Abstract
Background/Objectives
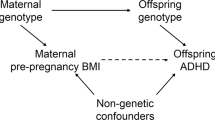
Attention-deficit hyperactivity disorder (ADHD), one of the most common neurodevelopmental disorders in childhood and adolescence, is associated with obesity in observational studies. However, it is unclear whether ADHD contributes to, results from or is merely correlated with obesity. This study evaluates the presence and direction of a causal effect between ADHD and obesity.
Subjects/Methods
We performed a bidirectional two-sample Mendelian randomization using summary data from consortia of genome-wide association studies to investigate if ADHD (N = 55,374) has a causal effect on body mass index (BMI) in childhood (N = 35,668) and adulthood (N = 322,154–500,000), and vice-versa. The main analysis was performed using the inverse variance weighted (IVW) method. As sensitivity analyses, we used other Mendelian randomization methods that are more robust to horizontal pleiotropy (i.e., MR-Egger, weighted mode, and penalized weighted median estimators), as well as stratified the analysis by the putative mechanisms of genetic instruments (i.e., pathways involved or not in neurological processes).
Results
The IVW method indicated a positive causal effect of BMI on ADHD: β = 0.324 (95% CI 0.198 to 0.449, p < 0.001; expressed as change in ln(odds ratio) of ADHD per each additional SD unit of BMI). IVW estimates were directionally consistent with other methods. On the other hand, we did not find consistent evidence for a causal effect of ADHD genetic liability on BMI.
Conclusions
The results suggested that higher BMI increases the risk of developing ADHD, but not the other way around.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
WHO. The World Health Report 2002: Reducing risks, promoting healthy life. 2002.
Reilly JJ, Methven E, McDowell ZC, Hacking B, Alexander D, Stewart L. et al. Health consequences of obesity. Arch Dis Child. 2003;88:748–52.
Klein RG, Mannuzza S, Olazagasti MA, Roizen E, Hutchison JA, Lashua EC, et al. Clinical and functional outcome of childhood attention-deficit/hyperactivity disorder 33 years later. Arch Gen Psychiatry. 2012;69:1295–303.
van Emmerik-van Oortmerssen K, van de Glind G, van den Brink W, Smit F, Crunelle CL, Swets M, et al. Prevalence of attention-deficit hyperactivity disorder in substance use disorder patients: a meta-analysis and meta-regression analysis. Drug alcohol Depend. 2012;122:11–9.
Dalsgaard S, Mortensen PB, Frydenberg M, Thomsen PH. Long-term criminal outcome of children with attention deficit hyperactivity disorder. Crim Behav Ment Health. 2013;23:86–98.
Narad M, Garner AA, Brassell AA, Saxby D, Antonini TN, O'Brien KM, et al. Impact of distraction on the driving performance of adolescents with and without attention-deficit/hyperactivity disorder. JAMA Pediatr. 2013;167:933–8.
Maxson RT, Lawson KA, Pop R, Yuma-Guerrero P, Johnson KM. Screening for attention-deficit/hyperactivity disorder in a select sample of injured and uninjured pediatric patients. J Paediatr Surg. 2009;44:743–8.
Dubnov-Raz G, Perry A, Berger I. Body mass index of children with attention-deficit/hyperactivity disorder. J Child Neurol. 2011;26:302–8.
Lam LT, Yang L. Overweight/obesity and attention deficit and hyperactivity disorder tendency among adolescents in China. Int J Obes. 2007;31:584–90.
Byrd HC, Curtin C, Anderson SE. Attention-deficit/hyperactivity disorder and obesity in US males and females, age 8–15 years: National Health and Nutrition Examination Survey 2001–2004. Pediatr Obes. 2013;8:445–53.
Yang R, Mao S, Zhang S, Li R, Zhao Z. Prevalence of obesity and overweight among Chinese children with attention deficit hyperactivity disorder: A survey in Zhejiang Province, China. BMC Psychiatry. 2013;13-133.
Cortese S, Moreira-Maia CR, St Fleur D, Morcillo-Penalver C, Rohde LA, Faraone SV. Association Between ADHD and Obesity: A Systematic Review and Meta-Analysis. Am J Psychiatry. 2016;173:34–43.
Demontis D, Walters RK, Martin J, Mattheisen M, Als TD, Agerbo E. et al. Discovery of the first genome wide significant risk loci for attention deficit/hyperactivity disorder. Nature genetics. 2019;51:63–75.
Albayrak O, Putter C, Volckmar AL, Cichon S, Hoffmann P, Nothen MM. et al. Common obesity risk alleles in childhood attention-deficit/hyperactivity disorder. Am J Med Genet B Neuropsychiatr Genet. 2013;162B:295–305.
Du Rietz E, Coleman J, Glanville K, Choi SW, O'Reilly PF, Kuntsi J. Association of Polygenic Risk for Attention-Deficit/Hyperactivity Disorder With Co-occurring Traits and Disorders. Biological psychiatry Cognitive neuroscience and neuroimaging. 2018;3:635–43.
Cortese S, Ramos Olazagasti MA, Klein RG, Castellanos FX, Proal E, Mannuzza S. Obesity in men with childhood ADHD: a 33-year controlled, prospective, follow-up study. Pediatrics. 2013;131:e1731–8.
White B, Nicholls D, Christie D, Cole TJ, Viner RM. Childhood psychological function and obesity risk across the lifecourse: findings from the 1970 British Cohort Study. Int J Obes. 2012;36:511–6.
Khalife N, Kantomaa M, Glover V, Tammelin T, Laitinen J, Ebeling H. et al. Childhood attention-deficit/hyperactivity disorder symptoms are risk factors for obesity and physical inactivity in adolescence. J Am Acad Child Adolesc Psychiatry.2014;53:425–36.
Cortese S, Tessari L. Attention-Deficit/Hyperactivity Disorder (ADHD) and Obesity: Update 2016. Current Psychiatry Rep. 2017;19:4.
Perez-Bonaventura I, Granero R, Ezpeleta L. The relationship between weight status and emotional and behavioral problems in Spanish preschool children. J Pediatr Psychol. 2015;40:455–63.
Vogel SW, Bijlenga D, Tanke M, Bron TI, van der Heijden KB, Swaab H. et al. Circadian rhythm disruption as a link between Attention-Deficit/Hyperactivity Disorder and obesity?. J Psychosom Res. 2015;79:443–50.
Cortese S, Vincenzi B. Obesity and ADHD: clinical and neurobiological implications. Curr Top Behav Neurosci. 2012;9:199–218.
Lawlor DA, Tilling K, Davey Smith G. Triangulation in aetiological epidemiology. Int J Epidemiol. 2016;45:1866–86.
Greenland S. An introduction to instrumental variables for epidemiologists. Int J Epidemiol. 2000;29:722–9.
Hartwig FP, Bowden J, Loret de Mola C, Tovo-Rodrigues L, Davey Smith G, Horta BL. Body mass index and psychiatric disorders: a Mendelian randomization study. Sci Rep. 2016;6:32730.
Felix JF, Bradfield JP, Monnereau C, van der Valk RJ, Stergiakouli E, Chesi A. et al. Genome-wide association analysis identifies three new susceptibility loci for childhood body mass index. Hum Mol Genet. 2016;25:389–403.
Locke AE, Kahali B, Berndt SI, Justice AE, Pers TH, Day FR, et al. Genetic studies of body mass index yield new insights for obesity biology. Nature. 2015;518:197–206.
UKBiobank. "Rapid GWAS of thousands of phenotypes for 337,000 samples in the UK Biobank". Retrieved November 22, 2017, from http://www.nealelab.is/blog/2017/7/19/rapid-gwas-of-thousands-of-phenotypes-for-337000-samples-in-the-uk-biobank. 2015.
UK Biobank. Genotyping and quality control of UK Biobank, a large-scale, extensively phenotyped prospective resource. 2015 [cited 2017 November 22]; Available from: http://www.ukbiobank.ac.uk/wp-content/uploads/2014/04/UKBiobank_genotyping_QC_documentation-web.pdf.
UK Biobank Genotype imputation and genetic association studies of UK Biobank, 2015 [cited 2017 November 22]; Available from: http://www.ukbiobankacuk/wp-content/uploads/2014/04/imputation_documentation_May2015pdf.
Auton A, Brooks LD, Durbin RM, Garrison EP, Kang HM, Korbel JO, et al. A global reference for human genetic variation. Nature. 2015;526:68–74.
Arnold M, Raffler J, Pfeufer A, Suhre K, Kastenmüller, G SNiPA: an interactive, genetic variant-centered annotation browser. Bioinformatics first published onlineNovember 26, 2014 https://doi.org/10.1093/bioinformatics/btu779 OPEN ACCESS.
Machiela MJ, Chanock SJ. LDlink: a web-based application for exploring population-specific haplotype structure and linking correlated alleles of possible functional variants. Bioinformatics. 2015;31:3555–7.
Hemani G, Zheng J, Elsworth B, Wade KH, Haberland V, Baird D. et al. The MR-Base platform supports systematic causal inference across the human phenome. Elife. 2018;7:e34408.
Burgess S, Butterworth A, Thompson SG. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol. 2013;37:658–65.
Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 2015;44:512–25.
Bowden J, Davey Smith G, Haycock PC, Burgess S. Consistent Estimation in Mendelian Randomization with Some Invalid Instruments Using a Weighted Median Estimator. Genet Epidemiol. 2016;40:304–14.
Hartwig FP, Davey Smith G, Bowden J. Robust inference in summary data Mendelian randomization via the zero modal pleiotropy assumption. Int J Epidemiol. 2017;46:1985–98.
Zheng J, Haycock P, Hemani G, Elsworth B, Shihab H, Laurin C, et al. LD hub and MR-base: online platforms for preforming LD score regression and Mendelian randomization analysis using GWAS summary data 2016.
Aguirre Castaneda RL, Kumar S, Voigt RG, Leibson CL, Barbaresi WJ, Weaver AL. et al. Childhood attention-deficit/hyperactivity disorder, sex, and obesity: A Longitudinal Population-Based Study. Mayo Clin Proc. 2016;91:352–61.
Davis C, Levitan RD, Smith M, Tweed S, Curtis C. Associations among overeating, overweight, and attention deficit/hyperactivity disorder: a structural equation modelling approach. Eat Behav. 2006;7:266–74.
van Egmond-Frohlich AW, Weghuber D, de Zwaan M. Association of symptoms of attention-deficit/hyperactivity disorder with physical activity, media time, and food intake in children and adolescents. PLoS ONE. 2012;7:e49781.
Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 2006;36:159–65.
Cortese S, Isnard P, Frelut ML, Michel G, Quantin L, Guedeney A. et al. Association between symptoms of attention-deficit/hyperactivity disorder and bulimic behaviors in a clinical sample of severely obese adolescents. Int J Obes. 2007;31:340–6.
Levitan RD, Masellis M, Lam RW, Muglia P, Basile VS, Jain U, et al. Childhood inattention and dysphoria and adult obesity associated with the dopamine D4 receptor gene in overeating women with seasonal affective disorder. Neuropsychopharmacology. 2004;29:179–86.
Schweickert LA, Strober M, Moskowitz A. Efficacy of methylphenidate in bulimia nervosa comorbid with attention-deficit hyperactivity disorder: a case report. Int J Eat Disord. 1997;21:299–301.
Smith GD, Lawlor DA, Harbord R, Timpson N, Day I, Ebrahim S. Clustered environments and randomized genes: a fundamental distinction between conventional and genetic epidemiology. PLoS Med. 2007;4:e352.
Schrader H, Bovim G, Sand T. The prevalence of delayed and advanced sleep phase syndromes. J Sleep Res. 1993;2:51–5.
Hvolby A. Associations of sleep disturbance with ADHD: implications for treatment. Atten Defic Hyperact Disord. 2015;7:1–18.
Owens JA. The ADHD and sleep conundrum: a review. J Dev Behav Pediatr. 2005;26:312–22.
Yang H, Youm YH, Vandanmagsar B, Ravussin A, Gimble JM, Greenway F, et al. Obesity increases the production of proinflammatory mediators from adipose tissue T cells and compromises TCR repertoire diversity: implications for systemic inflammation and insulin resistance. J Immunol. 2010;185:1836–45.
Chen HJ, Lee YJ, Yeh GC, Lin HC. Association of attention-deficit/hyperactivity disorder with diabetes: a population-based study. Pediatr Res. 2013;73(4 Pt 1):492–6.
Burgess S, Bowden J, Fall T, Ingelsson E, Thompson SG. Sensitivity analyses for robust causal inference from Mendelian randomization analyses with multiple genetic variants. Epidemiology. 2017;28:30–42.
Acknowledgements
TMS received a scholarship for a PhD’s degree from the Coordination of Improvement of Higher Level Personnel (CAPES). This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—Brasil (CAPES)—Finance Code 001. MCB is supported by a UK Medical Research Council (MRC) Skills Development Fellowship (MR/P014054/1). FPH is supported by a Brazilian National Council for Scientific and Technological Development (CNPq) postdoctoral fellowship. We wish to thank Vanessa Rodrigues Paixão-Côrtes for her assistance with the figures editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
LAR has been a member of the speakers’ bureau/advisory board and/or acted as a consultant for Eli-Lilly, Janssen-Cilag, Medice, Novartis and Shire in the last 3 years. He receives authorship royalties from Oxford Press and ArtMed. He has also received travel awards from Shire for his participation in the 2018 APA meetings and from Novartis to take part of the 2016 AACAP meeting. The ADHD and Juvenile Bipolar Disorder Outpatient Programs chaired by him received unrestricted educational and research support from the following pharmaceutical companies in the last 3 years: Janssen - Cilag, Novartis, and Shire. The remaining authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Martins-Silva, T., Vaz, J.d.S., Hutz, M.H. et al. Assessing causality in the association between attention-deficit/hyperactivity disorder and obesity: a Mendelian randomization study. Int J Obes 43, 2500–2508 (2019). https://doi.org/10.1038/s41366-019-0346-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-019-0346-8
This article is cited by
-
No evidence for a causal contribution of bioavailable testosterone to ADHD in sex-combined and sex-specific two-sample Mendelian randomization studies
European Child & Adolescent Psychiatry (2024)
-
Emotional problems mediate the association between attention deficit/hyperactivity disorder and obesity in adolescents
BMC Psychiatry (2023)
-
ADHD in childhood predicts BMI and body composition measurements over time in a population-based birth cohort
International Journal of Obesity (2022)
-
Large-scale genetic investigation reveals genetic liability to multiple complex traits influencing a higher risk of ADHD
Scientific Reports (2021)
-
Two genetic analyses to elucidate causality between body mass index and personality
International Journal of Obesity (2021)