Abstract
The incidence of obesity has dramatically increased in recent years, and poses a public health challenge for which an effective and scalable intervention strategy is yet to be found. Our food choices are one of the primary drivers of obesity, where the overconsumption of energy from foods high in fat and sugar can be particularly problematic. Unfortunately, these same foods also tend to be highly palatable. We select foods more on their sensory properties than on any other factor, such as price, convenience, or healthfulness. Previous evidence from human sensory studies has suggested a depressed sense of taste in panelists with obesity. Evidence from animal models also demonstrates a clear deficiency in taste buds occurring with obesity, suggesting that damage to the taste system may result from an obese state. In this review only taste, as opposed to smell, will be examined. Here we seek to bring together evidence from a diverse array of human and animal studies into taste response, dietary intake, and physiology, to better understand changes in taste with obesity, with the goal of understanding whether taste may provide a novel target for intervention in the treatment of obesity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Hunter DJ, Reddy KS. Noncommunicable Diseases. N Engl J Med. 2013;369:1336–43.
Hamann A. Aktuelles zur Adipositas (mit und ohne Diabetes). Diabetologe. 2017;13:331–41.
Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014;103:137–49.
Zalesin KC, Franklin BA, Miller WM, Peterson ED, McCullough PA. Impact of obesity on cardiovascular disease. Med Clin North Am. 2011;95:919–37.
Seravalle G, Grassi G. Obesity and hypertension. Pharmacol Res. 2017;122:1–7.
Després JP, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. 2006;444:881–7.
Chen C, Ye Y, Zhang Y, Pan XF, Pan A. Weight change across adulthood in relation to all cause and cause specific mortality: prospective cohort study. BMJ. 2019;367:15584.
Kolotkin RL, Andersen JR. A systematic review of reviews: exploring the relationship between obesity, weight loss and health-related quality of life. Clin Obes. 2017;7:273–89.
Wright SM, Aronne LJ. Causes of obesity. Abdom Imaging. 2012;37:730–2.
Jeffery RW, Harnack LJ. Evidence implicating eating as a primary driver for the obesity epidemic. Diabetes. 2007;56:2673–6.
Young LR, Nestle M. Expanding portion sizes in the US marketplace: implications for nutrition counseling. J Am Diet Assoc. 2003;103:231–40.
Ford ES, Dietz WH. Trends in energy intake among adults in the United States: findings from NHANES. Am J Clin Nutr. 2013;97:848–53.
Haslam DW, James WPT. Obesity. Lancet. 2005;366:1197–209.
Rehm CD, Peñalvo JL, Afshin A, Mozaffarian D. Dietary intake among US adults. JAMA. 2016;1999–2012.
Liu J, Rehm CD, Onopa J, Mozaffarian D. Trends in diet quality among Youth in the United States. JAMA. 2020;1999–2016.
Crino M, Sacks G, Vandevijvere S, Swinburn B, Neal B. The influence on population weight gain and obesity of the macronutrient composition and energy density of the food supply. Curr Obes Rep. 2015;4:1–10.
Naughton SS, Mathai ML, Hryciw DH, McAinch AJ. Australia’s nutrition transition 1961–2009: A focus on fats. Br J Nutr. 2015;114:337–46.
Rikkers W, Lawrence D, Hafekost K, Mitrou F, Zubrick SR. Trends in sugar supply and consumption in Australia: is there an Australian Paradox? BMC Public Health. 2013;13:1–11.
Vandevijvere S, Chow CC, Hall KD, Umali E, Swinburn BA. L’accroissement de la disponibilité énergétique alimentaire comme facteur majeur de l’épidémie d’obésité: Une analyse à l’échelle internationale. Bull World Health Organ. 2015;93:446–56.
Chaput JP, Doucet É, Tremblay A. Obesity: a disease or a biological adaptation? An update. Obes Rev. 2012;13:681–91.
Hooper L, Abdelhamid A, Bunn D, Brown T, Summerbell CD, Skeaff CM. Effects of total fat intake on body weight. Cochrane Database Syst Rev. 2015. https://doi.org/10.1002/14651858.CD011834.
Morenga LTE, Mallard S, Mann J. Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies. BMJ. 2013;345.
Mozaffarian D. Dietary and policy priorities for cardiovascular disease, diabetes, and obesity. Circulation. 2016;133:187–225.
King NA, Hopkins M, Caudwell P, Stubbs RJ, Blundell JE. Beneficial effects of exercise: shifting the focus from body weight to other markers of health. Br J Sports Med. 2009;43:924–7.
Foright RM, Presby DM, Sherk VD, et al. Is regular exercise an effective strategy for weight loss maintenance? Physiol Behav. 2018;188:86–93.
Rosenbaum M, Leibel RL. Adaptive thermogenesis in humans. Int J Obes. 2010;34:S47–55.
Chen KY, Brychta RJ, Sater ZA, Cassimatis TM, Cero C, Fletcher LA, et al. Opportunities and challenges in the therapeutic activation of human energy expenditure and thermogenesis to manage obesity. J Biol Chem. 2020;295:1926–42.
Diet, nutrition and the prevention of chronic diseases. World Health Organ Tech Rep Ser. 2003;916:i–viii.
Aggarwal A, Rehm CD, Monsivais P, Drewnowski A. Importance of taste, nutrition, cost and convenience in relation to diet quality: evidence of nutrition resilience among US adults using National Health and Nutrition Examination Survey (NHANES) 2007–2010. Prev Med (Baltim). 2016;90:184–92.
Berridge KC. Measuring hedonic impact in animals and infants: microstructure of affective taste reactivity patterns. Neurosci Biobehav Rev. 2000;24:173–98.
Diószegi J, Llanaj E, Ádány R. Genetic background of taste perception, taste preferences, and its nutritional implications: a systematic review. Front Genet. 2019;10:1–22.
Nolden AA, Feeney EL. Genetic differences in taste receptors: implications for the food industry. Annu Rev Food Sci Technol. 2020;11:183–204.
De Carli L, Gambino R, Lubrano C, Rosato R, Bongiovanni D, Lanfrancoet F, et al. Impaired taste sensation in type 2 diabetic patients without chronic complications: a case–control study. J Endocrinol Invest. 2018;41:765–72.
Ahmed K, Penney N, Darzi A, Purkayastha S. Taste changes after bariatric surgery: a systematic review. Obes Surg. 2018;28:3321–32.
Cattaneo C, Gargari G, Koirala R, Laureati M, Riso P, Guglielmetti S. et al. New insights into the relationship between taste perception and oral microbiota composition. Sci Rep.2019;9:1–8.
Chang SH, Stoll CRT, Song J, Varela JE, Eagon CJ, Colditz GA. The effectiveness and risks of bariatric surgery an updated systematic review and meta-analysis 2003–2012. JAMA Surg. 2014;149:275–87.
Curioni CC, Lourenço PM. Long-term weight loss after diet and exercise: a systematic review. Int J Obes. 2005;29:1168–74.
Wu T, Gao X, Chen M, Van Dam RM. Long-term effectiveness of diet-plus-exercise interventions vs. diet-only interventions for weight loss: a meta-analysis: obesity management. Obes Rev. 2009;10:313–23.
Glanz K, Basil M, Maibach E, Goldberg J, Snyder D. Why Americans eat what they do: taste, nutrition, cost, convenience, and weight control concerns as influences on food consumption. J Am Diet Assoc. 1998;98:1118–26.
Kourouniotis S, Keast RSJ, Riddell LJ, Lacy K, Thorpe MG, Cicerale S. The importance of taste on dietary choice, behaviour and intake in a group of young adults. Appetite. 2016;103:1–7.
Zylan KD. Gender differences in the reasons given for meal termination. Appetite. 1996;26:37–44.
Beauchamp GK, Cowart BJ. Development of Sweet Taste. 1987:127–40.
Drewnowski A. Why do we like fat? J Am Diet Assoc. 1997;97(7 Suppl.):S58–62.
Lease H, Hendrie GA, Poelman AAM, Delahunty C, Cox DN. A Sensory-Diet database: a tool to characterise the sensory qualities of diets. Food Qual Prefer. 2016;49:20–32.
La Fleur SE, Van Rozen AJ, Luijendijk MCM, Groeneweg F, Adan RAH. A free-choice high-fat high-sugar diet induces changes in arcuate neuropeptide expression that support hyperphagia. Int J Obes. 2010;34:537–46.
Astrup A, Buemann B, Western P, Toubro S, Raben A, Christensen NJ. Obesity as an adaptation to a high-fat diet: evidence from a cross- sectional study. Am J Clin Nutr. 1994;59:350–5.
Warwick ZS, Schiffman SS. Sensory evaluations of fat-sucrose and fat-salt mixtures: relationship to age and weight status. Physiol Behav. 1990;48:633–6.
Blundell JE, Stubbs RJ. High and low carbohydrate and fat intakes: limits imposed by appetite and palatability and their implications for energy balance. Eur J Clin Nutr. 1999;53:s148–65.
Harnack LJ, Jeffery RW, Boutelle KN. Temporal trends in energy intake in the United States: an ecologic perspective. Am J Clin Nutr. 2000;71:1478–84.
Heitmann BL, Lissner L, Osler M. Do we eat less fat, or just report so? Int J Obes. 2000;24:435–42.
Thompson FE, Byers T. Dietary assessment resource manual. J Nutr. 1994;124(11 Suppl.):2245S–317S.
Chambers E, McGuire B, Godwin S, McDowell M, Vecchio F. Quantifying portion sizes for selected snack foods and beverages in 24- hour dietary recalls. Nutr Res. 2000;20:315–26.
Faggiano F, Vineis P, Cravanzola D, Pisani P, Xompero G, Riboli E, et al. Validation of a method for the estimation of food portion size. Epidemiology. 1992;3:379–82.
Harnack L, Steffen L, Arnett DK, Gao S, Luepker RV. Accuracy of estimation of large food portions. J Am Diet Assoc. 2004;104:804–6.
Chambers L, McCrickerd K, Yeomans MR. Optimising foods for satiety. Trends Food Sci Technol. 2015;41:149–60.
Keskitalo K, Tuorila H, Spector TD, Cherkas LF, Knaapila A, Kaprio J, et al. The Three-Factor Eating Questionnaire, body mass index, and responses to sweet and salty fatty foods: a twin study of genetic and environmental associations. Am J Clin Nutr. 2008;88:263–71.
Jayasinghe SN, Kruger R, Walsh DCI, et al. Is sweet taste perception associated with sweet food liking and intake? Nutrients. 2017;9:750.
Cattaneo C, Riso P, Laureati M, Gargari G, Pagliarini E. Exploring associations between interindividual differences in taste perception, oral microbiot a composition, and reported food intake. Nutrients. 2019;11:1167.
Han P, Keast RSJ, Roura E. Salivary leptin and TAS1R2/TAS1R3 polymorphisms are related to sweet taste sensitivity and carbohydrate intake from a buffet meal in healthy young adults. Br J Nutr. 2017;118:763–70.
Low JYQ, Lacy KE, McBride R, Keast RSJ. The association between sweet taste function, anthropometry, and dietary intake in adults. Nutrients. 2016;8:241.
Tan SY, Tucker RM. Sweet taste as a predictor of dietary intake: a systematic review. Nutrients. 2019;11:94.
Wise PM, Nattress L, Flammer LJ, Beauchamp GK. Reduced dietary intake of simple sugars alters perceived sweet taste intensity but not perceived pleasantness. Am J Clin Nutr. 2016;103:50–60.
Bertino M, Beauchamp GK, Engelman K. Long-term reduction in dietary sodium alters the taste of salt. Am J Clin Nutr. 1982;36:1134–44.
Beauchamp GK, Bertino M, Engelman K. Modification of salt taste. Ann Intern Med. 1983;98(5 Suppl.):763–9.
Noel CA, Sugrue M, Dando R. Participants with pharmacologically impaired taste function seek out more intense, higher calorie stimuli. Appetite.2017;117:74–81.
Kashima N, Kimura K, Nishitani N, Endo MY, Fukuba Y, Kashima H. Suppression of oral sweet sensations during consumption of sweet food in humans: effects on gastric emptying rate, glycemic response, appetite, food satisfaction and desire for basic tastes. Nutrients. 2020;12:1249.
Cox DN, Perry L, Moore PB, Vallis L, Mela DJ. Sensory and hedonic associations with macronutrient and energy intakes of lean and obese consumers. Int J Obes. 1999;23:403–10.
Zhou L, Stamler J, Chan Q, Van Horn L, Daviglus ML, Dyer AR, et al. Salt intake and prevalence of overweight/obesity in Japan, China, the United Kingdom, and the United States: the INTERMAP Study. Am J Clin Nutr. 2019;110:34–40.
Monteiro CA, Levy RB, Claro RM, De Castro IRR, Cannon G. Increasing consumption of ultra-processed foods and likely impact on human health: evidence from Brazil. Public Health Nutr. 2011;14:5–13.
Rust P, Ekmekcioglu C. Impact of salt intake on the pathogenesis and treatment of hypertension. Adv Exp Med Biol. 2017;956:61–84.
Bertino M, Beauchamp GK, Engelman K. Increasing dietary salt alters salt taste preference. Physiol Behav. 1986;38:203–13.
Blais CA, Pangborn RM, Borhani NO, Ferrell MF, Prineas RJ, Laing B. Effect of dietary sodium restriction on taste responses to sodium chloride: a longitudinal study. Am J Clin Nutr. 1986;44:232–43.
Bobowski N. Shifting human salty taste preference: potential opportunities and challenges in reducing dietary salt intake of Americans. Chemosens Percept. 2015;8:112–6.
Hayes JE, Sullivan BS, Duffy VB. Explaining variability in sodium intake through oral sensory phenotype, salt sensation and liking. Physiol Behav. 2010;100:369–80.
Kim GH, Lee HM. Frequent consumption of certain fast foods may be associated with an enhanced preference for salt taste. J Hum Nutr Diet. 2009;22:475–80.
Zhang Z, Zhang X. Salt taste preference, sodium intake and gastric cancer in China. Asian Pacific J Cancer Prev. 2011;12:1207–10.
Kastorini CM, Milionis HJ, Esposito K, Giugliano D, Goudevenos JA, Panagiotakos DB. The effect of mediterranean diet on metabolic syndrome and its components: a meta-analysis of 50 studies and 534,906 individuals. J Am Coll Cardiol. 2011;57:1299–313.
Veček NN, Mucalo L, Dragun R, Miličević T, Pribisalić A, Patarčićet I, et al. The association between salt taste perception, mediterranean diet and metabolic syndrome: A cross-sectional study. Nutrients. 2020;12:1164.
Noel CA, Finlayson G, Dando R. Prolonged exposure to monosodium glutamate in healthy young adults decreases perceived umami taste and diminishes appetite for savory foods. J Nutr. 2018;148:980–8.
Newman LP, Bolhuis DP, Torres SJ, Keast RSJ. Dietary fat restriction increases fat taste sensitivity in people with obesity. Obesity. 2016;24:328–34.
Halton TL, Hu FB. The effects of high protein diets on thermogenesis, satiety and weight loss: a critical review. J Am Coll Nutr. 2004;23:373–85.
Luscombe-Marsh ND, Smeets AJPG, Westerterp-Plantenga MS. Taste sensitivity for monosodium glutamate and an increased liking of dietary protein. Br J Nutr. 2008;99:904–8.
Kubota M, Toda C, Nagai-Moriyama A. Relationship between umami taste acuity with sweet or bitter taste acuity and food selection in Japanese women university students. Asia Pac J Clin Nutr. 2018;27:107–12.
Nelson G, Chandrashekar J, Hoon MA, et al. An amino-acid taste receptor. Nature. 2002;416:199–202.
Shahbandi A, Choo E, Dando R. Receptor regulation in taste: can diet influence how we perceive foods? J Multidiscip J. 2018;1:106–15.
Westerterp KR. Perception, passive overfeeding and energy metabolism. Physiol Behav. 2006;89:62–5.
Heinze JM, Costanzo A, Baselier I, Fritsche A, Frank-Podlech S, Keast R. Detection thresholds for four different fatty stimuli are associated with increased dietary intake of processed high-caloric food. Appetite. 2018;123:7–13.
Proserpio C, Laureati M, Bertoli S, Battezzati A, Pagliarini E. Determinants of obesity in Italian adults: the role of taste sensitivity, food liking, and food neophobia. Chem Senses. 2016;41:169–76.
Stewart JE, Feinle-Bisset C, Golding M, Delahunty C, Clifton PM, Keast RSJ. Oral sensitivity to fatty acids, food consumption and BMI in human subjects. Br J Nutr. 2010;104:145–52.
Stewart JE, Newman LP, Keast RSJ. Oral sensitivity to oleic acid is associated with fat intake and body mass index. Clin Nutr. 2011;30:838–44.
Bartoshuk LM, Duffy VB, Hayes JE, Moskowitz HR, Snyder DJ. Psychophysics of sweet and fat perception in obesity: problems, solutions and new perspectives. Philos Trans R Soc B Biol Sci. 2006;361:1137–48.
Ettinger L, Duizer L, Caldwell T. Body fat, sweetness sensitivity, and preference: determining the relationship. Can J Diet Pract Res. 2012;73:45–8.
Overberg J, Hummel T, Krude H, Wiegand S. Differences in taste sensitivity between obese and non-obese children and adolescents. Arch Dis Child. 2012;97:1048–52.
Pepino MY, Finkbeiner S, Beauchamp GK, Mennella JA. Obese women have lower monosodium glutamate taste sensitivity and prefer higher concentrations than do normal-weight women. Obesity. 2010;18:959–65.
Vignini A, Borroni F, Sabbatinelli J, Pugnaloni S, Alia S, Taus M, et al. General decrease of taste sensitivity is related to increase of BMI: a simple method to monitor eating behavior. Dis Markers. 2019;2019:1–8.
Park DC, Yeo JH, Ryu IY, Kim SH, Jung J, Yeo SG. Differences in taste detection thresholds between normal-weight and obese young adults. Acta Otolaryngol. 2015;135:478–83.
Coltell O, Sorlí JV, Asensio EM, Fernández-Carrión R, Barragán R, Ortega-Azorín C, et al. Association between taste perception and adiposity in overweight or obese older subjects with metabolic syndrome and identification of novel taste-related genes. Am J Clin Nutr. 2019;109:1709–23.
Stewart JE, Keast RSJ. Recent fat intake modulates fat taste sensitivity in lean and overweight subjects. Int J Obes. 2012;36:834–42.
He K, Zhao L, Daviglus ML, Dyer AR, Van Horn L, Garsidee D, et al. Association of monosodium glutamate intake with overweight in Chinese adults: the INTERMAP study. Obesity. 2008;16:1875–80.
Feeney EL, Leacy L, O‘kelly M, Leacy N, Phelan A, Crowley L, et al. Sweet and umami taste perception differs with habitual exercise in males. Nutrients. 2019;11:155.
Liu D, Archer N, Duesing K, Hannan G, Keast R. Mechanism of fat taste perception: association with diet and obesity. Prog Lipid Res. 2016;63:41–9.
Pepino MY, Love-Gregory L, Klein S, Abumrad NA. The fatty acid translocase gene CD36 and lingual lipase influence oral sensitivity to fat in obese subjects. J Lipid Res. 2012;53:561–6.
Mrizak I, Šerý O, Plesnik J, Arfa A, Fekih M, Bouslemae A, et al. The A allele of cluster of differentiation 36 (CD36) SNP 1761667 associates with decreased lipid taste perception in obese Tunisian women. Br J Nutr. 2015;113:1330–7.
Sayed A, Šerý O, Plesnik J, Daoudi H, Rouabah A, Rouabahe L, et al. CD36 AA genotype is associated with decreased lipid taste perception in young obese, but not lean, children. Int J Obes. 2015;39:920–4.
Karmous I, Plesník J, Khan AS, Šerý O, Abid A, Mankai A, et al. Orosensory detection of bitter in fat-taster healthy and obese participants: genetic polymorphism of CD36 and TAS2R38. Clin Nutr. 2018;37:313–20.
Tucker RM, Nuessle TM, Garneau NL, Smutzer G, Mattes RD. No difference in perceived intensity of linoleic acid in the oral cavity between obese and nonobese individuals. Chem Senses. 2015;40:557–63.
Costanzo A, Orellana L, Nowson C, Duesing K, Keast R. Fat taste sensitivity is associated with short-term and habitual fat intake. Nutrients. 2017;9:781.
Bolhuis DP, Costanzo A, Newman LP, Keast RSJ. Salt promotes passive overconsumption of dietary fat in humans. J Nutr. 2016;146:838–45.
Hardikar S, Höchenberger R, Villringer A, Ohla K. Higher sensitivity to sweet and salty taste in obese compared to lean individuals. Appetite. 2017;111:158–65.
Drewnowski A, Kurth CL, Rahaim JE. Taste preferences in human obesity: environmental and familial factors. Am J Clin Nutr. 1991;54:635–41.
Enns MP, Van Itallie TB, Grinker JA. Contributions of age, sex and degree of fatness on preferences and magnitude estimations for sucrose in humans. Physiol Behav. 1979;22:999–1003.
Frijters JE, Rasmussen-Conrad EL. Sensory discrimination, intensity perception, and affective judgment of sucrose-sweetness in the overweight. J Gen Psychol. 1982;107(2 d Half):233–47.
Rodin J, Moskowitz HR, Bray GA. Relationship between obesity, weight loss, and taste responsiveness. Physiol Behav. 1976;17:591–7.
Thompson DA, Moskowitz HR, Campbell RG. Taste and olfaction in human obesity. Physiol Behav. 1977;19:335–7.
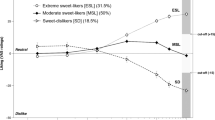
Noel CA, Cassano PA, Dando R. College-aged males experience attenuated sweet and salty taste with modest weight gain. J Nutr. 2017;147:1885–91.
Kalveramn L, Gohlisch J, Brauchmann J, Overberg J, Kühnen P, Wiegand S. Lifestyle Intervention: a longitudinal observational study in pediatric patients with obesity. Child Obes. 2021;17:136–43.
Singh S. Exploring the associations between sweet taste perception and habitual dietary intake in New Zealand European women. Massey University. Published online 2018.
Miyaki T, Imada T, Shuzhen Hao S, Kimura E. Monosodium l-glutamate in soup reduces subsequent energy intake from high-fat savoury food in overweight and obese women. Br J Nutr. 2016;115:176–84.
Masic U, Yeomans MR. Does monosodium glutamate interact with macronutrient composition to influence subsequent appetite? Physiol Behav. 2013;116–7:23–9.
Anderson GH, Fabek H, Akilen R, Chatterjee D, Kubant R. Acute effects of monosodium glutamate addition to whey protein on appetite, food intake, blood glucose, insulin and gut hormones in healthy young men. Appetite. 2018;120:92–9.
Ventura AK, Beauchamp GK, Mennella JA. Infant regulation of intake: the effect of free glutamate content in infant formulas. Am J Clin Nutr. 2012;95:875–81.
Masic U, Yeomans MR. Umami flavor enhances appetite but also increases satiety. Am J Clin Nutr. 2014;100:532–8.
He K, Du S, Xun P, Sharma S, Wang H, Zhai F, et al. Consumption of monosodium glutamate in relation to incidence of overweight in Chinese adults: China Health and Nutrition Survey (CHNS). Am J Clin Nutr. 2011;93:1328–36.
Shi Z, Luscombe-Marsh ND, Wittert GA, Yuan B, Dai Y, Pan X, et al. Monosodium glutamate is not associated with obesity or a greater prevalence of weight gain over 5 years: findings from the Jiangsu Nutrition Study of Chinese adults. Br J Nutr. 2010;104:457–63.
Samuels A. Monosodium glutamate is not associated with obesity or a greater prevalence of weight gain over 5 years: findings from the Jiangsu Nutrition Study of Chinese adults—Comments by Samuels. Br J Nutr. 2010;104:1729.
He K, Daviglus ML, Stamler J. Response to “evidence that MSG does not induce obesity”. Obesity. 2009;17:630–1.
Deglaire A, Méjean C, Castetbon K, Kesse-Guyot E, Hercberg S, Schlich P. Associations between weight status and liking scores for sweet, salt and fat according to the gender in adults (The Nutrinet-Santé study). Eur J Clin Nutr. 2015;69:40–6.
Donaldson LF, Bennett L, Baic S, Melichar JK. Taste and weight: is there a link? Am J Clin Nutr. 2009;90:800S–3S.
Pasquet P, Frelut ML, Simmen B, Hladik CM, Monneuse MO. Taste perception in massively obese and in non-obese adolescents. Int J Pediatr Obes. 2007;2:242–8.
Tucker RM, Edlinger C, Craig BA, Mattes RD. Associations between BMI and fat taste sensitivity in humans. Chem Senses. 2014;39:349–57.
Tucker RM, Mattes RD. Influences of repeated testing on nonesterified fatty acid taste. Chem Senses. 2013;38:325–32.
Keast RSJ, Azzopardi KM, Newman LP, Haryono RY. Impaired oral fatty acid chemoreception is associated with acute excess energy consumption. Appetite. 2014;80:1–6.
Costanzo A, Russell CG, Lewin S, Keast R. A fatty acid mouth rinse decreases self-reported hunger and increases self-reported fullness in healthy Australian adults: a randomized cross-over trial. Nutrients. 2020;12:678.
Stewart JE, Seimon RV, Otto B, Keast RSJ, Clifton PM, Feinle-Bisset C. Marked differences in gustatory and gastrointestinal sensitivity to oleic acid between lean and obese men. Am J Clin Nutr. 2011;93:703–11.
Liu D, Costanzo A, Evans MDM, Archer NS, Nowson C, Duesing K, et al. Expression of the candidate fat taste receptors in human fungiform papillae and the association with fat taste function. Br J Nutr. 2018;120:64–73.
Kaufman A, Choo E, Koh A, Dando R. Inflammation arising from obesity reduces taste bud abundance and inhibits renewal. PLoS Biol. 2018;16:e2001959.
Kaufman A, Kim J, Noel C, Dando R. Taste loss with obesity in mice and men. Int J Obes. 2020;44:739–43.
Ahart Z, Martin L, Kemp B, Banik DD, Roberts SGE, Torregrossa AM, et al. Differential effects of diet and weight on taste responses in diet-induced obese mice. Obesity. 2019;28:284–92.
Chen K, Yan J, Suo Y, Li J, Wang Q, Lv B. Nutritional status alters saccharin intake and sweet receptor mRNA expression in rat taste buds. Brain Res. 2010;1325:53–62.
Chevrot M, Bernard A, Ancel D, Buttet M, Martin C, Abdoul-Azize S, et al. Obesity alters the gustatory perception of lipids in the mouse: plausible involvement of lingual CD36. J Lipid Res. 2013;54:2485–94.
Maliphol AB, Garth DJ, Medler KF. Diet-induced obesity reduces the responsiveness of the peripheral taste receptor cells. PLoS ONE. 2013;8:e79403.
Zhang XJ, Zhou LH, Ban X, Liu DX, Jiang W, Liu XM. Decreased expression of CD36 in circumvallate taste buds of high-fat diet induced obese rats. Acta Histochem. 2011;113:663–7.
Ozdener MH, Subramaniam S, Sundaresan S, Sery O, Hashimoto T, Asakawa Y, et al. CD36- and GPR120-mediated Ca2+. signaling in human taste bud cells mediates differential responses to fatty acids and is altered in obese mice. Gastroenterology. 2014;146:995–1005.
Fukuwatari T, Kawada T, Tsuruta M, Hiraoka T, Iwanaga T, Sugimoto E, et al. Expression of the putative membrane fatty acid transporter (FAT) in taste buds of the circumvallate papillae in rats. FEBS Lett. 1997;414:461–4.
Laugerette F, Passilly-Degrace P, Patris B, Niot I, Febbraio M, Montmayeur JP, et al. CD36 involvement in orosensory detection of dietary lipids, spontaneous fat preference, and digestive secretions. J Clin Invest. 2005;115:3177–84.
Bernard A, Ancel D, Neyrinck AM, Dastugue A, Bindels LB, Delzenne NM, et al. A preventive prebiotic supplementation improves the sweet taste perception in diet-induced obese mice. Nutrients. 2019;11:549.
Choo E, Wong L, Chau P, Bushnell J, Dando R. Offspring of obese mice display enhanced intake and sensitivity for palatable stimuli, with altered expression of taste signaling elements. Sci Reps Press. 2020;10:1–11.
Liu F, Thirumangalathu S, Gallant NM, Yang SH, Stoick-Cooper CL, Reddy ST, et al. Wnt-β-catenin signaling initiates taste papilla development. Nat Genet. 2007;39:106–12.
Iwatsuki K, Liu HX, Gründer A, Singer MA, Lane TF, Grosschedl R, et al. Wnt signaling interacts with Shh to regulate taste papilla development. Proc Natl Acad Sci U.S.A. 2007;104:2253–8.
May CE, Vaziri A, Lin YQ, Grushko O, Khabiri M, Wang QP, et al. High dietary sugar reshapes sweet taste to promote feeding behavior in drosophila melanogaster. Cell Rep. 2019;27:1675–.e7.
Archer N, Shaw J, Cochet-Broch M, Bunch R, Poelman A, Barendse W, et al. Obesity is associated with altered gene expression in human tastebuds. Int J Obes. 2019;43:1475–84.
Hall JMH, Bell ML, Finger TE. Disruption of Sonic hedgehog signaling alters growth and patterning of lingual taste papillae. Dev Biol. 2003;255:263–77.
Mameli C, Cattaneo C, Panelli S, Comandatore F, Sangiorgio A, Bedogni G, et al. Taste perception and oral microbiota are associated with obesity in children and adolescents. PLoS ONE. 2019;14:e0221656.
Miller IJ, Reedy FE. Quantification of fungiform papillae and taste pores in living human subjects. Chem Senses. 1990;15:281–94.
Johnson PM, Kenny PJ. Dopamine D2 receptors in addiction-like reward dysfunction and compulsive eating in obese rats. Nat Neurosci. 2010;13:635–41. https://doi.org/10.1038/nn.2519.
Volkow ND, Wang GJ, Baler RD. Reward, dopamine and the control of food intake: implications for obesity. Trends Cogn Sci. 2011;15:37–46.
Weiss MS, Hajnal A, Czaja K, Di Lorenzo PM. Taste responses in the nucleus of the solitary tract of awake obese rats are blunted compared with those in lean rats. Front Integr Neurosci. 2019;13:35.
Frank GKW, Reynolds JR, Shott ME, Jappe L, Yang TT, Tregellas JR, et al. Anorexia nervosa and obesity are associated with opposite brain reward response. Neuropsychopharmacology. 2012;37:2031–46.
Green E, Jacobson A, Haase L, Murphy C. Reduced nucleus accumbens and caudate nucleus activation to a pleasant taste is associated with obesity in older adults. Brain Res. 2011;1386:109–17.
Hardikar S, Wallroth R, Villringer A, Ohla K. Shorter-lived neural taste representations in obese compared to lean individuals. Sci Rep. 2018;8:1–10.
Chao DHM, Argmann C, Van Eijk M, Boot RG, Ottenhoff R, Van Roomen C, et al. Impact of obesity on taste receptor expression in extra-oral tissues: Emphasis on hypothalamus and brainstem. Sci Rep. 2016;6:1–14.
Rohde K, Schamarek I, Blüher M. Consequences of obesity on the sense of taste: taste buds as treatment targets? Diabetes Metab J. 2020;44:509–28.
Goodman J, Dando R. To detect and reject: parallel roles for taste and immunity. Current Nutriton Reports. 2021;10:137–45.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Harnischfeger, F., Dando, R. Obesity-induced taste dysfunction, and its implications for dietary intake. Int J Obes 45, 1644–1655 (2021). https://doi.org/10.1038/s41366-021-00855-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-00855-w