Abstract
Background
Fetal exposure to maternal excess adiposity and hyperglycemia is risk factors for childhood adverse metabolic outcomes. Using data from a prospective pre-birth cohort, we aimed to further understand the prenatal determinants of fetal metabolic programming based on analyses of maternal adiposity and glycemic traits across pregnancy with childhood metabolomic profiles.
Methods
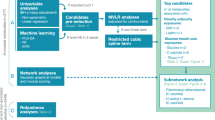
This study included 330 mother–child pairs from the Gen3G cohort with information on maternal adiposity and glycemic markers at 5–16 (visit 1) and 24–30 (visit 2) weeks of pregnancy. At mid-childhood (4.8–7.2 years old), we collected fasting plasma and measured 1116 metabolites using an untargeted approach. We constructed networks of interconnected metabolites using a weighted-correlation network analysis algorithm. We estimated Spearman’s partial correlation coefficients of maternal adiposity and glycemic traits across pregnancy with metabolite networks and individual metabolites, adjusting for maternal age, gravidity, race/ethnicity, history of smoking, and child’s sex and age at blood collection for metabolite measurement.
Results
We identified a network of 16 metabolites, primarily glycero-3-phosphoethanolamines (GPE) at mid-childhood that showed consistent negative correlations with maternal body mass index, waist circumference, and body-fat percentage at visits 1 and 2 (ρadjusted = −0.14 to −0.21) and post-challenge glucose levels at visit 2 (ρadjusted = −0.10 to −0.13), while positive correlations with Matsuda index (ρadjusted = 0.13). Within this identified network, 1-palmitoyl-2-decosahexaenoyl-GPE and 1-stearoyl-2-decosahexaenoyl-GPE appeared to be driving the associations. In addition, a network of 89 metabolites, primarily phosphatidylcholines, plasmalogens, sphingomyelins, and ceramides showed consistent negative correlations with insulin at visit 1 and post-challenge glucose at visit 2, while positive correlation with adiponectin at visit 2.
Conclusions
Prenatal exposure to maternal higher adiposity and hyperglycemic traits and lower insulin sensitivity markers were associated with a unique metabolomic pattern characterized by low serum phospho- and sphingolipids in mid-childhood.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Barker DJ. The origins of the developmental origins theory. J Intern Med. 2007;261:412–7.
Marsit CJ. Placental epigenetics in children’s environmental health. Semin Reprod Med. 2016;34:36–41.
Hivert MF, Perng W, Watkins SM, Newgard CS, Kenny LC, Kristal BS, et al. Metabolomics in the developmental origins of obesity and its cardiometabolic consequences. J Dev Orig Health Dis. 2015;6(2):65–78.
Gautier JF, Wilson C, Weyer C, Mott D, Knowler WC, Cavaghan M, et al. Low acute insulin secretory responses in adult offspring of people with early onset type 2 diabetes. Diabetes. 2001;50:1828–33.
Krishnaveni GV, Veena SR, Hill JC, Kehoe S, Karat SC, Fall CH. Intrauterine exposure to maternal diabetes is associated with higher adiposity and insulin resistance and clustering of cardiovascular risk markers in Indian children. Diabetes Care. 2010;33:402–4.
Sauder KA, Hockett CW, Ringham BM, Glueck DH, Dabelea D. Fetal overnutrition and offspring insulin resistance and beta-cell function: the Exploring Perinatal Outcomes among Children (EPOCH) study. Diabetic Med J Br Diabet Assoc. 2017;34:1392–9.
West NA, Crume TL, Maligie MA, Dabelea D. Cardiovascular risk factors in children exposed to maternal diabetes in utero. Diabetologia. 2011;54:504–7.
Lowe WL Jr., Scholtens DM, Lowe LP, Kuang A, Nodzenski M, Talbot O, et al. Association of gestational diabetes with maternal disorders of glucose metabolism and childhood adiposity. JAMA. 2018;320:1005–16.
Wright CS, Rifas-Shiman SL, Rich-Edwards JW, Taveras EM, Gillman MW, Oken E. Intrauterine exposure to gestational diabetes, child adiposity, and blood pressure. Am J Hypertens. 2009;22:215–20.
Perng W, Gillman MW, Fleisch AF, Michalek RD, Watkins SM, Isganaitis E, et al. Metabolomic profiles and childhood obesity. Obesity. 2014;22:2570–8.
Bunt JC, Tataranni PA, Salbe AD. Intrauterine exposure to diabetes is a determinant of hemoglobin A(1)c and systolic blood pressure in pima Indian children. J Clin Endocrinol Metab. 2005;90:3225–9.
Razquin C, Liang L, Toledo E, Clish CB, Ruiz-Canela M, Zheng Y, et al. Plasma lipidome patterns associated with cardiovascular risk in the PREDIMED trial: a case-cohort study. Int J Cardiol. 2018;253:126–32.
Rhee EP, Cheng S, Larson MG, Walford GA, Lewis GD, McCabe E, et al. Lipid profiling identifies a triacylglycerol signature of insulin resistance and improves diabetes prediction in humans. J Clin Invest. 2011;121:1402–11.
Alshehry ZH, Mundra PA, Barlow CK, Mellett NA, Wong G, McConville MJ, et al. Plasma lipidomic profiles improve on traditional risk factors for the prediction of cardiovascular events in type 2 diabetes mellitus. Circulation. 2016;134:1637–50.
Guillemette L, Allard C, Lacroix M, Patenaude J, Battista MC, Doyon M, et al. Genetics of glucose regulation in gestation and growth (Gen3G): a prospective prebirth cohort of mother-child pairs in Sherbrooke, Canada. BMJ Open. 2016;6:e010031.
Nunez C, Gallagher D, Visser M, Pi-Sunyer FX, Wang Z, Heymsfield SB. Bioimpedance analysis: evaluation of leg-to-leg system based on pressure contact footpad electrodes. Med Sci Sports Exerc. 1997;29:524–31.
Matsuda M, DeFronzo RA. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care. 1999;22:1462–70.
Kirwan JP, Huston-Presley L, Kalhan SC, Catalano PM. Clinically useful estimates of insulin sensitivity during pregnancy: validation studies in women with normal glucose tolerance and gestational diabetes mellitus. Diabetes Care. 2001;24:1602–7.
Zaghlool SB, Mook-Kanamori DO, Kader S, Stephan N, Halama A, Engelke R, et al. Deep molecular phenotypes link complex disorders and physiological insult to CpG methylation. Human Mol Genet. 2018;27:1106–21.
Evans AM, DeHaven CD, Barrett T, Mitchell M, Milgram E. Integrated, nontargeted ultrahigh performance liquid chromatography/electrospray ionization tandem mass spectrometry platform for the identification and relative quantification of the small-molecule complement of biological systems. Anal Chem. 2009;81:6656–67.
Dehaven CD, Evans AM, Dai H, Lawton KA. Organization of GC/MS and LC/MS metabolomics data into chemical libraries. J Cheminform. 2010;2:9.
Hagenbeek FA, Pool R, van Dongen J, Draisma HHM, Jan Hottenga J, Willemsen G, et al. Heritability estimates for 361 blood metabolites across 40 genome-wide association studies. Nat Commun. 2020;11:39.
Wei R, Wang J, Su M, Jia E, Chen S, Chen T, et al. Missing value imputation approach for mass spectrometry-based metabolomics data. Sci Rep. 2018;8:663.
Yang J, Zhao X, Lu X, Lin X, Xu G. A data preprocessing strategy for metabolomics to reduce the mask effect in data analysis. Front Mol Biosci. 2015;2:4.
Perng W, Rifas-Shiman SL, Sordillo J, Hivert M-F, Oken E. Metabolomic profiles of overweight/obesity phenotypes during adolescence: a cross-sectional study in project viva. Obesity. 2020;28:379–87.
Langfelder P, Horvath S. WGCNA: an R package for weighted correlation network analysis. BMC Bioinform. 2008;9:559.
Bareinboim E, Barbosa VC. Descents and nodal load in scale-free networks. Phys Rev E Stat Nonlin Soft Matter Phys. 2008;77:046111.
Cline MS, Smoot M, Cerami E, Kuchinsky A, Landys N, Workman C, et al. Integration of biological networks and gene expression data using Cytoscape. Nat Protoc. 2007;2:2366.
Catalano PM, Presley L, Minium J, Hauguel-de Mouzon S. Fetuses of obese mothers develop insulin resistance in utero. Diabetes Care. 2009;32:1076–80.
Catalano PM, Thomas A, Huston-Presley L, Amini SB. Increased fetal adiposity: a very sensitive marker of abnormal in utero development. Am J Obstet Gynecol. 2003;189:1698–704.
Lowe WL Jr., Bain JR, Nodzenski M, Reisetter AC, Muehlbauer MJ, Stevens RD, et al. Maternal BMI and glycemia impact the fetal metabolome. Diabetes Care. 2017;40:902–10.
Kim S, Chen J, Cheng T, Gindulyte A, He J, He S, et al. PubChem 2019 update: improved access to chemical data. Nucleic Acids Res. 2019;47:D1102–9.
Wassall SR, Leng X, Canner SW, Pennington R, Kinnun JJ, Cavazos A, et al. Docosahexaenoic acid regulates the formation of lipid rafts: a unified view from experiment and simulation. Biochimica et Biophysica Acta (BBA) Biomembr. 2018;1860:1985–93.
Avallone R, Vitale G, Bertolotti M. Omega 3 fatty acids and neurodegenerative diseases: new evidence in clinical trials. Int J Mol Sci. 2019;20:4256.
Gianfrancesco MA, Paquot N, Piette J, Legrand-Poels S. Lipid bilayer stress in obesity-linked inflammatory and metabolic disorders. Biochem Pharmacol. 2018;153:168–83.
Wishart DS, Feunang YD, Marcu A, Guo AC, Liang K, Vazquez-Fresno R, et al. HMDB 4.0: the human metabolome database for 2018. Nucleic Acids Res. 2018;46:D608–17.
National Center for Biotechnology Information. PubChem Database. 2020. CID=53478105. 2020.
Palmer ND, Okut H, Hsu FC, Ng MCY, Chen YI, Goodarzi MO, et al. Metabolomics identifies distinctive metabolite signatures for measures of glucose homeostasis: the Insulin Resistance Atherosclerosis Family Study (IRAS-FS). J Clin Endocrinol Metab. 2018;103:1877–88.
Wahl S, Holzapfel C, Yu Z, Michaela B, Kondofersky I, Christiane F, et al. Metabolomics reveals determinants of weight loss during lifestyle intervention in obese children. Metabolomics. 2013;9:1157–67.
Viner RM, Ross D, Hardy R, Kuh D, Power C, Johnson A, et al. Life course epidemiology: recognising the importance of adolescence. J Epidemiol Community Health. 2015;69:719–20.
Pirhaji L, Milani P, Leidl M, Curran T, Avila-Pacheco J, Clish CB, et al. Revealing disease-associated pathways by network integration of untargeted metabolomics. Nat Methods. 2016;13:770–6.
Molenaar PCM. A manifesto on psychology as idiographic science: bringing the person back into scientific psychology, this time forever. Meas: Interdiscip Res Perspect. 2004;2:201–18.
Lof M, Forsum E. Evaluation of bioimpedance spectroscopy for measurements of body water distribution in healthy women before, during, and after pregnancy. J Appl Physiol (1985). 2004;96:967–73.
Ceyhan ST, Safer U, Cintosun U. Bioelectric impedance analysis in pregnant women. American J Obstet Gynecol. 2015;212:120.
Acknowledgements
This work was supported by American Diabetes Association accelerator award #1–15-ACE-26 (M-FH), Fonds de recherche du Québec en santé (FRSQ) #20697 (M-FH); Canadian Institute of Health Research #MOP 115071 (M-FH), and Diabète Québec Grants (PP and LB). LB is a senior research scholar from the FRSQ. LB, M-FH, and PP are members of the FRSQ-funded CRCHUS.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Rahman, M.L., Doyon, M., Arguin, M. et al. A prospective study of maternal adiposity and glycemic traits across pregnancy and mid-childhood metabolomic profiles. Int J Obes 45, 860–869 (2021). https://doi.org/10.1038/s41366-021-00750-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-021-00750-4