Abstract
Background/Objectives
While an increased risk for substance use disorders (SUD) and also for several adverse pregnancy and birth outcomes in patients who have undergone bariatric surgery have been well documented when considered separately, an association between these important risk factors has not been investigated. This study explored the potential dependence of these two bariatric surgery-related risks.
Subjects/Methods
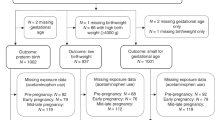
This study was a retrospective cohort study with adult women (18–45) who underwent bariatric surgery between 1996 and 2016 and who gave birth after surgery between 1996 and 2018. The study population consisted of 1849 post-bariatric surgery women with 3010 reported post-surgical births. Subjects with post-surgical, prenatal SUD were identified based on diagnosis codes extracted within the 10 months prior to delivery. Using random-effects logistic regression with retrospective cohort data, preterm birth, low birth weight, macrosomia, Caesarian delivery, congenital anomalies, and neonatal intensive care unit admission were considered as outcomes.
Results
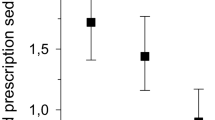
About 10% (n = 289) of women had an SUD diagnosis within 10 months prior to child delivery. Women with SUD during pregnancy had significantly more pregnancy and birth complications compared to women without SUD: preterm birth (OR = 2.08, p = 0.03, 95% CI: 1.07–4.03), low birth weight (OR = 3.41, p < 0.01, 95% CI: 1.99–5.84), Caesarian delivery (OR = 9.71, p < 0.01, 95% CI: 2.69–35.05), and neonatal intensive care unit admission (OR = 3.87, p < 0.01, 95% CI: 2.04–7.34). Women with SUD had lower risk for macrosomia than women without SUD (OR = 0.07, p = 0.02, 95% CI: 0.01–0.70).
Conclusion
Results from this study demonstrated that post-bariatric surgery women who had SUD during pregnancy had significantly more pregnancy- and birth-related complications than post-surgery pregnant women without SUD, despite the reduction in macrosomia. Where possible, greater prenatal surveillance of post-surgery women with SUD should be considered.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Adams TD, Davidson LE, Litwin SE, Kim J, Kolotkin RL, Nanjee MN, et al. Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med. 2017;377:1143–55.
Adams TD, Davidson LE, Litwin SE, Kolotkin RL, LaMonte MJ, Pendleton RC, et al. Health benefits of gastric bypass surgery after 6 years. JAMA. 2012;308:1122–31.
Arterburn DE, Telem DA, Kushner RF, Courcoulas AP. Benefits and risks of bariatric surgery in adults: a review. JAMA. 2020;324:879–87.
Kolotkin RL, Kim J, Davidson LE, Crosby RD, Hunt SC, Adams TD. 12-year trajectory of health-related quality of life in gastric bypass patients versus comparison groups. Surg Obes Relat Dis. 2018;14:1359–65.
Flolo TN, Tell GS, Kolotkin RL, Aasprang A, Norekval TM, Vage V, et al. Changes in quality of life 5 years after sleeve gastrectomy: a prospective cohort study. BMJ Open. 2019;9:e031170.
Versteegden DPA, Van Himbeeck MJJ, Nienhuijs SW. Improvement in quality of life after bariatric surgery: sleeve versus bypass. Surg Obes Relat Dis. 2018;14:170–4.
Kwong W, Tomlinson G, Feig DS. Maternal and neonatal outcomes after bariatric surgery; a systematic review and meta-analysis: do the benefits outweigh the risks? Am J Obstet Gynecol. 2018;218:573–80.
Rottenstreich A, Elchalal U, Kleinstern G, Beglaibter N, Khalaileh A, Elazary R. Maternal and perinatal outcomes after laparoscopic sleeve gastrectomy. Obstet Gynecol. 2018;131:451–6.
Bramming M, Becker U, Jorgensen MB, Neermark S, Bisgaard T, Tolstrup JS. Bariatric surgery and risk of alcohol use disorder: a register-based cohort study. Int J Epidemiol. 2021;49:1826–35.
Conason A, Teixeira J, Hsu CH, Puma L, Knafo D, Geliebter A. Substance use following bariatric weight loss surgery. JAMA Surg. 2013;148:145–50.
Young MT, Phelan MJ, Nguyen NT. A decade analysis of trends and outcomes of male vs female patients who underwent bariatric surgery. J Am Coll Surg. 2016;222:226–31.
Courcoulas A, Coley RY, Clark JM, McBride CL, Cirelli E, McTigue K, et al. Interventions and operations 5 years after bariatric surgery in a cohort from the US National Patient-Centered Clinical Research Network Bariatric Study. JAMA Surg. 2020;155:194–204.
Maggard MA, Yermilov I, Li Z, Maglione M, Newberry S, Suttorp M, et al. Pregnancy and fertility following bariatric surgery: a systematic review. JAMA. 2008;300:2286–96.
Bennett WL, Gilson MM, Jamshidi R, Burke AE, Segal JB, Steele KE, et al. Impact of bariatric surgery on hypertensive disorders in pregnancy: retrospective analysis of insurance claims data. BMJ. 2010;340:c1662.
Adams TD, Hammoud AO, Davidson LE, Laferrere B, Fraser A, Stanford JB, et al. Maternal and neonatal outcomes for pregnancies before and after gastric bypass surgery. Int J Obes (Lond). 2015;39:686–94.
Ciangura C, Coupaye M, Deruelle P, Gascoin G, Calabrese D, Cosson E, et al. Clinical practice guidelines for childbearing female candidates for bariatric surgery, pregnancy, and post-partum management after bariatric surgery. Obes Surg. 2019;29:3722–34.
Parent B, Martopullo I, Weiss NS, Khandelwal S, Fay EE, Rowhani-Rahbar A. Bariatric surgery in women of childbearing age, timing between an operation and birth, and associated perinatal complications. JAMA Surg. 2017;152:128–35.
Roos N, Neovius M, Cnattingius S, Trolle Lagerros Y, Saaf M, Granath F, et al. Perinatal outcomes after bariatric surgery: nationwide population based matched cohort study. BMJ. 2013;347:f6460.
Ibrahim N, Alameddine M, Brennan J, Sessine M, Holliday C, Ghaferi AA. New onset alcohol use disorder following bariatric surgery. Surg Endosc. 2019;33:2521–30.
King WC, Chen JY, Mitchell JE, Kalarchian MA, Steffen KJ, Engel SG, et al. Prevalence of alcohol use disorders before and after bariatric surgery. JAMA. 2012;307:2516–25.
Svensson PA, Anveden A, Romeo S, Peltonen M, Ahlin S, Burza MA, et al. Alcohol consumption and alcohol problems after bariatric surgery in the Swedish obese subjects study. Obesity (Silver Spring). 2013;21:2444–51.
Maciejewski ML, Smith VA, Berkowitz TSZ, Arterburn DE, Mitchell JE, Olsen MK, et al. Association of bariatric surgical procedures with changes in unhealthy alcohol use among US veterans. JAMA Netw Open. 2020;3:e2028117.
King WC, Chen JY, Belle SH, Courcoulas AP, Dakin GF, Flum DR, et al. Use of prescribed opioids before and after bariatric surgery: prospective evidence from a U.S. multicenter cohort study. Surg Obes Relat Dis. 2017;13:1337–46.
Maciejewski ML, Smith VA, Berkowitz TSZ, Arterburn DE, Bradley KA, Olsen MK, et al. Long-term opioid use after bariatric surgery. Surg Obes Relat Dis. 2020;16:1100–10.
Fernandez AC. Unhealthy alcohol use-a common iatrogenic complication of bariatric surgery. JAMA Netw Open. 2020;3:e2028222.
Centers for Disease Control and Prevention. Preterm Birth 2021. Updated 30 Oct 2020. Accessed date: 12 Jan 2021. https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pretermbirth.htm#:~:text=Preterm%20birth%20is%20when%20a,born%20in%20the%20United%20States.
Johansson K, Cnattingius S, Naslund I, Roos N, Trolle Lagerros Y, Granath F, et al. Outcomes of pregnancy after bariatric surgery. N Engl J Med. 2015;372:814–24.
Centers for Medicare and Medicaid Services. Chronic Conditions Data Warehouse. 2021. Accessed date: January 12, 2021. https://www2.ccwdata.org/web/guest/condition-categories.
Backman O, Stockeld D, Rasmussen F, Naslund E, Marsk R. Alcohol and substance abuse, depression and suicide attempts after Roux-en-Y gastric bypass surgery. Br J Surg. 2016;103:1336–42.
King WC, Chen JY, Courcoulas AP, Dakin GF, Engel SG, Flum DR, et al. Alcohol and other substance use after bariatric surgery: prospective evidence from a U.S. multicenter cohort study. Surg Obes Relat Dis. 2017;13:1392–402.
Akhter Z, Rankin J, Ceulemans D, Ngongalah L, Ackroyd R, Devlieger R, et al. Pregnancy after bariatric surgery and adverse perinatal outcomes: a systematic review and meta-analysis. PLoS Med. 2019;16:e1002866.
American College of Obstetricians and Gynecologists. Opioid use and opioid use disorder in pregnancy. Committee Opinion No. 711. Obstet Gynecol. 2017;130:e81–e94.
Substance Abuse and Mental Health Services Administration. Clinical guidance for treating pregnant and parenting women with opioid use disorder and their infants. HHS Publication No. (SMA) 18-5054. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2018. https://store.samhsa.gov/sites/default/files/d7/priv/sma18-5054.pdf.
American Society of Addiction Medicine. Public policy statement on substance use, misuse, and use disorders during and following pregnancy with an emphasis on opioids. 2017 Accessed date: August 09, 2021. https://www.asam.org/docs/default-source/public-policy-statements/substance-use-misuse-and-use-disorders-during-and-following-pregnancy.pdf?sfvrsn=644978c2_4.
Funding
Partial support for all datasets within the Utah Population Database was provided by the University of Utah Huntsman Cancer Institute and the Huntsman Cancer Institute Cancer Center Support grant (grant number P30 CA2014) from the National Cancer Institute.
Author information
Authors and Affiliations
Contributions
JK and TA had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: JK. Acquisition, analysis, or interpretation of data: all authors. Drafting of the manuscript: JK and TA. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: JK and SH. Administrative, technical, or material support: JK, TA, and LD. Supervision: JK and TA.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Kim, J., Davidson, L., Hunt, S. et al. Association of prenatal substance use disorders with pregnancy and birth outcomes following bariatric surgery. Int J Obes 46, 107–112 (2022). https://doi.org/10.1038/s41366-021-00964-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-00964-6
This article is cited by
-
Benefits and Risks of Bariatric Surgery on Women’s Reproductive Health: a Narrative Review
Obesity Surgery (2023)
-
Association of Pre-operative Arthritis with Long-Term Mortality Following Bariatric Surgery
Journal of Gastrointestinal Surgery (2023)
-
Pre-Operative Substance Use Disorder is Associated with Higher Risk of Long-Term Mortality Following Bariatric Surgery
Obesity Surgery (2023)
-
Pregnant Women Following Bariatric Surgery: a Focus on Maternal Mental Health and Its Impact on Birth Outcomes
Obesity Surgery (2022)
-
Risk factors of lower birth weight, small-for-gestational-age infants, and preterm birth in pregnancies following bariatric surgery: a scoping review
Archives of Gynecology and Obstetrics (2022)