Abstract
Background
Observational and Mendelian randomization (MR) studies link obesity and cancer, but it remains unclear whether these depend upon related metabolic abnormalities.
Methods
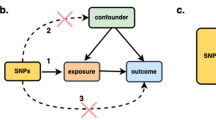
We used information from 321,472 participants in the UK biobank, including 30,561 cases of obesity-related cancer. We constructed three genetic instruments reflecting higher adiposity together with either “unfavourable” (82 SNPs), “favourable” (24 SNPs) or “neutral” metabolic profile (25 SNPs). We looked at associations with 14 types of cancer, previously suggested to be associated with obesity.
Results
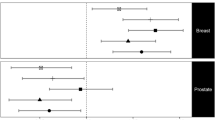
All genetic instruments had a strong association with BMI (p < 1 × 10−300 for all). The instrument reflecting unfavourable adiposity was also associated with higher CRP, HbA1c and adverse lipid profile, while instrument reflecting metabolically favourable adiposity was associated with lower HbA1c and a favourable lipid profile. In MR-inverse-variance weighted analysis unfavourable adiposity was associated with an increased risk of non-hormonal cancers (OR = 1.22, 95% confidence interval [CI]:1.08, 1.38), but a lower risk of hormonal cancers (OR = 0.80, 95%CI: 0.72, 0.89). From individual cancers, MR analyses suggested causal increases in the risk of multiple myeloma (OR = 1.36, 95%CI: 1.09, 1.70) and endometrial cancer (OR = 1.77, 95%CI: 1.16, 2.68) by greater genetically instrumented unfavourable adiposity but lower risks of breast and prostate cancer (OR = 0.72, 95%CI: 0.61, 0.83 and OR = 0.81, 95%CI: 0.68, 0.97, respectively). Favourable or neutral adiposity were not associated with the odds of any individual cancer.
Conclusions
Higher adiposity associated with a higher risk of non-hormonal cancer but a lower risk of some hormone related cancers. Presence of metabolic abnormalities might aggravate the adverse effects of higher adiposity on cancer. Further studies are warranted to investigate whether interventions on adverse metabolic health may help to alleviate obesity-related cancer risk.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
All data will be available to approved users of the UK Biobank upon application. This study uses a reporting checklist for observational studies i.e., Strengthening the Reporting of Observational studies in Epidemiology (STROBE) guidelines (Supplementary Table 9).
References
WCRF/AICR. Diet, Nutrition, Physical Activity and Cancer: a Global Perspective A summary of the third Expert Report World Cancer Research Fund/American Institute for Cancer Research 2018. Report no.: Expert Report 2018.
Coelho M, Oliveira T, Fernandes R. Biochemistry of adipose tissue: an endocrine organ. Arch Med Sci. 2013;9:191–200.
Deng T, Lyon CJ, Bergin S, Caligiuri MA, Hsueh WA. Obesity, inflammation, and cancer. Annu Rev Pathol. 2016;11:421–49.
Park J, Morley TS, Kim M, Clegg DJ, Scherer PE. Obesity and cancer-mechanisms underlying tumour progression and recurrence. Nat Rev Endocrinol. 2014;10:455–65.
Ittmann M, Huang J, Radaelli E, Martin P, Signoretti S, Sullivan R, et al. Animal models of human prostate cancer: the consensus report of the New York meeting of the Mouse Models of Human Cancers Consortium Prostate Pathology Committee. Cancer Res. 2013;73:2718–36.
Cozzo AJ, Fuller AM, Makowski L. Contribution of adipose tissue to development of cancer. Compr Physiol. 2017;8:237–82.
Flanders WD, Augestad LB Methodological issues in observational studies of obesity and mortality. Norsk Epidemiologi. 2011;20(2):143–148.
Plotnikov D, Guggenheim JA. Mendelian randomisation and the goal of inferring causation from observational studies in the vision sciences. Ophthalmic Physiol Opt. 2019;39:11–25.
Guo Y, Warren Andersen S, Shu XO, Michailidou K, Bolla MK, Wang Q, et al. Genetically predicted body mass index and breast cancer risk: Mendelian randomization analyses of data from 145,000 women of european descent. PLoS Med. 2016;13:e1002105.
Thrift AP, Gong J, Peters U, Chang-Claude J, Rudolph A, Slattery ML, et al. Mendelian randomization study of body mass index and colorectal cancer risk. Cancer Epidemiol Biomarkers Prev. 2015;24:1024–31.
Thrift AP, Shaheen NJ, Gammon MD, Bernstein L, Reid BJ, Onstad L et al. Obesity and risk of esophageal adenocarcinoma and Barrett’s esophagus: a Mendelian randomization study. J Natl Cancer Inst. 2014;106(11):1–8.
Masuda T, Ogawa K, Kamatani Y, Murakami Y, Kimura T, Okada Y. A Mendelian randomization study identified obesity as a causal risk factor of uterine endometrial cancer in Japanese. Cancer Sci. 2020;111:4646–51.
Davies NMea. The effects of height and BMI on prostate cancer inidence and mortality: a mendelain randomization study in 20,848 cases and 20,214 controls from the PRACTICAL consortium. Cancer Causes Control. 2015;26:1603–16.
Dixon SC, Nagle CM, Thrift AP, Pharoah PD, Pearce CL, Zheng W, et al. Adult body mass index and risk of ovarian cancer by subtype: a Mendelian randomization study. Int J Epidemiol. 2016;45:884–95.
Cornish AJ, Law PJ, Timofeeva M, Palin K, Farrington SM, Palles C, et al. Modifiable pathways for colorectal cancer: a mendelian randomisation analysis. The Lancet Gastroenterol Hepatol. 2020;5:55–62.
Takahashi H, Cornish AJ, Sud A, Law PJ, Disney-Hogg L, Calvocoressi L, et al. Mendelian randomization provides support for obesity as a risk factor for meningioma. Sci Rep. 2019;9:309.
Quail DF, Dannenberg AJ. The obese adipose tissue microenvironment in cancer development and progression. Nat Rev Endocrinol. 2019;15:139–54.
Grundy SM, Brewer HB Jr., Cleeman JI, Smith SC Jr., Lenfant C, American Heart A, et al. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004;109:433–8.
NM I. Systemic correlates of white adipose tissue inflammation in early-stage breast cancer. Clin. Cancer Res. 2016;22:2283–9.
Winkler TW, Gunther F, Hollerer S, Zimmermann M, Loos RJ, Kutalik Z, et al. A joint view on genetic variants for adiposity differentiates subtypes with distinct metabolic implications. Nat Commun. 2018;9:1946.
Álvarez-Castro P, Sangiao-Alvarellos S, Brandón-Sandá I, Cordido F. Endocrine function in obesity. Endocrinología y Nutrición (English Edition). 2011;58:422–32.
Henderson BE, Feigelson HS. Hormonal carcinogenesis. Carcinogenesis. 2000;21:427–33.
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12:e1001779.
Biobank U UK Biobank Cancer Numbers Summary Report. In. UK: UK Biobank, 2020.
Wu P, Gifford A, Meng X, Li X, Campbell H, Varley T, et al. Mapping ICD-10 and ICD-10-CM Codes to Phecodes: Workflow Development and Initial Evaluation. JMIR Med Inform. 2019;7:e14325.
Locke AE, Kahali B, Berndt SI, Justice AE, Pers TH, Day FR, et al. Genetic studies of body mass index yield new insights for obesity biology. Nature. 2015;518:197–206.
Biobank TU Genotyping and quality control of UK Biobank, a large-scale, extensively phenotyped prospective resource. 2015.
GIANT. GIANT consortium data files. In. March 2019 ed, 2019.
Hyppönen E, Mulugeta A, Zhou A, Santhanakrishnan VK. A data-driven approach for studying the role of body mass in multiple diseases: a phenome-wide registry-based case-control study in the UK Biobank. The Lancet Digital Health. 2019;1:e116–e126.
Bowden J, Davey Smith G, Haycock PC, Burgess S. Consistent estimation in mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol. 2016;40:304–14.
Hartwig FP, Davey Smith G, Bowden J. Robust inference in summary data Mendelian randomization via the zero modal pleiotropy assumption. Int J Epidemiol. 2017;46:1985–98.
Burgess S, Foley CN, Allara E, Staley JR, Howson JMM. A robust and efficient method for Mendelian randomization with hundreds of genetic variants. Nat Commun. 2020;11:376.
Burgess S. Sample size and power calculations in Mendelian randomization with a single instrumental variable and a binary outcome. Int J Epidemiol. 2014;43:922–9.
Hemani G, Zheng J, Elsworth B, Wade KH, Haberland V, Baird D et al. The MR-base platform supports systematic causal inference across the human phenome. Elife 2018;7:e34408.
Amin HA, Kaewsri P, Yiorkas AM, Cooke H, Blakemore AI, Drenos F Increased adiposity is protective for breast and prostate cancer: a Mendelian randomisation study using up to 132,413 breast cancer cases and 85,907 prostate cancer cases. medRxiv. 2020:26. https://doi.org/10.1101/2020.04.02.20049031.
Davies NM, Gaunt TR, Lewis SJ, Holly J, Donovan JL, Hamdy FC, et al. The effects of height and BMI on prostate cancer incidence and mortality: a Mendelian randomization study in 20,848 cases and 20,214 controls from the PRACTICAL consortium. Cancer Causes Control. 2015;26:1603–16.
Perez-Cornago A, Appleby PN, Pischon T, Tsilidis KK, Tjonneland A, Olsen A, et al. Tall height and obesity are associated with an increased risk of aggressive prostate cancer: results from the EPIC cohort study. BMC Med. 2017;15:115.
Kabat GC, Kim MY, Lee JS, Ho GY, Going SB, Beebe-Dimmer J, et al. Metabolic obesity phenotypes and risk of breast cancer in postmenopausal women. Cancer Epidemiol Biomarkers Prev. 2017;26:1730–5.
Phillips CM. Metabolically healthy obesity across the life course: epidemiology, determinants, and implications. Ann NY Acad Sci. 2017;1391:85–100.
Painter JN, O’Mara TA, Marquart L, Webb PM, Attia J, Medland SE, et al. Genetic risk score mendelian randomization shows that obesity measured as body mass index, but not waist:hip ratio, is causal for endometrial cancer. Cancer Epidemiol Biomarkers Prev. 2016;25:1503–10.
Rosato V, Zucchetto A, Bosetti C, Dal Maso L, Montella M, Pelucchi C, et al. Metabolic syndrome and endometrial cancer risk. Ann Oncol. 2011;22:884–9.
Dallal CM, Brinton LA, Bauer DC, Buist DS, Cauley JA, Hue TF, et al. Obesity-related hormones and endometrial cancer among postmenopausal women: a nested case-control study within the B~FIT cohort. Endocr Relat Cancer. 2013;20:151–60.
Nagle CM, Marquart L, Bain CJ, O’Brien S, Lahmann PH, Quinn M, et al. Impact of weight change and weight cycling on risk of different subtypes of endometrial cancer. Eur J Cancer. 2013;49:2717–26.
Renehan AG. Bariatric surgery, weight reduction, and cancer prevention. The Lancet Oncology. 2009;10:640–1.
Went M, Cornish AJ, Law PJ, Kinnersley B, van Duin M, Weinhold N, et al. Search for multiple myeloma risk factors using Mendelian randomization. Blood Adv. 2020;4:2172–9.
Went M, Sud A, Law PJ, Johnson DC, Weinhold N, Forsti A, et al. Assessing the effect of obesity-related traits on multiple myeloma using a Mendelian randomisation approach. Blood Cancer J. 2017;7:e573.
Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. The Lancet. 2008;371:569–78.
Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K, et al. Body fatness and cancer-viewpoint of the IARC Working Group. N Engl J Med. 2016;375:794–8.
Taylor RW, Grant AM, Williams SM, Goulding A. Sex differences in regional body fat distribution from pre- to postpuberty. Obesity (Silver Spring). 2010;18:1410–6.
Perry BL, Pescosolido BA, Bucholz K, Edenberg H, Kramer J, Kuperman S, et al. Gender-specific gene-environment interaction in alcohol dependence: the impact of daily life events and GABRA2. Behav Genet. 2013;43:402–14.
Ni G, van der Werf J, Zhou X, Hypponen E, Wray NR, Lee SH. Genotype-covariate correlation and interaction disentangled by a whole-genome multivariate reaction norm model. Nat Commun. 2019;10:2239.
Martinez-Useros J, Garcia-Foncillas J. Obesity and colorectal cancer: molecular features of adipose tissue. J Transl Med. 2016;14:21.
Nagata N, Sakamoto K, Arai T, Niikura R, Shimbo T, Shinozaki M, et al. Visceral abdominal fat measured by computed tomography is associated with an increased risk of colorectal adenoma. Int J Cancer. 2014;135:2273–81.
BMJ. Reading Mendelian Randomization studies: a guide, glossary, and cheklist for clinicians. BMJ Open 2018;362:k601.
Wacholder S, Rothman N, Caporaso N. Population stratification in epidemiologic studies of common genetic variants and cancer: quantification of bias. J Natl Cancer Inst. 2000;92:1151–8.
Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 2015;44:512–25.
Alicia R Martin, M K, Yoichiro Kamatani, Yukinori Okada, Benjamin M. Neale, Mark J Daly. Clinical use of current polygenic risk scores may exacerbate health disparities. Nature Genetics. 2019;51:584–91.
Fry A, Littlejohns TJ, Sudlow C, Doherty N, Adamska L, Sprosen T, et al. Comparison of sociodemographic and health-related characteristics of UK biobank participants with those of the general population. Am J Epidemiol. 2017;186:1026–34.
Gkatzionis A, Burgess S. Contextualizing selection bias in Mendelian randomization: how bad is it likely to be? Int J Epidemiol. 2019;48:691–701.
Acknowledgements
We extend sincere thanks to the participants of the UK Biobank, who made this work possible. This study was conducted using the UK Biobank Resource under application number 20175.
Funding
This work was supported by grants from Tour de Cure (RSP-013-18/19) and National Health and Medical Research Council, Australia (GT1157281).
Author information
Authors and Affiliations
Contributions
MA wrote the original draft, conducted data management and statistical analyses. AM advised on statistical analysis. EH developed concept and design, drafted the manuscript and funded the study. All authors interpreted data, revised the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
Professor Hyppönen has received grants from the National Health and Medical Research Council, Australian Research Council, Tour de Cure, Medical Research Future Fund. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. The rest of the authors (MA, AM, SHL, V-PM and TB) declare no potential competing interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Ahmed, M., Mulugeta, A., Lee, S.H. et al. Adiposity and cancer: a Mendelian randomization analysis in the UK biobank. Int J Obes 45, 2657–2665 (2021). https://doi.org/10.1038/s41366-021-00942-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-00942-y
This article is cited by
-
The causal effects of genetically predicted alcohol consumption on endometrial cancer risk from a Mendelian randomization study
Scientific Reports (2024)
-
Causal associations of Sjögren’s syndrome with cancers: a two-sample Mendelian randomization study
Arthritis Research & Therapy (2023)
-
Exploring the causal relationship between inflammatory cytokines and migraine: a bidirectional, two-sample Mendelian randomization study
Scientific Reports (2023)
-
UK Biobank: a globally important resource for cancer research
British Journal of Cancer (2023)
-
Using machine learning to identify gene interaction networks associated with breast cancer
BMC Cancer (2022)