Abstract
Objective
Exposure to impaired gestational glucose tolerance has been shown to have sex-specific associations with offspring obesity risk, perhaps by affecting the development of appetite regulation. We examined the extent to which prenatal exposure to impaired glucose tolerance was associated with eating in the absence of hunger (EAH) in early adolescent offspring, and in turn, whether EAH was cross-sectionally associated with body composition.
Methods
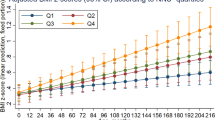
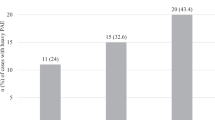
We included data from 1097 adolescents participating in Project Viva, a pre-birth longitudinal cohort. We obtained the results of two-stage prenatal glycemic screening (50 g glucose challenge test, followed if abnormal by 100 g oral glucose tolerance test) at 26–28 weeks of gestation, and categorized mothers as having normal glucose tolerance, isolated hyperglycemia (IH, n = 92, 8.4%), impaired glucose tolerance (IGT, n = 36, 3.3%), or gestational diabetes mellitus (GDM, n = 52, 4.7%). At a median age of 13 years, offspring reported on two modified items of the Eating in the Absence of Hunger in Children and Adolescents questionnaire, we measured height and weight, and performed dual X-ray absorptiometry scans to assess fat and fat-free mass. We used multivariable linear regression analyses adjusted for sociodemographic and prenatal covariates, including maternal pre-pregnancy BMI.
Results
On a ten-point scale, the mean (SD) EAH score was 4.4 points (SD = 1.5) in boys and 4.4 (SD = 1.4) in girls. In girls, prenatal exposure to both IH and IGT was associated with more EAH compared with normal glucose tolerance (e.g., for IH: 0.56 points, 95% CI: 0.17, 0.96), whereas in boys, prenatal exposure to IGT was associated with less EAH (–0.81 points, 95% CI: −1.41, −0.21). We did not observe an association between exposure to GDM and EAH, nor did we observe associations between EAH and body composition in early adolescence.
Conclusions
These findings suggest sex-specific associations of exposure to impaired gestational glucose tolerance with offspring EAH in early adolescence.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Ferrara A. Increasing prevalence of gestational diabetes mellitus: a public health perspective. Diabetes Care. 2007;30(Suppl 2):S141–6.
DeSisto CL, Kim SY, Sharma AJ. Prevalence estimates of gestational diabetes mellitus in the United States, Pregnancy Risk Assessment Monitoring System (PRAMS), 2007-2010. Prev Chronic Dis. 2014;11:E104.
Lavery JA, Friedman AM, Keyes KM, Wright JD, Ananth CV. Gestational diabetes in the United States: temporal changes in prevalence rates between 1979 and 2010. BJOG. 2017;124:804–13.
Page KA, Romero A, Buchanan TA, Xiang AH. Gestational diabetes mellitus, maternal obesity, and adiposity in offspring. J Pediatr. 2014;164:807–10.
Gillman MW, Rifas-Shiman S, Berkey CS, Field AE, Colditz GA. Maternal gestational diabetes, birth weight, and adolescent obesity. Pediatrics. 2003;111:e221–6.
Zhao YL, Ma RM, Lao TT, Chen Z, Du MY, Liang K, et al. Maternal gestational diabetes mellitus and overweight and obesity in offspring: a study in Chinese children. J Dev Orig Health Dis. 2015;6:479–84.
Kim SY, England JL, Sharma JA, Njoroge T. Gestational diabetes mellitus and risk of childhood overweight and obesity in offspring: a systematic review. Exp Diabetes Res. 2011;2011:541308.
Regnault N, Gillman MW, Rifas-Shiman SL, Eggleston E, Oken E. Sex-specific associations of gestational glucose tolerance with childhood body composition. Diabetes Care. 2013;36:3045–53.
Franks PW, Looker HC, Kobes S, Touger L, Tataranni PA, Hanson RL, et al. Gestational glucose tolerance and risk of type 2 diabetes in young Pima Indian offspring. Diabetes. 2006;55:460–5.
Breier BH, Vickers MH, Ikenasio BA, Chan KY, Wong WP. Fetal programming of appetite and obesity. Mol Cell Endocrinol. 2001;185:73–9.
Neary NM, Goldstone AP, Bloom SR. Appetite regulation: from the gut to the hypothalamus. Clin Endocrinol (Oxf). 2004;60:153–60.
Langley-Evans SC, Bellinger L, McMullen S. Animal models of programming: early life influences on appetite and feeding behaviour. Matern Child Nutr. 2005;1:142–8.
Steculorum SM, Bouret SG. Maternal diabetes compromises the organization of hypothalamic feeding circuits and impairs leptin sensitivity in offspring. Endocrinology. 2011;152:4171–9.
Muhlhausler BS, Duffield JA, McMillen IC. Increased maternal nutrition increases leptin expression in perirenal and subcutaneous adipose tissue in the postnatal lamb. Endocrinology. 2007;148:6157–63.
Ornellas F, Souza-Mello V, Mandarim-de-Lacerda CA, Aguila MB. Combined parental obesity augments single-parent obesity effects on hypothalamus inflammation, leptin signaling (JAK/STAT), hyperphagia, and obesity in the adult mice offspring. Physiol Behav. 2016;153:47–55.
Morris MJ, Chen H. Established maternal obesity in the rat reprograms hypothalamic appetite regulators and leptin signaling at birth. Int J Obes (Lond). 2009;33:115–22.
Fisher JO, Birch LL. Restricting access to foods and children’s eating. Appetite. 1999;32:405–19.
Lansigan RK, Emond JA, Gilbert-Diamond D. Understanding eating in the absence of hunger among young children: a systematic review of existing studies. Appetite. 2015;85:36–47.
Francis LA, Ventura AK, Marini M, Birch LL. Parent overweight predicts daughters’ increase in BMI and disinhibited overeating from 5 to 13 years. Obes (Silver Spring). 2007;15:1544–53.
Faith MS, Berkowitz RI, Stallings VA, Kerns J, Storey M, Stunkard AJ. Eating in the absence of hunger: a genetic marker for childhood obesity in prepubertal boys? Obes (Silver Spring). 2006;14:131–8.
Wardle J, Guthrie C, Sanderson S, Birch L, Plomin R. Food and activity preferences in children of lean and obese parents. Int J Obes Relat Metab Disord. 2001;25:971–7.
Shapiro ALB, Sauder KA, Tregellas JR, Legget KT, Gravitz SL, Ringham BM, et al. Exposure to maternal diabetes in utero and offspring eating behavior: The EPOCH study. Appetite. 2017;116:610–5.
Fisher JO, Cai G, Jaramillo SJ, Cole SA, Comuzzie AG, Butte NF. Heritability of hyperphagic eating behavior and appetite-related hormones among Hispanic children. Obesity. 2007;15:1484–95.
Oken E, Baccarelli AA, Gold DR, Kleinman KP, Litonjua AA, De Meo D, et al. Cohort profile: project viva. Int J Epidemiol. 2015;44:37–48.
Wright CS, Rifas-Shiman SL, Rich-Edwards JW, Taveras EM, Gillman MW, Oken E. Intrauterine exposure to gestational diabetes, child adiposity, and blood pressure. Am J Hypertens. 2009;22:215–20.
Tanofsky-Kraff M, Ranzenhofer LM, Yanovski SZ, Schvey NA, Faith M, Gustafson J, et al. Psychometric properties of a new questionnaire to assess eating in the absence of hunger in children and adolescents. Appetite. 2008;51:148–55.
Rifas-Shiman SL, Willett WC, Lobb R, Kotch J, Dart C, Gillman MW. PrimeScreen, a brief dietary screening tool: reproducibility and comparability with both a longer food frequency questionnaire and biomarkers. Public Health Nutr. 2001;4:249–54.
Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat. Series 11, 2002;246:1–190.
Willett W. Nutritional Epidemiology. 2. New York, NY: Oxford University Press; 1998.
Lange NE, Rifas-Shiman SL, Camargo CA Jr., Gold DR, Gillman MW, Litonjua AA. Maternal dietary pattern during pregnancy is not associated with recurrent wheeze in children. J Allergy Clin Immunol. 2010;126:250–5. 5 e1-4
Fawzi WW, Rifas-Shiman SL, Rich-Edwards JW, Willett WC, Gillman MW. Calibration of a semi-quantitative food frequency questionnaire in early pregnancy. Ann Epidemiol. 2004;14:754–62.
Oken E, Kleinman KP, Rich-Edwards J, Gillman MW. A nearly continuous measure of birth weight for gestational age using a United States national reference. BMC Pediatr. 2003;3:6.
VanderWeele TJ, Mumford SL, Schisterman EF. Conditioning on intermediates in perinatal epidemiology. Epidemiology. 2012;23:1–9.
Gingras V, Rifas-Shiman SL, Derks IPM, Aris IM, Oken E, Hivert MF. Associations of Gestational Glucose Tolerance with Offspring Body Composition and Estimated Insulin Resistance in Early Adolescence. Diabetes Care. 2018. https://doi.org/10.2337/dc18-1490 [e-pub ahead of print].
Regnault N, Botton J, Heude B, Forhan A, Hankard R, Foliguet B, et al. Higher cord C-peptide concentrations are associated with slower growth rate in the 1st year of life in girls but not in boys. Diabetes. 2011;60:2152–9.
O’Tierney-Ginn P, Presley L, Minium J, Hauguel deMouzon S, Catalano PM. Sex-specific effects of maternal anthropometrics on body composition at birth. Am J Obstet Gynecol. 2014;211:292 e1–9.
Landon MB, Rice MM, Varner MW, Casey BM, Reddy UM, Wapner RJ, et al. Mild gestational diabetes mellitus and long-term child health. Diabetes Care. 2015;38:445–52.
Okereke NC, Uvena-Celebrezze J, Hutson-Presley L, Amini SB, Catalano PM. The effect of gender and gestational diabetes mellitus on cord leptin concentration. Am J Obstet Gynecol. 2002;187:798–803.
Kostalova L, Leskova L, Kapellerova A, Strbak V. Body mass, plasma leptin, glucose, insulin and C-peptide in offspring of diabetic and non-diabetic mothers. Eur J Endocrinol. 2001;145:53–8.
Oken E, Morton-Eggleston E, Rifas-Shiman SL, Switkowski KM, Hivert MF, Fleisch AF, et al. Sex-Specific Associations of Maternal Gestational Glycemia with Hormones in Umbilical Cord Blood at Delivery. Am J Perinatol. 2016;33:1273–81.
Allard C, Desgagne V, Patenaude J, Lacroix M, Guillemette L, Battista MC, et al. Mendelian randomization supports causality between maternal hyperglycemia and epigenetic regulation of leptin gene in newborns. Epigenetics. 2015;10:342–51.
De Silva A, Salem V, Matthews PM, Dhillo WS. The Use of Functional MRI to Study Appetite Control in the CNS. Experimental Diabetes Res 2012;2012:1–13.
Birch LL, Fisher JO, Davison KK. Learning to overeat: maternal use of restrictive feeding practices promotes girls’ eating in the absence of hunger. Am J Clin Nutr. 2003;78:215–20.
Fisher JO, Birch LL. Eating in the absence of hunger and overweight in girls from 5 to 7 y of age. Am J Clin Nutr. 2002;76:226–31.
Shunk JA, Birch LL. Girls at risk for overweight at age 5 are at risk for dietary restraint, disinhibited overeating, weight concerns, and greater weight gain from 5 to 9 years. J Am Diet Assoc. 2004;104:1120–6.
Francis LA, Birch LL. Maternal weight status modulates the effects of restriction on daughters’ eating and weight. Int J Obes (Lond). 2005;29:942–9.
Moens E, Braet C. Predictors of disinhibited eating in children with and without overweight. Behav Res Ther. 2007;45:1357–68.
Hill C, Llewellyn CH, Saxton J, Webber L, Semmler C, Carnell S, et al. Adiposity and ‘eating in the absence of hunger’ in children. Int J Obes (Lond). 2008;32:1499–505.
Butte NF, Cai G, Cole SA, Wilson TA, Fisher JO, Zakeri IF, et al. Metabolic and behavioral predictors of weight gain in Hispanic children: the Viva la Familia Study. Am J Clin Nutr. 2007;85:1478–85.
Kelly NR, Shomaker LB, Pickworth CK, Brady SM, Courville AB, Bernstein S, et al. A prospective study of adolescent eating in the absence of hunger and body mass and fat mass outcomes. Obes (Silver Spring). 2015;23:1472–8.
Madowitz J, Liang J, Peterson CB, Rydell S, Zucker NL, Tanofsky-Kraff M, et al. Concurrent and convergent validity of the eating in the absence of hunger questionnaire and behavioral paradigm in overweight children. Int J Eat Disord. 2014;47:287–95.
Acknowledgements
Project Viva is supported by the National Institutes of Health (R01 HD034568, UG3OD023286). We appreciate the dedication of Project Viva participants and staff. This study was supported by the Dutch KNAW Ter Meulen Foundation. PWJ is supported by the Dutch Diabetes Foundation (grant number: 2013.81.1664).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Derks, I.P.M., Hivert, MF., Rifas-Shiman, S.L. et al. Associations of prenatal exposure to impaired glucose tolerance with eating in the absence of hunger in early adolescence. Int J Obes 43, 1903–1913 (2019). https://doi.org/10.1038/s41366-018-0296-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0296-6
This article is cited by
-
Developmental Programming of Body Composition: Update on Evidence and Mechanisms
Current Diabetes Reports (2019)