Abstract
Background/Objectives
Associations between overweight and altered stress biology have been reported cross-sectionally during childhood, but it is unclear whether overweight precedes altered stress biology or if altered stress biology predicts greater likelihood of overweight over time. The current longitudinal study investigates associations between overweight/obesity, salivary alpha amylase and cortisol morning intercept, diurnal slope, and reactivity to social stress in a cohort of low-income children during preschool and middle childhood.
Subjects/Methods
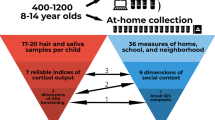
Children were recruited through Head Start and were observed and followed into middle childhood (N = 257; M = 8.0 years). Height and weight were measured at both time points. Saliva samples were collected across the day and in response to a social challenge at both ages for alpha amylase and cortisol determination.
Results
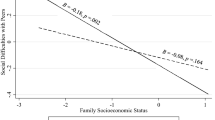
Cross-lagged panel analyses indicated that overweight/obesity at preschool predicted lower morning alpha amylase (β = −0.18, 95% CI: −0.34, −0.03; p = 0.023), lower morning cortisol (β = −0.22, 95% CI: −0.38, −0.06; p = 0.006), lower sAA diurnal slope (β = −0.18, 95% CI: −0.34, −0.03; p = 0.021), and lower cortisol stress reactivity (β = −0.19, 95% CI: −0.35, −0.02; p = 0.031) in middle childhood. Lower alpha amylase reactivity at preschool was the only biological factor that predicted higher likelihood of overweight/obesity at middle childhood (β = −0.20, 95% CI: −0.38, −0.01; p = 0.035).
Conclusions
These findings suggest that overweight/obesity may be driving changes in stress biology across early-to-middle childhood, particularly in downregulation of morning levels of stress hormones, diurnal sAA slope, and cortisol reactivity to stress, rather than stress biology driving overweight/obesity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Ng M, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–81.
Pan L, May AL, Wethington H, Dalenius K, Grummer-Strawn LM. Incidence of obesity among young US children living in low-income families, 2008–2011. Pediatrics. 2013;132:1006–13.
Dallman MF, et al. Glucocorticoids, the etiology of obesity and the metabolic syndrome. Curr Alzheimer Res. 2007;4:199–204.
Dallman MF. Stress-induced obesity and the emotional nervous system. Trends Endocrinol Metab. 2010;21:159–65.
Vicennati V, et al. Cross-talk between adipose tissue and the HPA axis in obesity and overt hypercortisolemic states. Horm Mol Biol Clin Investig. 2014;17:63–77.
Papafotiou C, et al. Hair cortisol concentrations exhibit a positive association with salivary cortisol profiles and are increased in obese prepubertal girls. Stress. 2017;20:217–22.
Reinehr T, et al. Relationships between 24-hour urinary free cortisol concentrations and metabolic syndrome in obese children. J Clin Endocrinol Metab. 2014;99:2391–9.
Kjölhede EA, Gustafsson PE, Gustafsson P, Nelson N. Overweight and obese children have lower cortisol levels than normal weight children. Acta Paediatr. 2014;103:295–9.
Lumeng JC, et al. Diurnal cortisol pattern, eating behaviors and overweight in low-income preschool-aged children. Appetite. 2014;73:65–72.
Veldhorst MA, et al. Increased scalp hair cortisol concentrations in obese children. J Clin Endocrinol Metab. 2014;99:285–90.
Knutsson U, et al. Circadian cortisol rhythms in healthy boys and girls: relationship with age, growth, body composition, and pubertal development. J Clin Endocrinol Metab. 1997;82:536–40.
Törnhage C-J, Αlfvén G. Diurnal salivary cortisol concentration in school-aged children: increased morning cortisol concentration and total cortisol concentration negatively correlated to body mass index in children with recurrent abdominal pain of psychosomatic origin. J Pediatr Endocrinol Metab. 2006;19:843–54.
Hillman JB, Dorn LD, Loucks TL, Berga SL. Obesity and the hypothalamic-pituitary-adrenal axis in adolescent girls. Metab-Clin Exp. 2012;61:341–8.
Ruttle PL, et al. Concurrent and longitudinal associations between diurnal cortisol and body mass index across adolescence. J Adolesc Health. 2013;52:731–7.
Dockray S, Susman EJ, Dorn LD. Depression, cortisol reactivity and obesity in childhood and adolescence. J Adolesc Health. 2009;45:344–50.
Francis L, Granger D, Susman E. Adrenocortical regulation, eating in the absence of hunger and BMI in young children. Appetite. 2013;64:32–8.
Miller AL, et al. Blunted cortisol response to stress is associated with higher body mass index in low-income preschool-aged children. Psychoneuroendocrinology. 2013;38:2611–7.
Davy KP, Orr JS. Sympathetic nervous system behavior in human obesity. Neurosci Biobehav Rev. 2009;33:116–24.
Tataranni PA, Young JB, Bogardus C, Ravussin E. A low sympathoadrenal activity is associated with body weight gain and development of central adiposity in Pima Indian men. Obesity. 1997;5:341–7.
Tentolouris N, Liatis S, Katsilambros N. Sympathetic system activity in obesity and metabolic syndrome. Ann N Y Acad Sci. 2006;1083:129–52.
Latchman PL, Mathur M, Bartels MN, Axtell RS, De Meersman RE. Impaired autonomic function in normotensive obese children. Clin Autonomic Res. 2011;21:319–23.
Kuebler U, et al. Norepinephrine infusion with and without alpha-adrenergic blockade by phentolamine increases salivary alpha amylase in healthy men. Psychoneuroendocrinology. 2014;49:290–8.
Nater UM, Rohleder N. Salivary alpha-amylase as a non-invasive biomarker for the sympathetic nervous system: current state of research. Psychoneuroendocrinology. 2009;34:486–96.
Nater UM, Rohleder N, Schlotz W, Ehlert U, Kirschbaum C. Determinants of the diurnal course of salivary alpha-amylase. Psychoneuroendocrinology. 2007;32:392–401.
Hill-Soderlund AL, et al. The developmental course of salivary alpha-amylase and cortisol from 12 to 36 months: Relations with early poverty and later behavior problems. Psychoneuroendocrinology. 2015;52:311–23.
Morrison SF. Differential control of sympathetic outflow. Am J Physiol-Regulatory Integr Comp Physiol. 2001;281:R683–98.
Alkon A, et al. Latino children’s body mass index at 2–3.5 years predicts sympathetic nervous system activity at 5 years. Child Obes. 2014;10:214–24.
Rodríguez-Colón SM, Bixler EO, Li X, Vgontzas AN, Liao D. Obesity is associated with impaired cardiac autonomic modulation in children. Pediatr Obes. 2011;6:128–34.
Soares-Miranda L, et al. Central fat influences cardiac autonomic function in obese and overweight girls. Pediatr Cardiol. 2011;32:924–8.
Vanderlei LCM, Pastre CM, Freitas Júnior IF, Godoy MFd. Analysis of cardiac autonomic modulation in obese and eutrophic children. Clinics. 2010;65:789–92.
Baum P, Petroff D, Classen J, Kiess W, Blüher S. Dysfunction of autonomic nervous system in childhood obesity: a cross-sectional study. PLoS ONE. 2013;8:e54546.
Papafotiou C, et al. Increased salivary and hair cortisol and decreased salivary alpha-amylase concentrations in obese prepubertal girls. 55th Annual European Society for Paediatric Endocrinology. 2016.
Miller AL, et al. Salivary alpha amylase diurnal pattern and stress response are associated with body mass index in low-income preschool-aged children. Psychoneuroendocrinology. 2015;53:40–8.
Miller AL, et al. Associations between stress biology indicators and overweight across toddlerhood. Psychoneuroendocrinology. 2017;79:98–106.
Miller AL, et al. Early childhood stress and child age predict longitudinal increases in obesogenic eating among low-income children. Acad Pediatr. 2018;18:685–91.
Kuczmarski RJ, et al. CDC growth charts for the United States: methods and development. Vital- health Stat Ser 11. 2000;2002:1–190.
Hu L-t, Bentler PM. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods. 1998;3:424.
Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Long KABJS, editor. Testing structural equation models. Newbury Park, CA: Sage; 1993. p. 136–62.
Björntorp P. Do stress reactions cause abdominal obesity and comorbidities? Obes Rev. 2001;2:73–86.
Björntorp P. Endocrine abnormalities of obesity. Metab-Clin Exp. 1995;44:21–3.
Rosmond R, Dallman MF, Björntorp P. Stress-related cortisol secretion in men: Relationships with abdominal obesity and endocrine, metabolic and hemodynamic abnormalities. J Clin Endocrinol Metab. 1998;83:1853–9.
Lee M-J, Pramyothin P, Karastergiou K, Fried SK. Deconstructing the roles of glucocorticoids in adipose tissue biology and the development of central obesity. Biochimica et Biophysica Acta. 2014;1842:473–81.
Miller GE, Chen E, Zhou ES. If it goes up, must it come down? Chronic stress and the hypothalamic-pituitary-adrenocortical axis in humans. Psychological Bull. 2007;133:25–45.
Gunnar MR, Vazquez DM. Low cortisol and a flattening of expected daytime rhythm: Potential indices of risk in human development. Dev Psychopathol. 2001;13:515–38.
Heim C, Ehlert U, Hellhammer DH. The potential role of hypocortisolism in the pathophysiology of stress-related bodily disorders. Psychoneuroendocrinology. 2000;25:1–35.
Ouellet-Morin I, et al. Blunted cortisol responses to stress signal social and behavioral problems among maltreated/bullied 12-year-old children. Biol Psychiatry. 2011;70:1016–23.
Lumeng JC, Gannon K, Cabral HJ, Frank DA, Zuckerman B. Association between clinically meaningful behavior problems and overweight in children. Pediatrics. 2003;112:1138–45.
Meaney MJ, Szyf M, Seckl JR. Epigenetic mechanisms of perinatal programming of hypothalamic-pituitary-adrenal function and health. Trends Mol Med. 2007;13:269–77.
Steptoe A, van Jaarsveld CH, Semmler C, Plomin R, Wardle J. Heritability of daytime cortisol levels and cortisol reactivity in children. Psychoneuroendocrinology. 2009;34:273–80.
Locke AE, et al. Genetic studies of body mass index yield new insights for obesity biology. Nature. 2015;518:197.
Evans GW, Kim P. Childhood poverty and health: cumulative risk exposure and stress dysregulation. Psychol Sci. 2007;18:953–7.
Harthoorn LF, Dransfield E. Periprandial changes of the sympathetic–parasympathetic balance related to perceived satiety in humans. Eur J Appl Physiol. 2008;102:601–8.
Taşçılar ME, et al. Cardiac autonomic functions in obese children. J Clin Res Pediatr Endocrinol. 2011;3:60.
Altuncu ME, Baspinar O, Keskin M. The use of short-term analysis of heart rate variability to assess autonomic function in obese children and its relationship with metabolic syndrome. Cardiol J. 2012;19:501–6.
Rothman KJ. Six persistent research misconceptions. J Gen Intern Med. 2014;29:1060–4.
Acknowledgements
This research was supported by funding from F32HD088029 (PI: JRD), NICHD/NIDDK R01 DK095695 (PI: ALM and JCL), NIDDK R21DK090718 (PI: ALM and JCL), American Heart Association 10GRNT4460043 (PI: ALM), and NIDDK RC1DK086376 (PI: JCL).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Doom, J.R., Lumeng, J.C., Sturza, J. et al. Longitudinal associations between overweight/obesity and stress biology in low-income children. Int J Obes 44, 646–655 (2020). https://doi.org/10.1038/s41366-019-0447-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-019-0447-4