Abstract
Introduction
In obese individuals, nonalcoholic fatty liver disease (NAFLD) is common but often goes undiagnosed, and therefore untreated. The presence of significant fibrosis is a key determinant of NAFLD progression, and liver steatosis has substantial cardiovascular implications. We aimed to determine the diagnostic accuracy of common noninvasive diagnostic tests for steatosis and fibrosis in the obese.
Methods
We recruited 182 severely and morbidly obese individuals undergoing bariatric surgery (age 44 ± 12 years, body mass index 45.1 ± 8.3 kg/m2). Medical history, blood tests and liver biopsy were taken on the day of surgery. Serum steatosis and fibrosis scores were calculated. In a subgroup of patients, transient elastography with controlled attenuation parameter (TE/CAP) (n = 82) and proton magnetic resonance spectroscopy (1H-MRS) (n = 49) were performed.
Results
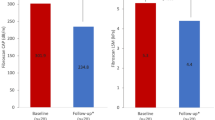
1H-MRS had excellent diagnostic accuracy for steatosis, with strong correlation to steatosis (r = 0.647, p < 0.001), good AUROC (0.852, p = 0.001), sensitivity (81.3%) and specificity (87.5%). However, due to low feasibility in this cohort (65.3% success), this was substantially decreased with intention-to-diagnose analysis (sensitivity 50.0%, specificity 60.9%). CAP had good feasibility (80.5%), and performed better in intention-to-diagnose analysis (AUROC 0.688, sensitivity 84.8%, specificity 47.2%). Serum steatosis scores performed poorly, with comparable accuracy to ALT. For significant fibrosis, TE had the best accuracy (AUROC 0.903, p = 0.007), which remained reasonable after intention-to-diagnose analysis (sensitivity 100%, specificity 59.0%). A combination approach using CAP with ALT for steatosis and TE with Forn index for fibrosis yielded reasonable overall accuracy.
Conclusions
1H-MRS and TE/CAP had greatest accuracy for NAFLD-related steatosis and fibrosis. Failure rates in obesity significantly diminished diagnostic ability. Use of a combination of serum and imaging tests improved overall feasibility of assessment and diagnostic accuracy in obese individuals.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Vernon G, Baranova A, Younossi ZM. Systematic review: The epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther. 2011;34:274–85.
Williams KH, Shackel NA, Gorrell MD, McLennan SV, Twigg SM. Diabetes and nonalcoholic fatty liver disease: A pathogenic duo. Endocr Rev. 2013;34:84–129.
Goodman ZD. The impact of obesity on liver histology. Clin Liver Dis. 2014;18:33–40.
Ekstedt M, Hagström H, Nasr P, Fredrikson M, Stål P, Kechagias S, et al. Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology. 2015;61:1547–54.
Angulo P, Kleiner DE, Dam-Larsen S, Adams L, Bjornsson ES, Charatcharoenwitthaya P, et al. Liver fibrosis, but no other histologic features, is associated with long-term outcomes of patients with nonalcoholic fatty liver disease. Gastroenterology. 2015;149:389–97.
Byrne C, Targher G. NAFLD: A multisystem disease. J Hepatol. 2015;62:S47–S64.
Yki-Jarvinen H. Non-alcoholic fatty liver disease as a cause and a consequence of metabolic syndrome. Lancet Diabetes Endocrinol. 2014;2:901–10.
Targher G, Byrne CD. A perspective on metabolic syndrome and nonalcoholic fatty liver disease. Metab Syndr Relat Disord. 2015;13:235–8.
Manchanayake J, Chitturi S, Nolan C, Farrell GC. Postprandial hyperinsulinemia is universal in non-diabetic patients with nonalcoholic fatty liver disease. J Gastroenterol Hepatol. 2011;26:510–6.
Anstee Q, Targher G, Day CP. Progression of NAFLD to diabetes mellitus, cardiovascular disease or cirrhosis. Nat Rev Gastroenterol Hepatol. 2013;10:330–44.
Taitano AA, Markow M, Fiana JE, Wheeler DE, Gonzalvo JP, Murr MM. Bariatric surgery improves histological features of nonalcoholic fatty liver disease and liver fibrosis. J Gastrointest Surg. 2014;19:429–36.
Lassailly G, Caiazzo R, Buob D, Pigeyre M, Verkindt H, Labreuche J, et al. Bariatric surgery reduces features of nonalcoholic steatohepatitis in morbidly obese patients. Gastroenterology. 2015;149:379–88.
Rockey DC, Caldwell SH, Goodman ZD, Nelson RC, Smith AD. Liver biopsy - AASLD Position Paper. Hepatology. 2009;49:1017–44.
Castera L. Noninvasive evaluation of nonalcoholic fatty liver disease. Semin Liver Dis. 2015;35:291–303.
Asrani SK. Incorporation of non-invasive measures of liver fibrosis into clinical practice: diagnosis and prognosis. Clin Gastroenterol Hepatol. 2015;13:2190–204.
Rosen ED, Spiegelman BM. What we talk about when we talk about fat. Cell. 2014;156:20–44.
Uppot RN, Shahani DV, Hahn PF, Gervais D, Mueller PR. Impact of obesity on medical imaging and image-guided intervention. Am J Roentgenol. 2007;188:433–40.
Prati D, Taioli E, Zanella A, Torre ED, Butelli S, Vecchio ED, et al. Updated definitions of healthy ranges for serum alanine aminotransferase levels. Ann Intern Med. 2002;137:1–10.
Ratziu V, Bellentani S, Cortez-Pinto H, Day C, Marchesini G. A position statement on NAFLD/NASH based on the EASL 2009 special conference. J Hepatol. 2010;53:372–84.
Brunt EM, Kleiner DE, Wilson LA, Belt P, Neuschwander-Tetri BA. Nonalcoholic fatty liver disease (NAFLD) activity score and the histopathologic diagnosis in NAFLD: Distinct clinicopathologic meanings. Hepatology. 2010;53:810–20.
Kleiner DE, Brunt EM, Van Natta M, Behling C, Contos MJ, Cummings OW, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–21.
Kwok R, Tse YK, Wong GL, Ha Y, Lee AU, Ngu MC, et al. Systematic review with meta-analysis: non-invasive assessment of non-alcoholic fatty liver disease: the role of transient elastography and plasma cytokeratin-18 fragments. Aliment Pharmacol Ther. 2014;39:254–69.
Johnson NA, Walton DW, Sachinwalla T, Thompson CH, Smith K, Ruell PA, et al. Noninvasive assessment of hepatic lipid composition: Advancing understanding and management of fatty liver disorders. Hepatology. 2008;47:1513–23.
Keating SE, Hackett DA, Parker HM, O’Connor HT, Gerofi JA, Sainsbury A, et al. Effect of aerobic exercise training dose on liver fat and visceral adiposity. J Hepatol. 2015;63:174–82.
Fedchuk L, Nascimbeni F, Pais R, Charlotte F, Housset C, Ratziu V, et al. Performance and limitations of steatosis biomarkers in patients with nonalcoholic fatty liver disease. Aliment Pharmacol Ther. 2014;40:1209–22.
Oni ET, Agatston AS, Blaha MJ, Fialkow J, Cury R, Sposito A, et al. A systematic review: Burden and severity of subclinial cardiovascular disease among those with nonalcoholic fatty liver; Should we care? Atherosclerosis. 2013;230:258–67.
Hamirani YS, Pandey S, Rivera JJ, Ndumele C, Budoff MJ, Blumenthal RS, et al. Markers of inflammation and coronary artery calcification: a systematic review. Atherosclerosis. 2008;201:1–7.
Cobble M, Bale B. Carotid intima-media thickness: knowledge and application to everyday practice. Postgrad Med. 2010;122:10–18.
Schwenzer NF, Springer F, Schraml C, Stefan N, Machann J, Schick F. Non-invasive assessment and quantification of liver steatosis by ultrasound, computed tomography and magnetic resonance. J Hepatol. 2009;51:433–45.
Naveau S, Lamouri K, Pourcher G, Njike-Nakseu M, Ferretti S, Courie R, et al. The diagnostic accuracy of transient elastography for the diagnosis of liver fibrosis in bariatric surgery candidates with suspected NAFLD. Obes Surg. 2014;24:1693–701.
Myers RP, Pomier-Layrargues G, Kirsch R, Pollett A, Duarte-Rojo A, Wong D, et al. Feasibility and diagnostic performance of the FibroScan XL probe for liver stiffness measurement in overweight and obese patients. Hepatology. 2012;55:199–208.
Myers RP, Pomier-Layrargues G, Kirsch R, et al. Feasibility and diagnostic performance of the FibroScan XL probe for liver stiffness measurement in overweight and obese patients. Hepatology. 2012;55:199–208.
Boursier J, Vergniol J, Guillet A, Hiriart JB, Lannes A, Le Bail B, et al. Diagnostic accuracy and prognostic significance of blood fibrosis tests and liver stiffness measurement by Fibroscan in nonalcoholic fatty liver disease. J Hepatol. 2016;65:570–8.
Chavez-Tapia NC, Tellez-Avila FI, Barrientos-Gutierrez T, Mendez-Sanchez N, Lizardi-Cervera J, Uribe M. Bariatric surgery for non-alcoholic steatohepatitis in obese patients. Cochrane Database Sys Rev. 2010: CD007340.
Bower G, Toma T, Harling L, Jiao LR, Efthimiou E, Darzi A, et al. Bariatric surgery and non-alcoholic fatty liver disease: a systematic review of liver biochemistry and histology. Obes Surg. 2015;25:2280–9.
National Institute of Health and Care Excellence. Non-alcoholic fatty liver disease: assessment and management of non-alcoholic fatty liver disease (NAFLD) in adults, children and young people. In: NICE guideline—methods, evidence and recommendations. National Institute for Health and Care Excellence; London, UK, 2015.
Kemp W, Roberts SK. FibroScan and transient elastography. Aust Fam Physician. 2013;42:468–71.
Bellentani S, Marino M. Epidemiology and natural history of non-alcoholic fatty liver disease (NAFLD). Ann Hepatol. 2009;8:Suppl 4–Suppl 8.
Teixeira AR, Bellodi-Privato M, Carvalheira JB, Pilla VF, Pareja JC, D’Albuquerque LA. The incapacity of the surgeon to identify NASH in bariatric surgery makes biopsy mandatory. Obes Surg. 2009;19:1678–84.
Lassailly G, Caiazzo R, Hollebecque A, Buob D, Leteurtre E, Arnalsteen L, et al. Validation of noninvasive biomarkers (FibroTest, SteatoTest, and NashTest) for prediction of liver injury in patients with morbid obesity. Eur J Gastroenterol Hepatol. 2011;23:499–506.
Francque SMA, Verrijken A, Mertens I, Hubens G, Van Marck E, Pelckmans P, et al. Noninvasive assessment of nonalcoholic fatty liver disease in obese or overweight patients. Clin Gastroenterol Hepatol. 2012;10:1162–8.
Ooi GJ, Burton PR, Doyle L, Wentworth JM, Bhathal PS, Sikaris K, et al. Effects of bariatric surgery on liver function tests in patients with nonalcoholic fatty liver disease. Obes Surg. 2016;27:1533.
Author contributions:
All listed authors have contributed to and agree upon the content of the final manuscript. All authors contributed to study conception, design and data acquisition. GO, PB, NJ and AE performed the data analyses. GO, PB and WB drafted the initial version of the manuscript. All authors critically revised and redrafted the manuscript, and all authors approve the final version.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
GO, PB, CL and WB report being affiliated with the Centre for Obesity Research and Education. The Centre has received funding for research purposes from Allergan and Apollo Endosurgery, the manufacturers of the LapBand™. The grant is not tied to any specific research project, and neither Allergan nor Apollo Endosurgery have control of the protocol, analysis and reporting of any studies. The Centre also receives a grant from Applied Medical towards educational programs. WB reports financial support for a bariatric surgery registry from the Commonwealth of Australia, Apollo Endosurgery, Covidien, Johnson and Johnson, Gore and Applied Medical; and a speaker’s honorarium from Merck Sharpe and Dohme. These are outside of the submitted work. NJ reports speaker’s honorarium from Merck Sharpe & Dohme, which is outside of the submitted work. GO reports scholarships from the National Health and Medical Research Council and the Royal Australasian College of Surgeons. WK, AE, AM, CM, SR have no other disclosures or conflicts of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Ooi, G.J., Earnest, A., Kemp, W.W. et al. Evaluating feasibility and accuracy of non-invasive tests for nonalcoholic fatty liver disease in severe and morbid obesity. Int J Obes 42, 1900–1911 (2018). https://doi.org/10.1038/s41366-018-0007-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0007-3
This article is cited by
-
Compare the Combined Diagnostic Accuracy of Transient Elastography and Visual Liver Score in Assessing Non-Alcoholic Fatty Liver Disease (NAFLD) and Compare it with Liver Biopsy in Morbidly Obese Patients Undergoing Bariatric Surgery: An Observational Study
Obesity Surgery (2024)
-
Performance of Serum-Based Scores for Identification of Mild Hepatic Steatosis in HBV Mono-infected and HBV–HIV Co-infected Adults
Digestive Diseases and Sciences (2022)
-
Higher cut-off values of non-invasive methods might be needed to detect moderate-to-severe steatosis in morbid obese patients: a pilot study
Scientific Reports (2020)
-
Noninvasive assessment of hepatic steatosis and fibrosis in patients with severe obesity
Endocrine (2020)
-
Measurement of Liver Stiffness with 2D-Shear Wave Elastography (2D-SWE) in Bariatric Surgery Candidates Reveals Acceptable Diagnostic Yield Compared to Liver Biopsy
Obesity Surgery (2019)