Abstract
Background
The prevalence of children with elevated weight or obesity is concerning for public health due to associated comorbidities. This study investigates associations between parental adiposity, physical activity (PA), fruit and vegetable consumption, and child adiposity and moderation by both child and parent gender.
Methods
Cross-sectional nationally representative data from the New Zealand Health Survey were pooled for the years 2013/14–2016/17. Parent and child surveys were matched resulting in 13,039 child (2–14 years) and parent (15–70 years) dyads. Parent and child, height (cm), weight (kg) and waist circumference (WC) were measured objectively. Height and weight were used to calculate BMI. Linear regression, accounting for clustered samples (b [95% CI]) investigated associations between parental characteristics and child BMI z-score and WC. Interactions and stratification were used to investigate effect moderation by parent gender, child gender, and parent adiposity.
Results
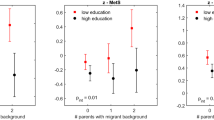
Parental PA and fruit and vegetable consumption were unrelated to child adiposity. Overall, higher parent BMI was related to a higher child BMI z-score (b = 0.047 [0.042, 0.052]) and higher parental WC was related to a higher child WC (0.15 [0.12, 0.17]). A three-way interaction revealed no moderation by parent gender, child gender, and parent BMI for child BMI z-score ((b = 0.005 [−0.017, 0.027], p = 0.318). However, a three-way interaction revealed moderation by parent gender, child gender, and parent WC for child WC (b = 0.13 [0.05, 0.22]). The slightly stronger associations were seen between father–son WC (b = 0.20 [0.15, 0.24]) and mother–daughter WC (b = 0.19 [0.15, 0.22]).
Conclusions
The findings are highly relevant for those wishing to understand the complex relationships between child-parent obesity factors. Findings suggest that family environments should be a key target for obesity intervention efforts and show how future public health interventions should be differentiated to account for both maternal and paternal influences on child adiposity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Abarca-Gómez L, Abdeen ZA, Hamid ZA, Abu-Rmeileh NM, Acosta-Cazares B, Acuin C, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128 million children, adolescents, and adults. Lancet. 2017;390:2627–42.
Bauman A, Rutter H, Baur L. Too little, too slowly: international perspectives on childhood obesity. Public Health Res Pract. 2019;29:1–5. https://pubmed.ncbi.nlm.nih.gov/30972402/.
Ananthapavan J, Sacks G, Moodie M, Carter R. Economics of obesity—learning from the past to contribute to a better future. Int J Environ Res Public Health. 2014;11:4007.
Ministry of Health. New Zealand Health Survey 2016/17 Annual Data Explorer Wellington: Minsitry of Health; 2018. https://minhealthnz.shinyapps.io/nz-health-survey-2016-17-annual-data-explorer/_w_c13033de/#!/explore-indicators.
Ministry of Health. Childhood obesity plan. Wellington: Ministry of Health; 2018.
Abdullah A, Peeters A, de Courten M, Stoelwinder J. The magnitude of association between overweight and obesity and the risk of diabetes: a meta-analysis of prospective cohort studies. Diabetes Res Clin Pract. 2010;89:309.
Apovian C. The clinical and economic consequences of obesity. Am J Manag Care. 2013;19:219–28.
Brytek-Matera A. Exploring the factors related to body image dissatisfaction in the context of obesity. Arch Psychiatry Psychother. 2011;13:63.
Cote A, Harris K, Panagiotopoulos C, Sandor G, Devlin A. Childhood obesity and cardiovascular dysfunction. J Am College Cardiol. 2013;3:3011–8.
Dee A, Kearns K, O’Neill C, Sharp L, Staines A, O’Dwyer V, et al. The direct and indirect costs of both overweight and obesity: a systematic review. BMC Res Notes. 2014;7:242.
Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–858. https://doi.org/10.1016/S0140-6736(18)32279-7.
Egger G, Swinburn B. Ecological model and obesity. Br Med J. 1997;515:477–80.
Hobbs M, Tomintz M, McCarthy J, Marek L, Vannier C, Campbell M, et al. Obesity risk in women of childbearing age in New Zealand: a nationally representative cross-sectional study. Int J Public Health. 2019;64:625–35.
Green MA, Radley D, Lomax N, Morris MA, Griffiths C. Is adolescent body mass index and waist circumference associated with the food environments surrounding schools and homes? A longitudinal analysis. BMC Public Health. 2018;18:482.
Whitaker KL, Jarvis MJ, Beeken RJ, Boniface D, Wardle J. Comparing maternal and paternal intergenerational transmission of obesity risk in a large population-based sample. Am J Clin Nutr. 2010;91:1560–7.
Huffman FG, Kanikireddy S, Patel M. Parenthood—a contributing factor to childhood obesity. Int J Environ Res Public Health. 2010;7:2800–10.
Jones LR, Steer CD, Rogers IS, Emmett PM. Influences on child fruit and vegetable intake: sociodemographic, parental and child factors in a longitudinal cohort study. Public Health Nutr. 2010;13:1122–30.
Pearson N, Biddle SJ, Gorely T. Family correlates of fruit and vegetable consumption in children and adolescents: a systematic review. Public Health Nutr. 2009;12:267–83.
Touyz LM, Wakefield CE, Grech AM, Quinn VF, Costa DSJ, Zhang FF, et al. Parent-targeted home-based interventions for increasing fruit and vegetable intake in children: a systematic review and meta-analysis. Nutr Rev. 2018;76:154–73.
Sterdt E, Liersch S, Walter U. Correlates of physical activity of children and adolescents: a systematic review of reviews. Health Educ J. 2013;73:72–89.
Fuemmeler BF, Anderson CB, Masse LC. Parent-child relationship of directly measured physical activity. Int J Behav Nutr Phys Act. 2011;8:17.
Jacobi D, Caille A, Borys J-M, Lommez A, Couet C, Charles M-A, et al. Parent-offspring correlations in pedometer-assessed physical activity. PloS ONE. 2011;6:e29195.
Gebremariam MK, Altenburg TM, Lakerveld J, Andersen LF, Stronks K, Chinapaw MJ, et al. Associations between socioeconomic position and correlates of sedentary behaviour among youth: a systematic review. Obes Rev. 2015;16:988–1000.
Neshteruk CD, Nezami BT, Nino-Tapias G, Davison KK, Ward DS. The influence of fathers on children’s physical activity: a review of the literature from 2009 to 2015. Prev Med. 2017;102:12–9.
Barnes AT, Plotnikoff RC, Collins CE, Morgan PJ. Maternal correlates of objectively measured physical activity in girls. Matern Child Health J. 2015;19:2348–57.
Lee CY, Ledoux TA, Johnston CA, Ayala GX, O’Connor DP. Association of parental body mass index (BMI) with child’s health behaviors and child’s BMI depend on child’s age. BMC. Obesity. 2019;6:11.
Danford C, Schultz C, Marvicsin D. Parental roles in the development of obesity in children: challenges and opportunities. Res Rep Biol. 2014;6:39–53.
Schoeppe S, Vandelanotte C, Bere E, Lien N, Verloigne M, Kovacs E, et al. The influence of parental modelling on children’s physical activity and screen time: does it differ by gender? Eur J Public Health. 2017;27:152–7.
Ministry of Health. Methodology Report 2016/17: New Zealand Health Survey Wellington: Ministry of Health; 2017 [This methodology report details the procedures and protocols followed to ensure the New Zealand Health Survey produces the high-quality and robust data expected of official statistics]. https://www.health.govt.nz/publication/methodology-report-2016-17-new-zealand-health-survey.
Green MA. Do we need to think beyond BMI for estimating population-level health risks? J Public Health. 2015; 192–3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5896802/.
Asia Pacific Cohort Studies Collaboration. Body mass index and cardiovascular disease in the Asia-Pacific Region: an overview of 33 cohorts involving 310,000 participants. Int J Epidemiol. 2004;33:751–8.
World Health Organisation (WHO). The WHO Child Growth Standards Geneva: WHO; 2019. https://www.who.int/childgrowth/en/.
World Health Organisation (WHO). Growth reference data for 5–19 years Geneva: WHO; 2019. https://www.who.int/growthref/en/.
Statistics New Zealand. New Zealand: an urban/rural profile Wellington; 2014.
Erkelenz N, Kobel S, Kettner S, Drenowatz C, Steinacker JM. Parental activity as influence on children’s BMI percentiles and physical activity. J Sports Sci Med. 2014;13:645–50.
Sijtsma A, Sauer PJJ, Corpeleijn E. Parental correlations of physical activity and body mass index in young children-he GECKO Drenthe cohort. Int J Behav Nutr Phys Activity. 2015;12:132.
Hawkins SS, Law C. A review of risk factors for overweight in preschool children: a policy perspective. Int J Pediatr Obes. 2006;1:195–209.
Voerman E, Santos S, Patro Golab B, Amiano P, Ballester F, Barros H, et al. Maternal body mass index, gestational weight gain, and the risk of overweight and obesity across childhood: an individual participant data meta-analysis. PLoS Med. 2019;16:e1002744–e.
Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337:869–73.
Perez-Pastor EM, Metcalf BS, Hosking J, Jeffery AN, Voss LD, Wilkin TJ. Assortative weight gain in mother-daughter and father-son pairs: an emerging source of childhood obesity. Longitudinal study of trios (EarlyBird 43). Int J Obes. 2009;33:727–35.
Andriani H, Liao C-Y, Kuo H-W. Parental weight changes as key predictors of child weight changes. BMC Public Health. 2015;15:645.
Naess M, Sund ER, Holmen TL, Kvaløy K. Implications of parental lifestyle changes and education level on adolescent offspring weight: a population based cohort study—the HUNT study, Norway. BMJ Open. 2018;8:e023406.
Stunkard AJ, Sørensen TIA, Hanis C, Teasdale TW, Chakraborty R, Schull WJ, et al. An adoption study of human obesity. N Engl J Med. 1986;314:193–8.
Stunkard AJ, Harris JR, Pedersen NL, McClearn GE. The body-mass index of twins who have been reared apart. N Engl J Med. 1990;322:1483–7.
Swinburn BA, Sacks G, Hall KD, McPherson K, Finegood DT, Moodie ML, et al. The global obesity pandemic: shaped by global drivers and local environments. Lancet. 2011;378:804–14.
Wang Y, Min J, Khuri J, Li M. A systematic examination of the association between parental and child obesity across countries. Adv Nutr. 2017;8:436–48.
Perez-Pastor EM, Metcalf BS, Hosking J, Jeffery AN, Voss LD, Wilkin TJ. Assortative weight gain in mother–daughter and father–son pairs: an emerging source of childhood obesity. Longitudinal study of trios (EarlyBird 43). Int J Obesity. 2009;33:727–35.
Hesketh K, Waters E, Green J, Salmon L, Williams J. Healthy eating, activity and obesity prevention: a qualitative study of parent and child perceptions in Australia. Health Promot Int. 2005;20:19–26.
Morgan PJ, Young MD, Lloyd AB, Wang ML, Eather N, Miller A, et al. Involvement of fathers in pediatric obesity treatment and prevention trials: a systematic review. Pediatrics. 2017;139:e20162635.
Sigmund E, Sigmundová D, Badura P, Madarasová Gecková A. Health-related parental indicators and their association with healthy weight and overweight/obese children’s physical activity. BMC Public Health. 2018;18:676.
Maatta S, Ray C, Roos E. Associations of parental influence and 10-11-year-old children’s physical activity: are they mediated by children’s perceived competence and attraction to physical activity? Scand J Public Health. 2014;42:45–51.
Acknowledgements
This research was carried out as part of the GeoHealth Laboratory work programme at the University of Canterbury, funded by the New Zealand Ministry of Health. The authors thank the participants within the New Zealand Health Survey. Access to the data used in this study was provided by the New Zealand Ministry of Health under conditions designed to keep individual information confidential and secure in accordance with the requirements of the Health Information Privacy Code 1994 and the Privacy Act 1993. Finally, we would like to thank the staff at the New Zealand Ministry of Health who provided valuable advice to the project. MJD is supported by a Career Development Fellowship (APP1141606) from the National Health and Medical Research Council.
Author information
Authors and Affiliations
Contributions
MH—Drafted manuscript, data analysis, interpretation of results, and submission of article. SS—Conception of idea, advice on data analysis, writing and editing of the manuscript. MD—Conception of idea, advice on data analysis, and editing of the manuscript. CV—Conception of idea, advice on data analysis, and editing of the manuscript. LM—Editing of manuscript and advice on data analysis. JW—Editing of the manuscript and advice on data analysis. MT—Editing of the manuscript. MC—Conception of idea and editing of the manuscript. SK—Conception of idea and editing of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Hobbs, M., Schoeppe, S., Duncan, M.J. et al. Objectively measured waist circumference is most strongly associated in father–boy and mother–girl dyads in a large nationally representative sample of New Zealanders. Int J Obes 45, 438–448 (2021). https://doi.org/10.1038/s41366-020-00699-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-020-00699-w