Abstract
Objectives
This study aimed to examine the associations between (1) mothers’ preconception body mass index (BMI) trajectories over 6–7 years and offspring childhood BMI, and (2) mothers’ BMI changes between first and second pregnancy and the second-born child’s BMI.
Methods
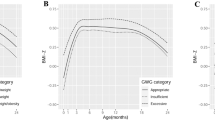
We used data (1606 mothers with 2733 children with mean age 7.7 years, SD 2.9) from the Australian Longitudinal Study on Women’s Health and the Mothers and their Children’s Health study. Preconception BMI trajectories were identified using latent class growth modeling. Children were categorized as underweight, normal, overweight or obese based on age and sex-specific BMI cut-off points for children. Multinomial and binary logistic regression were used for analyses.
Results
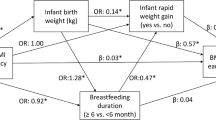
We identified three preconception BMI trajectories, named as ‘normative’ (61.2%), ‘chronically overweight’ (30.7%), and ‘chronically obese’ (8.1%). Children born to ‘chronically overweight’ and ‘chronically obese’ mothers were more likely to be overweight than normal weight relative to children born to women with a ‘normative’ BMI trajectory. The corresponding adjusted relative risk ratios (RRRs) (95% confidence interval [CI]) of childhood overweight were 1.75 (1.33, 2.31) for chronically overweight mothers and 2.48 (1.65, 3.73) for chronically obese mothers. Similarly, we found a much stronger association between ‘chronically overweight’ and ‘chronically obese’ BMI trajectories and childhood risk of obesity; RRR (95% CI), 2.49 (1.41, 4.40) and 6.65 (3.40, 13.01), respectively. Second-born children of mothers with high interpregnancy weight gain (≥4 BMI units) were also at higher risk of being overweight or obese (OR = 2.20, 95% CI: 1.02, 4.75) compared with children of mothers with stable interpregnancy weight (gain or loss of 1 BMI unit or less).
Conclusions
In this population-based prospective cohort study, we found strong dose-response associations between preconception BMI trajectories and offsprings’ childhood BMI.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
World Health Organization. Global database on body mass index: BMI classification 2006. http://www.assessmentpsychology.com/icbmi.htm.
Yu Z, Han S, Zhu J, Sun X, Ji C, Guo X. Pre-pregnancy body mass index in relation to infant birth weight and offspring overweight/obesity: a systematic review and meta-analysis. PLoS ONE. 2013;8:e61627.
Starling AP, Brinton JT, Glueck DH, Shapiro AL, Harrod CS, Lynch AM, et al. Associations of maternal BMI and gestational weight gain with neonatal adiposity in the Healthy Start study. Am J Clin Nutr. 2015;101:302–9.
Castillo-Laura H, Santos IS, Quadros LC, Matijasevich A. Maternal obesity and offspring body composition by indirect methods: a systematic review and meta-analysis. Cad De Saude Publica. 2015;31:2073–92.
Catalano PM, Farrell K, Thomas A, Huston-Presley L, Mencin P, de Mouzon SH, et al. Perinatal risk factors for childhood obesity and metabolic dysregulation. Am J Clin Nutr. 2009;90:1303–13.
Lawlor DA, Smith GD, O’Callaghan M, Alati R, Mamun AA, Williams GM, et al. Epidemiologic evidence for the fetal overnutrition hypothesis: findings from the mater-university study of pregnancy and its outcomes. Am J Epidemiol. 2007;165:418–24.
Linabery AM, Nahhas RW, Johnson W, Choh AC, Towne B, Odegaard AO, et al. Stronger influence of maternal than paternal obesity on infant and early childhood body mass index: the Fels Longitudinal Study. Pediatr Obes. 2013;8:159–69.
Lawlor DA, Timpson NJ, Harbord RM, Leary S, Ness A, McCarthy MI, et al. Exploring the developmental overnutrition hypothesis using parental-offspring associations and FTO as an instrumental variable. PLoS Med. 2008;5:e33.
Li L, Law C, Lo Conte R, Power C. Intergenerational influences on childhood body mass index: the effect of parental body mass index trajectories. Am J Clin Nutr. 2009;89:551–7.
Jacota M, Forhan A, Saldanha-Gomes C, Charles MA, Heude B. Maternal weight prior and during pregnancy and offspring’s BMI and adiposity at 5-6 years in the EDEN mother-child cohort. Pediatr Obes. 2017;12:320–9.
Zhang S, Rattanatray L, Morrison JL, Nicholas LM, Lie S, McMillen IC. Maternal obesity and the early origins of childhood obesity: weighing up the benefits and costs of maternal weight loss in the periconceptional period for the offspring. Exp Diabetes Res. 2011;2011:585749.
Bogaerts A, Van den Bergh BR, Ameye L, Witters I, Martens E, Timmerman D, et al. Interpregnancy weight change and risk for adverse perinatal outcome. Obstet Gynecol. 2013;122:999–1009.
Persson M, Johansson S, Cnattingius S. Inter-pregnancy weight change and risks of severe birth-asphyxia-related outcomes in singleton infants born at term: a Nationwide Swedish Cohort Study. PLoS Med. 2016;13:e1002033.
Dobson AJ, Hockey R, Brown WJ, Byles JE, Loxton DJ, McLaughlin D, et al. Cohort profile update: Australian Longitudinal Study on Women’s Health. Int J Epidemiol. 2015;44:1547,1547a–1547f.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–3.
Department of Health and Aged Care (GISCA). Measuring remoteness: accessibility/remoteness index of Australia (ARIA): Revised Ed. In. Canberra, 2001.
Brown WJ, Ford JH, Burton NW, Marshall AL, Dobson AJ. Prospective study of physical activity and depressive symptoms in middle-aged women. Am J Prev Med. 2005;29:265–72.
Moraeus L, Lissner L, Yngve A, Poortvliet E, Al-Ansari U, Sjoberg A. Multi-level influences on childhood obesity in Sweden: societal factors, parental determinants and child’s lifestyle. Int J Obes (Lond). 2012;36:969–76.
Cameron AJ, Spence AC, Laws R, Hesketh KD, Lioret S, Campbell KJ. A review of the relationship between socioeconomic position and the early-life predictors of obesity. Curr Obes Rep. 2015;4:350–62.
Andruff H, Carraro N, Thompson A, Gaudreau P. Latent class growth modelling: a tutorial. Tutor Quant Methods Psychol. 2009;5:11–24.
Jones BL, Nagin DS. Advances in group-based trajectory modeling and an SAS procedure for estimating them. Sociol Methods Res. 2007;35:542–71.
Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6:109–38.
Ostbye T, Malhotra R, Landerman LR. Body mass trajectories through adulthood: results from the National Longitudinal Survey of Youth 1979 Cohort (1981-2006). Int J Epidemiol. 2011;40:240–50.
SAS Institute Inc. SAS/IML® 14.1 User’s Guide. Cary, NC: SAS Institute Inc.; 2015.
StataCorp. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP; 2015.
Muhlhausler BS, Ong ZY. The fetal origins of obesity: early origins of altered food intake. Endocr Metab Immune Disord Drug Targets. 2011;11:189–97.
Jaaskelainen A, Pussinen J, Nuutinen O, Schwab U, Pirkola J, Kolehmainen M, et al. Intergenerational transmission of overweight among Finnish adolescents and their parents: a 16-year follow-up study. Int J Obes (Lond). 2011;35:1289–94.
Campbell MK. Biological, environmental, and social influences on childhood obesity. Pediatr Res. 2016;79:205–11.
Kral TV, Rauh EM. Eating behaviors of children in the context of their family environment. Physiol Behav. 2010;100:567–73.
Kral JG, Biron S, Simard S, Hould FS, Lebel S, Marceau S, et al. Large maternal weight loss from obesity surgery prevents transmission of obesity to children who were followed for 2 to 18 years. Pediatrics. 2006;118:e1644–9.
Lundahl A, Kidwell KM, Nelson TD. Parental underestimates of child weight: a meta-analysis. Pediatrics. 2014;133:e689–703.
Tie HT, Xia YY, Zeng YS, Zhang Y, Dai CL, Guo JJ, et al. Risk of childhood overweight or obesity associated with excessive weight gain during pregnancy: a meta-analysis. Arch Gynecol Obstet. 2014;289:247–57.
Poston L, Caleyachetty R, Cnattingius S, Corvalan C, Uauy R, Herring S, et al. Preconceptional and maternal obesity: epidemiology and health consequences. Lancet Diabetes Endocrinol. 2016;4:1025–36.
Organisation for Economic Co-operation and Development. Obesity Update. 2014; http://www.oecd.org/health/Obesity-Update-2014.pdf.
Hanson M, Barker M, Dodd JM, Kumanyika S, Norris S, Steegers E, et al. Interventions to prevent maternal obesity before conception, during pregnancy, and post partum. Lancet Diabetes Endocrinol. 2017;5:65–76.
Acknowledgements
The research on which this paper is based was conducted as part of the Australian Longitudinal Study on Women’s Health by the University of Queensland and the University of Newcastle. We are grateful to the Australian Government Department of Health for funding and to the women who provided the survey data. AAA supported by International Postgraduate Research Scholarship (IPRS) and UQ Centennial scholarship. The MatCH study is funded by the National Health and Medical Research Council (NHMRC) (APP1059550) and GDM holds NHMRC Principal Research Fellowship (APP1121844).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
41366_2018_78_MOESM1_ESM.docx
The association between preconception BMI trajectories and offsprings’ childhood BMI after excluding children born to women with GDM and /or HDP (n = 2 483)
41366_2018_78_MOESM2_ESM.docx
The association between preconception BMI trajectories and offsprings’ childhood BMI (sample restricted to the first births, n = 1 156)
Rights and permissions
About this article
Cite this article
Adane, A.A., Dobson, A., Tooth, L. et al. Maternal preconception weight trajectories are associated with offsprings’ childhood obesity. Int J Obes 42, 1265–1274 (2018). https://doi.org/10.1038/s41366-018-0078-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0078-1
This article is cited by
-
Barriers and facilitators for sustainable weight loss in the pre-conception period among Danish women with overweight or obesity – a qualitative study
BMC Public Health (2023)
-
Distribution and association of interpregnancy weight change with subsequent pregnancy outcomes in Asian women
Scientific Reports (2023)
-
Interpregnancy weight gain and childhood obesity: analysis of a UK population-based cohort
International Journal of Obesity (2022)
-
Cohort profile: Singapore Preconception Study of Long-Term Maternal and Child Outcomes (S-PRESTO)
European Journal of Epidemiology (2021)