exercise trial 2. Int J Obes (Lond). 2020;44:114–24.
Wijsman CA, Westendorp RG, Verhagen EA, Catt M, Slagboom PE, de Craen AJ, et al. Effects of a web-based intervention on physical activity and metabolism in older adults: randomized controlled trial. J Med Internet Res. 2013;15:e233.
van Hees VT, Fang Z, Langford J, Assah F, Mohammad A, da Silva IC, et al. Autocalibration of accelerometer data for free-living physical activity assessment using local gravity and temperature: an evaluation on four continents. J Appl Physiol (1985). 2014;117:738–44.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Schumacher LM, Thomas JG, Raynor HA, Rhodes RE, Bond DS. Consistent Morning Exercise May Be Beneficial for Individuals With Obesity. Exerc Sport Sci Rev. 2020;48:201–8.
Brooker PG, Gomersall SR, King NA, Leveritt MD. The feasibility and acceptability of morning versus evening exercise for overweight and obese adults: A randomized controlled trial. Contemp Clin Trials Commun. 2019;14:100320.
Di Blasio A, Di Donato F, Mastrodicasa M, Fabrizio N, Di Renzo D, Napolitano G, et al. Effects of the time of day of walking on dietary behaviour, body composition and aerobic fitness in post-menopausal women. J Sports Med Phys Fitness. 2010;50:196–201.
Henson J, Rowlands AV, Baldry E, Brady EM, Davies MJ, Edwardson CL, et al. Physical behaviors and chronotype in people with type 2 diabetes. BMJ Open Diabetes Res Care. 2020;8:e001375.
Facer-Childs ER, Boiling S, Balanos GM. The effects of time of day and chronotype on cognitive and physical performance in healthy volunteers. Sports Med Open. 2018;4:47.
Vera B, Dashti HS, Gomez-Abellan P, Hernandez-Martinez AM, Esteban A, Scheer F, et al. Modifiable lifestyle behaviors, but not a genetic risk score, associate with metabolic syndrome in evening chronotypes. Sci Rep. 2018;8:945.
Dekker SA, Noordam R, Biermasz NR, de Roos A, Lamb HJ, Rosendaal FR, et al. Habitual Sleep Measures are Associated with Overall Body Fat, and not Specifically with Visceral Fat, in Men and Women. Obesity (Silver Spring). 2018;26:1651–8.
Hirotsu C, Tufik S, Andersen ML. Interactions between sleep, stress, and metabolism: from physiological to pathological conditions. Sleep Sci. 2015;8:143–52.
Hower IM, Harper SA, Buford TW. Circadian Rhythms, Exercise, and Cardiovascular Health. J Circadian Rhythms. 2018;16:7.
Stenvers DJ, Scheer F, Schrauwen P, la Fleur SE, Kalsbeek A. Circadian clocks and insulin resistance. Nat Rev Endocrinol. 2019;15:75–89.
Akintola AA, Noordam R, Jansen SW, de Craen AJ, Ballieux BE, Cobbaert CM, et al. Accuracy of Continuous Glucose Monitoring Measurements in Normo-Glycemic Individuals. PLoS ONE. 2015;10:e0139973.
Park S, Jastremski CA, Wallace JP. Time of day for exercise on blood pressure reduction in dipping and nondipping hypertension. J Hum Hypertens. 2005;19:597–605.
Funding
The AGO study was financially supported by Philips Consumer Lifestyle, and the Netherlands Genomics Initiative/Netherlands Organisation for Scientific Research (NGI/NOW) (grant numbers: 05040202 and 050–060–810). DvH and RN were supported by the VELUX Stiftung (grant number 1156). RN was supported by an innovation grant from the Dutch Heart Foundation [grant number 2019T103]. The funders had no role in the design, analyses and interpretation of the results of the study.
Author information
Authors and Affiliations
Contributions
GA, MS, DvH, and RN conceptualised the study. GA performed the data analysis. GA, MS, DvH, and RN contributed to the interpretation of the data. CAW, SPM, FvdO, DvH, and PES contributed to the study design and CAW and SPM performed the data collection. PES, FvdO, SPM, DvH, and RN contributed to the funding acquisition. The drafting of the initial version of the paper was done by GA and RN. All authors critically revised the paper for important intellectual content. All authors read and approved the final paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Albalak, G., Stijntjes, M., Wijsman, C.A. et al. Timing of objectively-collected physical activity in relation to body weight and metabolic health in sedentary older people: a cross-sectional and prospective analysis. Int J Obes 46, 515–522 (2022). https://doi.org/10.1038/s41366-021-01018-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-01018-7
This article is cited by
-
Deep learning of movement behavior profiles and their association with markers of cardiometabolic health
BMC Medical Informatics and Decision Making (2024)
-
Machine learning in physical activity, sedentary, and sleep behavior research
Journal of Activity, Sedentary and Sleep Behaviors (2024)
-
Association between circadian physical activity trajectories and incident type 2 diabetes in the UK Biobank
Scientific Reports (2024)
-
Effects of the Timing of Intense Physical Activity on Hypertension Risk in a General Population: A UK-Biobank Study
Current Hypertension Reports (2024)