Abstract
Background
Relationship between BMI and all-cause mortality in patients with hypertension remains controversial. This study aimed to evaluate the time-varying association between BMI in patients with hypertension and all-cause mortality.
Methods
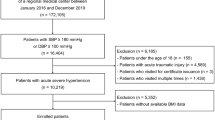
This population-based cohort study included 212,394 Chinese adults with hypertension from 2007 to 2015 and was followed up until death, loss-to-follow-up, or December 31, 2018. According to the World Health Organization criteria for Asians, BMI was categorized into five groups: underweight (BMI < 18.5 kg/m2), normal weight (18.5–22.9 kg/m2), overweight (23–24.9 kg/m2), class I obesity (25–29.9 kg/m2) and class II obesity (BMI ≥ 30 kg/m2). Cox model was used to estimate the time-varying association of BMI on the risk of mortality by including the interaction term between BMI and time using restricted cubic spline.
Results
Compared with normal weight, underweight and class II obesity were associated with higher mortality (Hazard ratio [HRs] at 1 and 10 years of follow-up: 1.51 [95% CI: 1.39–1.65], and 1.27 (1.15–1.41) for underweight, respectively; 1.08 (0.96–1.21), and 1.16 (1.03–1.30) for class II obesity, respectively). However, overweight and class I obesity were associated with lower mortality, although the protective effects gradually attenuated over time (HRs at 1 and 10 years of follow-up: 0.85 (0.81–0.90), and 0.96 (0.91–1.02) for overweight, respectively; 0.80 (0.76–0.84), and 1.04 (0.99–1.10) for class I obesity, respectively).
Conclusions
We found increased mortality among hypertensive patients with underweight and class II obesity while decreased mortality with overweight and class I obesity was observed during the first 5 years of follow-up. Management efforts for hypertension may target controlling body weight in a reasonable range for patients, and probably more attention should be given to underweight patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The datasets generated and analyzed in the study are not publicly available but are available from the corresponding authors on reasonable request.
References
Collaborators GCoD. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736–88.
Collaborators GRF. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1923–94.
Chow CK, Gupta R. Blood pressure control: a challenge to global health systems. Lancet. 2019;394:613–5.
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017;390:2627–42.
Hossain FB, Adhikary G, Chowdhury AB, Shawon MSR. Association between body mass index (BMI) and hypertension in south Asian population: evidence from nationally-representative surveys. Clin Hypertens. 2019;25:28.
Shihab HM, Meoni LA, Chu AY, Wang NY, Ford DE, Liang KY, et al. Body mass index and risk of incident hypertension over the life course: the Johns Hopkins Precursors Study. Circulation. 2012;126:2983–9.
Adams KF, Schatzkin A, Harris TB, Kipnis V, Mouw T, Ballard-Barbash R, et al. Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N Engl J Med. 2006;355:763–78.
Zheng W, McLerran DF, Rolland B, Zhang X, Inoue M, Matsuo K, et al. Association between body-mass index and risk of death in more than 1 million Asians. N Engl J Med. 2011;364:719–29.
Bastien M, Poirier P, Lemieux I, Després JP. Overview of epidemiology and contribution of obesity to cardiovascular disease. Prog Cardiovasc Dis. 2014;56:369–81.
Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet. 2008;371:569–78.
Landi F, Calvani R, Picca A, Tosato M, Martone AM, Ortolani E, et al. Body Mass Index is Strongly Associated with Hypertension: Results from the Longevity Check-up 7+. Study. Nutrients. 2018;10:1976.
Linderman GC, Lu J, Lu Y, Sun X, Xu W, Nasir K, et al. Association of Body Mass Index With Blood Pressure Among 1.7 Million Chinese Adults. JAMA Netw Open. 2018;1:e181271.
Booth HP, Prevost AT, Gulliford MC. Severity of obesity and management of hypertension, hypercholesterolaemia and smoking in primary care: population-based cohort study. J Hum Hypertens. 2016;30:40–5.
Aune D, Sen A, Prasad M, Norat T, Janszky I, Tonstad S, et al. BMI and all cause mortality: systematic review and non-linear dose-response meta-analysis of 230 cohort studies with 3.74 million deaths among 30.3 million participants. Bmj. 2016;353:i2156.
Mancia G, Fagard R, Narkiewicz K, Redón J, Zanchetti A, Böhm M, et al. ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2013. 2013;31:1281–357.
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. Evidence-Based Guideline for the Management of High Blood Pressure in Adults. JAMA. 2014;311:507–20.
Jayedi A, Shab-Bidar S. Nonlinear dose-response association between body mass index and risk of all-cause and cardiovascular mortality in patients with hypertension: A meta-analysis. Obes Res Clin Pract. 2018;12:16–28.
Chung WS, Ho FM, Cheng NC, Lee MC, Yeh CJ. BMI and all-cause mortality among middle-aged and older adults in Taiwan: a population-based cohort study. Public Health Nutr. 2015;18:1839–46.
McAuley PA, Sui X, Church TS, Hardin JW, Myers JN, Blair SN. The joint effects of cardiorespiratory fitness and adiposity on mortality risk in men with hypertension. Am J Hypertens. 2009;22:1062–9.
Yang W, Li JP, Zhang Y, Fan FF, Xu XP, Wang BY, et al. Association between Body Mass Index and All-Cause Mortality in Hypertensive Adults: Results from the China Stroke Primary Prevention Trial (CSPPT). Nutrients. 2016;8:384.
Li K, Yao C, Yang X, Di X, Li N, Dong L, et al. Body Mass Index and the Risk of Cardiovascular and All-Cause Mortality Among Patients With Hypertension: A Population-Based Prospective Cohort Study Among Adults in Beijing, China. J Epidemiol. 2016;26:654–60.
Xu W, Shubina M, Goldberg SI, Turchin A. Body mass index and all-cause mortality in patients with hypertension. Obesity. 2015;23:1712–20.
Barrett-Connor E, Khaw KT. Is hypertension more benign when associated with obesity? Circulation. 1985;72:53–60.
Esler M, Lambert G, Schlaich M, Dixon J, Sari CI, Lambert E. Obesity Paradox in Hypertension: Is This Because Sympathetic Activation in Obesity-Hypertension Takes a Benign Form? Hypertension. 2018;71:22–33.
Uretsky S, Messerli FH, Bangalore S, Champion A, Cooper-Dehoff RM, Zhou Q, et al. Obesity paradox in patients with hypertension and coronary artery disease. Am J Med. 2007;120:863–70.
Wang Y, Wang Y, Qain Y, Zhang J, Tang X, Sun J, et al. Association of body mass index with cause specific deaths in Chinese elderly hypertensive patients: Minhang community study. PLoS One. 2013;8:e71223.
Elagizi A, Kachur S, Lavie CJ, Carbone S, Pandey A, Ortega FB, et al. An Overview and Update on Obesity and the Obesity Paradox in Cardiovascular Diseases. Prog Cardiovasc Dis. 2018;61:142–50.
Kim S, Jeong JC, Ahn SY, Doh K, Jin DC, Na KY. Time-varying effects of body mass index on mortality among hemodialysis patients: Results from a nationwide Korean registry. Kidney Res Clin Pract. 2019;38:90–99.
Yu JM, Kong QY, Schoenhagen P, Shen T, He YS, Wang JW, et al. The prognostic value of long-term visit-to-visit blood pressure variability on stroke in real-world practice: a dynamic cohort study in a large representative sample of Chinese hypertensive population. Int J Cardiol. 2014;177:995–1000.
Organization WH Health Topic. In: Hypertension. https://www.who.int/health-topics/hypertension/#tab=tab_1.
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International Society of Hypertension global hypertension practice guidelines. J Hypertens. 2020;38:982–1004.
Consultation WHOE. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63.
Shanghai Municipal Center For Disease Control & Prevention. In. https://www.scdc.sh.cn/.
Williams TC, Bach CC, Matthiesen NB, Henriksen TB, Gagliardi L. Directed acyclic graphs: a tool for causal studies in paediatrics. Pediatr Res. 2018;84:487–93.
Hess KR. Assessing time-by-covariate interactions in proportional hazards regression models using cubic spline functions. Stat Med. 1994;13:1045–62.
Heinzl H, Kaider A. Gaining more flexibility in Cox proportional hazards regression models with cubic spline functions. Comput Methods Programs Biomed. 1997;54:201–8.
Núñez E, Steyerberg EW, Núñez J. [Regression modeling strategies]. Rev Esp Cardiol. 2011;64:501–7.
Ferrannini E, Cushman WC. Diabetes and hypertension: the bad companions. Lancet. 2012;380:601–10.
Suvila K, Langén V, Cheng S, Niiranen TJ. Age of Hypertension Onset: Overview of Research and How to Apply in Practice. Curr Hypertens Rep. 2020;22:68.
Cheng S, Xanthakis V, Sullivan LM, Vasan RS. Blood pressure tracking over the adult life course: patterns and correlates in the Framingham heart study. Hypertension. 2012;60:1393–9.
Spahillari A, Mukamal KJ, DeFilippi C, Kizer JR, Gottdiener JS, Djoussé L, et al. The association of lean and fat mass with all-cause mortality in older adults: The Cardiovascular Health Study. Nutr Metab Cardiovasc Dis. 2016;26:1039–47.
Tan BH, Fearon KC. Cachexia: prevalence and impact in medicine. Curr Opin Clin Nutr Metab Care. 2008;11:400–7.
Stamler R, Ford CE, Stamler J. Why do lean hypertensives have higher mortality rates than other hypertensives? Findings of the Hypertension Detection and Follow-up Program. Hypertension. 1991;17:553–64.
Flegal KM, Graubard BI, Williamson DF, Cooper RS. Reverse causation and illness-related weight loss in observational studies of body weight and mortality. Am J Epidemiol. 2011;173:1–9.
Lavie CJ, Milani RV, Ventura HO. Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss. J Am Coll Cardiol. 2009;53:1925–32.
Lavie CJ, McAuley PA, Church TS, Milani RV, Blair SN. Obesity and cardiovascular diseases: implications regarding fitness, fatness, and severity in the obesity paradox. J Am Coll Cardiol. 2014;63:1345–54.
Doehner W, Clark A, Anker SD. The obesity paradox: weighing the benefit. Eur Heart J. 2010;31:146–8.
Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. Jama. 2013;309:71–82.
Romero-Corral A, Montori VM, Somers VK, Korinek J, Thomas RJ, Allison TG, et al. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies. Lancet. 2006;368:666–78.
Carnethon MR, De Chavez PJ, Biggs ML, Lewis CE, Pankow JS, Bertoni AG, et al. Association of weight status with mortality in adults with incident diabetes. Jama. 2012;308:581–90.
Lainscak M, von Haehling S, Doehner W, Anker SD. The obesity paradox in chronic disease: facts and numbers. J Cachexia Sarcopenia Muscle. 2012;3:1–4.
Wessel TR, Arant CB, Olson MB, Johnson BD, Reis SE, Sharaf BL, et al. Relationship of physical fitness vs body mass index with coronary artery disease and cardiovascular events in women. Jama. 2004;292:1179–87.
Blair SN, Kampert JB, Kohl HW 3rd, Barlow CE, Macera CA, Paffenbarger RS Jr, et al. Influences of cardiorespiratory fitness and other precursors on cardiovascular disease and all-cause mortality in men and women. Jama. 1996;276:205–10.
Artero EG, Lee DC, Ruiz JR, Sui X, Ortega FB, Church TS, et al. A prospective study of muscular strength and all-cause mortality in men with hypertension. J Am Coll Cardiol. 2011;57:1831–7.
Carbone S, Lavie CJ, Arena R. Obesity and Heart Failure: Focus on the Obesity Paradox. Mayo Clin Proc. 2017;92:266–79.
Dixon JB, Lambert GW. The obesity paradox-a reality that requires explanation and clinical interpretation. Atherosclerosis. 2013;226:47–8.
Mohamed-Ali V, Goodrick S, Bulmer K, Holly JM, Yudkin JS, Coppack SW. Production of soluble tumor necrosis factor receptors by human subcutaneous adipose tissue in vivo. Am J Physiol. 1999;277:E971–5.
Feldman AM, Combes A, Wagner D, Kadakomi T, Kubota T, Li YY, et al. The role of tumor necrosis factor in the pathophysiology of heart failure. J Am Coll Cardiol. 2000;35:537–44.
Oreopoulos A, Kalantar-Zadeh K, Sharma AM, Fonarow GC. The obesity paradox in the elderly: potential mechanisms and clinical implications. Clin Geriatr Med. 2009;25:643–59.
Cornier MA, Després JP, Davis N, Grossniklaus DA, Klein S, Lamarche B, et al. Assessing adiposity: a scientific statement from the American Heart Association. Circulation. 2011;124:1996–2019.
Sarwer DB, Polonsky HM. The Psychosocial Burden of Obesity. Endocrinol Metab Clin North Am. 2016;45:677–88.
Acknowledgements
The authors would like to thank the research participants and the staff of the Minhang District community in Shanghai, China for their contributions to the research.
Funding
This study was supported by Shanghai Municipal Nature Science Foundation (19ZR1445900), Nature Science Foundation of Minhang district, Shanghai, China (2020MHZ043), the National Nature Science Foundation of China (NO: 11871164 and No 82073570), Minhang district key disciplines in public health (MGWXK01) and Health Consortium Foundation of Fudan University and Minhang District Health Committee (NO: 2019FM02).
Author information
Authors and Affiliations
Contributions
YFY, HLX, and GYQ had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. YFY, HLX, and GYQ conceived the idea, JJZ and HLX conducted data extraction and statistical analyses. JJZ wrote the first draft of the manuscript. JLZ, JL, and LLC involved in data acquisition and check. YFY, HLX, and GYQ contributed to data interpretation. All authors revised the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests
Ethics approval and consent to participate
The study was approved by the Institutional Review Board of center for disease control and prevention in Minhang District, Shanghai (NO: EC-P-2019-009). Informed consent from participants involved in the study was waived due to the fact that anonymized data compiled from electronic medical records was applied in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Zhu, J., Liu, X., Zhang, J. et al. Time-varying association between body mass index and all-cause mortality in patients with hypertension. Int J Obes 46, 316–324 (2022). https://doi.org/10.1038/s41366-021-00994-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-00994-0
This article is cited by
-
Age-specific association of stage of hypertension at diagnosis with cardiovascular and all-cause mortality among elderly patients with hypertension: a cohort study
BMC Cardiovascular Disorders (2023)
-
Obesity indices and the risk of total and cardiovascular mortality among people with diabetes: a long-term follow-up study in Taiwan
Cardiovascular Diabetology (2023)