Abstract
Background/Objective
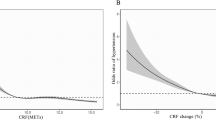
Obesity is a chronic disease, a risk factor for other chronic conditions and for early mortality, and is associated with higher health care utilization. Annual spending among obese individuals is at least 30% higher vs. that for normal-weight peers. In contrast, higher cardiorespiratory fitness (CRF) is related to many health benefits. We sought to examine the association between CRF and health care costs across the spectrum of body mass index (BMI).
Methods
Data from 3,924 men (58.1 ± 11.1 years, 29.2 ± 5.3 kg.m−2) who completed a maximal exercise test for clinical reasons and to estimate CRF were recorded prospectively at the time of testing. Cost data (USD) from each subject during a 6-year period after the exercise test were merged with the exercise database and compared according to BMI and estimated CRF (CRFe). Subjects were categorized as normal-weight (BMI < 25.0 kg.m−2), overweight (BMI 25.0–29.9 kg.m−2), and obese (BMI ≥ 30.0 kg.m−2). We also formed four CRFe categories based on age-stratified quartiles of metabolic equivalents (METs) achieved: least-fit (5.1 ± 1.5 METs; n = 1,044), moderately-fit (7.6 ± 1.5 METs; n = 938), fit (9.4 ± 1.5 METs; n = 988), and highly-fit (12.4 ± 2.2 METs; n = 954).
Results
Average annual costs per person adjusted for age and presence of cardiovascular disease were $37,018, $40,572, and $45,683 for normal-weight, overweight, and obese subjects, respectively (p < 0.01). For each 1-MET incremental increase in CRFe, annual cost savings per person were $3,272, $4,252, and $6,103 for normal-weight, overweight, and obese subjects, respectively. Stratified by CRFe categories, annual costs for normal-weight, overweight, and obese subjects in the highest CRFe quartile were $28,028, $31,669, and $32,807 lower, respectively, compared to subjects in the lowest CRFe quartile (p < 0.01).
Conclusion
Higher CRFe is associated with lower health care costs. Cost savings were particularly evident in obese subjects, suggesting that the economic burden of obesity may be reduced through interventions that target improvements in CRF.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
World and Health Organization (WHO). Fact sheet on obesity and overweight. http://www.who.int/mediacentre/factsheets. Accessed 10 Jan 2018.
Nguyen NT, Magno CP, Lane KT, Hinojosa MW, Lane JS. Association of hypertension, diabetes, dyslipidemia, and metabolic syndrome with obesity: findings from the National Health and Nutrition Examination Survey, 1999 to 2004. J Am Coll Surg. 2008;207:928–34.
Hall JE, do Carmo JM, da Silva AA, Wang Z, Hall ME. Obesity-induced hypertension: interaction of neurohumoral and renal mechanisms. Circ Res. 2015;116:991–1006.
Arnold M, Leitzmann M, Freisling H, Bray F, Romieu I, Renehan A, et al. Obesity and cancer: an update of the global impact. Cancer Epidemiol. 2016;41:8–15.
Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA. 2013;309:71–82.
Pantalone KM, Hobbs TM, Chagin KM, Kong SX, Wells BJ, Kattan MW, et al. Prevalence and recognition of obesity and its associated comorbidities: cross-sectional analysis of electronic health record data from a large US integrated health system. BMJ Open. 2017;7:e017583.
Dee A, Kearns K, O’Neill C, Sharp L, Staines A, O’Dwyer V, et al. The direct and indirect costs of both overweight and obesity: a systematic review. BMC Res Notes. 2014;7:242.
Breland JY, Phibbs CS, Hoggatt KJ, Washington DL, Lee J, Haskell S, et al. The obesity epidemic in the Veterans Health Administration: prevalence among key populations of women and men veterans. J Gen Intern Med. 2017;32(Suppl 1):11–17.
Finkelstein EA, Trogdon JG, Cohen JW, Dietz W. Annual medical spending attributable to obesity: payer-and service-specific estimates. Health Aff (Millwood). 2009;28:w822–831.
Biener AI, Decker SL, Agency for Healthcare Research and Quality. Medical care use and expenditures associated with adult obesity in the United States. JAMA. 2018;319:218.
Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011;378:815–25.
Harber MP, Kaminsky LA, Arena R, Blair SN, Franklin BA, Myers J, et al. Impact of cardiorespiratory fitness on all-cause and disease-specific mortality: advances since 2009. Prog Cardiovasc Dis. 2017;60:11–20.
Lear SA, Hu W, Rangarajan S, Gasevic D, Leong D, Iqbal R, et al. The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 high-income, middle-income, and low-income countries: the PURE study. Lancet. 2017;390:2643–54.
Ross R, Blair SN, Arena R, Church TS, Després JP, Franklin BA, et al. Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association. Circulation. 2016;134:e653–99.
Mitchell TL, Gibbons LW, Devers SM, Earnest CP. Effects of cardiorespiratory fitness on healthcare utilization. Med Sci Sports Exerc. 2004;36:2088–92.
Peeters GMEE, Gardine PA, Dobson AJ, Brown WJ. Associations between physical activity, medical costs and hospitalisations in older Australian women: results from the Australian Longitudinal Study on Women´s Health. J Sci Med Sport 2017;21:604–8.
Kennedy AB, Lavie CJ, Blair SN. Fitness or fatness: which is more important? JAMA. 2018;319:231–2.
Kokkinos P, Myers J. Exercise and physical activity: clinical outcomes and applications. Circulation. 2010;122:1637–48.
Bray GA, Frühbeck G, Ryan DH, Wilding JP. Management of obesity. Lancet. 2016;387:1947–56.
Barry VW, Baruth M, Beets MW, Durstine JL, Liu J, Blair SN. Fitness vs. fatness on all-cause mortality: a meta-analysis. Prog Cardiovasc Dis. 2014;56:382–90.
Lee DC, Sui X, Artero EG, Lee IM, Church TS, McAuley PA, et al. Long-term effects of changes in cardiorespiratory fitness and body mass index on all-cause and cardiovascular disease mortality in men: the Aerobics Center Longitudinal Study. Circulation. 2011;124:2483–90.
Shue P, Froelicher VF. EXTRA: an expert system for exercise test reporting. J Non-Invasive. 1998;II-4:21–27.
Myers J, Buchanan N, Walsh D, et al. Comparison of the ramp versus standard exercise protocols. J Am Coll Cardiol. 1991;17:1334–42.
Glass S, Dwyer GB. ACSM’s metabolic equations handbook. Philadelphia: Lippincott, Williams & Wilkins; 2007.
Kokkinos P, Myers J, Franklin B, Narayan P, Lavie CJ, Faselis C. Cardiorespiratory fitness and health outcomes: a call to standardize fitness categories. Mayo Clin Proc. 2018;93:333–6.
U.S. Department of Veterans Affairs. Health Economics Resource Center (HERC). http://www.herc.research.va.gov. Accessed 15 Aug 2018.
Anis AH, Zhang W, Bansback N, Guh DP, Amarsi Z, Birmingham CL. Obesity and overweight in Canada: an updated cost-of-illness study. Obes Rev. 2010;11:31–40.
Buchmueller TC, Johar M. Obesity and health expenditures: evidence from Australia. Econ Hum Biol. 2015;17:42–58.
McAuley PA, Kokkinos PF, Oliveira RB, Emerson BT, Myers JN. Obesity paradox and cardiorespiratory fitness in 12,417 male veterans aged 40 to 70 years. Mayo Clin Proc. 2010;85:115–21.
Myers J, Doom R, King R, Fonda H, Chan K, Kokkinos P, et al. Association between cardiorespiratory fitness and health care costs: The Veterans Exercise Testing Study. Mayo Clin Proc. 2018;93:48–55.
Wang F, McDonald T, Reffitt B, Edington DW. BMI, physical activity, and health care utilization/costs among Medicare retirees. Obes Res. 2005;13:1450–7.
Carlson SA, Fulton JE, Pratt M, Yang Z, Adams EK. Inadequate physical activity and health care expenditures in the United States. Prog Cardiovasc Dis. 2015;57:315–23.
Prince SA, Adamo KB, Hamel ME, et al. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Act. 2008;5:56.
Warner ET, Wolin KY, Duncan DT, Heil DP, Askew S, Bennett GG. Differential accuracy of physical activity self-report by body mass index. Am J Health Behav. 2012;36:168–78.
Weiss JP, Froelicher VF, Myers JN, Heidenreich PA. Health-care costs and exercise capacity. Chest. 2004;126:608–13.
Bachmann JM, DeFina LF, Franzini L, Gao A, Leonard DS, Cooper KH, et al. Cardiorespiratory fitness in middle age and health care costs in later life. J Am Coll Cardiol. 2015;66:1876–85.
Kodama S, Saito K, Tanaka S, Maki M, Yachi Y, Asumi M, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA. 2009;301:2024–35.
Kaminsky LA, Arena R, Myers J. Reference standards for cardiorespiratory fitness measured with cardiopulmonary exercise testing: data from the Fitness Registry and the Importance of Exercise National Database. Mayo Clin Proc. 2015;90:1515–23.
Acknowledgements
Christina Grüne de Souza e Silva was supported by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES)/Programa de Doutorado Sanduíche−88881.136006/2016–01
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
de Souza de Silva, C., Kokkinos, P., Doom, R. et al. Association between cardiorespiratory fitness, obesity, and health care costs: The Veterans Exercise Testing Study. Int J Obes 43, 2225–2232 (2019). https://doi.org/10.1038/s41366-018-0257-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0257-0