Abstract
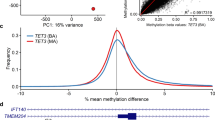
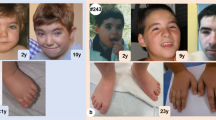
The search for aetiology of Mendelian disorders is traditionally based on the observation of clinical phenotypes and molecular screening of associated genes. However, a disease-specific diagnosis can be challenging. In this study we detail how the combinatorial genomic and epigenomic assessment allowed to find the underlying molecular event of a clinical case that remained misdiagnosed for years. The individual was referred as affected by an atypical form of Kabuki syndrome with a variant of uncertain significance in the KMT2D gene. However, significant inconsistencies with this diagnosis emerged upon familial segregation of the variant and after the clinical re-evaluation. Therefore, we applied an epigenomic strategy by studying the DNA methylation profile which resulted not consistent with the Kabuki syndrome episignature or with any other disorder-specific episignature described so far, providing strong evidence that the Kabuki syndrome diagnosis does not apply. This result led us to further investigate for epigenetic machinery diseases by using a multigene panel for chromatinopathies. Since this analysis yielded negative results, we applied a whole exome sequencing and identified a de novo pathogenic variant in the CTNNB1 gene associated to NEDSDV syndrome, a neurodevelopmental disorder characterized by intellectual disability and craniofacial anomalies. Based on molecular results and the updated clinical features, we confirmed the NEDSDV diagnosis. Our findings show that the combination of genomic and epigenomics strategies, along with a deeper analysis of clinical phenotype, may provide a significant improvement in the diagnostic protocols for rare genetic disorders and help resolve long-time misdiagnosed and unsolved case.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Petersen BS, Fredrich B, Hoeppner MP, Ellinghaus D, Franke A. Opportunities and challenges of whole-genome and -exome sequencing. BMC Genet. 2017;18:14.
Haghshenas S, Bhai P, Aref-Eshghi E, Sadikovic B. Diagnostic Utility of Genome-Wide DNA Methylation Analysis in Mendelian Neurodevelopmental Disorders. Int J Mol Sci. 2020;21:9303.
Kerkhof J, Squeo GM, McConkey H, Levy MA, Piemontese MR, Castori M, et al. DNA methylation episignature testing improves molecular diagnosis of Mendelian chromatinopathies. Genet Med. 2022;24:51–60.
Levy MA, McConkey H, Kerkhof J, Barat-Houari M, Bargiacchi S, Biamino E, et al. Novel diagnostic DNA methylation episignatures expand and refine the epigenetic landscapes of Mendelian disorders. HGG Adv. 2022;3:100075.
Sadikovic B, Aref-Eshghi E, Levy MA, Rodenhiser D. DNA methylation signatures in mendelian developmental disorders as a diagnostic bridge between genotype and phenotype. Epigenomics 2019;11:563–75.
Sadikovic B, Levy MA, Aref-Eshghi E. Functional annotation of genomic variation: DNA methylation episignatures in neurodevelopmental Mendelian disorders. Hum Mol Genet. 2020;29:R27–R32.
Sadikovic B, Levy MA, Kerkhof J, Aref-Eshghi E, Schenkel L, Stuart A, et al. Correction: Clinical epigenomics: genome-wide DNA methylation analysis for the diagnosis of Mendelian disorders. Genet Med. 2021;23:2228.
Priolo M, Micale L, Augello B, Fusco C, Zucchetti F, Prontera P, et al. Absence of deletion and duplication of MLL2 and KDM6A genes in a large cohort of patients with Kabuki syndrome. Mol Genet Metab. 2012;107:627–9.
Squeo GM, Augello B, Massa V, Milani D, Colombo EA, Mazza T, et al. Customised next-generation sequencing multigene panel to screen a large cohort of individuals with chromatin-related disorder. J Med Genet. 2020;57:760–8.
Alfaiz AA, Micale L, Mandriani B, Augello B, Pellico MT, Chrast J, et al. TBC1D7 mutations are associated with intellectual disability, macrocrania, patellar dislocation, and celiac disease. Hum Mutat. 2014;35:447–51.
Lodder EM, De Nittis P, Koopman CD, Wiszniewski W, Moura de Souza CF, Lahrouchi N, et al. GNB5 Mutations Cause an Autosomal-Recessive Multisystem Syndrome with Sinus Bradycardia and Cognitive Disability. Am J Hum Genet. 2016;99:704–10.
den Dunnen JT, Dalgleish R, Maglott DR, Hart RK, Greenblatt MS, McGowan-Jordan J, et al. HGVS Recommendations for the Description of Sequence Variants: 2016 Update. Hum Mutat. 2016;37:564–9.
Biesecker LG, Harrison SM. The ACMG/AMP reputable source criteria for the interpretation of sequence variants. Genet Med. 2018;20:1687–8.
Cocciadiferro D, Augello B, De Nittis P, Zhang J, Mandriani B, Malerba N, et al. Dissecting KMT2D missense mutations in Kabuki syndrome patients. Hum Mol Genet. 2018;27:3651–68.
Micale L, Augello B, Fusco C, Selicorni A, Loviglio MN, Silengo MC, et al. Mutation spectrum of MLL2 in a cohort of Kabuki syndrome patients. Orphanet J Rare Dis. 2011;6:38.
Sadikovic B, Levy MA, Kerkhof J, Aref-Eshghi E, Schenkel L, Stuart A, et al. Clinical epigenomics: genome-wide DNA methylation analysis for the diagnosis of Mendelian disorders. Genet Med. 2021;23:1065–74.
Kopanos C, Tsiolkas V, Kouris A, Chapple CE, Albarca Aguilera M, Meyer R, et al. VarSome: the human genomic variant search engine. Bioinformatics 2019;35:1978–80.
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–24.
Aref-Eshghi E, Bourque DK, Kerkhof J, Carere DA, Ainsworth P, Sadikovic B, et al. Genome-wide DNA methylation and RNA analyses enable reclassification of two variants of uncertain significance in a patient with clinical Kabuki syndrome. Hum Mutat. 2019;40:1684–9.
Xing Y, Takemaru K, Liu J, Berndt JD, Zheng JJ, Moon RT, et al. Crystal structure of a full-length beta-catenin. Structure 2008;16:478–87.
MacDonald BT, Tamai K, He X. Wnt/beta-catenin signaling: components, mechanisms, and diseases. Dev Cell. 2009;17:9–26.
Dong F, Jiang J, McSweeney C, Zou D, Liu L, Mao Y. Deletion of CTNNB1 in inhibitory circuitry contributes to autism-associated behavioral defects. Hum Mol Genet. 2016;25:2738–51.
Brault V, Moore R, Kutsch S, Ishibashi M, Rowitch DH, McMahon AP, et al. Inactivation of the beta-catenin gene by Wnt1-Cre-mediated deletion results in dramatic brain malformation and failure of craniofacial development. Development 2001;128:1253–64.
Huelsken J, Vogel R, Erdmann B, Cotsarelis G, Birchmeier W. beta-Catenin controls hair follicle morphogenesis and stem cell differentiation in the skin. Cell 2001;105:533–45.
Kuechler A, Willemsen MH, Albrecht B, Bacino CA, Bartholomew DW, van Bokhoven H, et al. De novo mutations in beta-catenin (CTNNB1) appear to be a frequent cause of intellectual disability: expanding the mutational and clinical spectrum. Hum Genet. 2015;134:97–109.
Tucci V, Kleefstra T, Hardy A, Heise I, Maggi S, Willemsen MH, et al. Dominant beta-catenin mutations cause intellectual disability with recognizable syndromic features. J Clin Investig. 2014;124:1468–82.
Kharbanda M, Pilz DT, Tomkins S, Chandler K, Saggar A, Fryer A, et al. Clinical features associated with CTNNB1 de novo loss of function mutations in ten individuals. Eur J Med Genet. 2017;60:130–5.
Ke Z, Chen Y. Case Report: A de novo CTNNB1 Nonsense Mutation Associated With Neurodevelopmental Disorder, Retinal Detachment, Polydactyly. Front Pediatr. 2020;8:575673.
Dubruc E, Putoux A, Labalme A, Rougeot C, Sanlaville D, Edery P. A new intellectual disability syndrome caused by CTNNB1 haploinsufficiency. Am J Med Genet A. 2014;164a:1571–5.
Aref-Eshghi E, Bend EG, Colaiacovo S, Caudle M, Chakrabarti R, Napier M, et al. Diagnostic Utility of Genome-wide DNA Methylation Testing in Genetically Unsolved Individuals with Suspected Hereditary Conditions. Am J Hum Genet. 2019;104:685–700.
Acknowledgements
We are grateful to the patient and parents for their cooperation in this study and for giving consent to publish data and photographs. Funding for this study was provided by Telethon - Italy (Grant no. GGP13231), Italian Ministry of Health, Jerome Lejeune Foundation, Daunia Plast to GM; by the London Health Sciences Molecular Diagnostics Development Fund and Genome Canada Genomic Applications Partnership Program Grant (Beyond Genomics: Assessing the Improvement in Diagnosis of Rare Diseases using Clinical Epigenomics in Canada, EpiSign-CAN) awarded to BS. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the paper.
Author information
Authors and Affiliations
Contributions
Conceptualization: AP, GM, GMS. Investigation and Methodology: AP, ED, EC, JK; Data curation and formal analysis: JK, HMC, BS, TM, SC; Patients and clinical follow-up: LS, MCD; Writing—original draft: AP, MCD, GM; Writing-review & editing: AP, MCD, BS, JK, GMS, HMC, TM, GM. Funding acquisition: GM, BS. All authors have read and agreed to the published version of the paper. The corresponding author has had full access to the data in the study and final responsibility for the decision to submit for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
Written informed consent was obtained from the mother of the child for the publication of any potentially identifiable images included in this paper.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Paparella, A., Squeo, G.M., Di Venere, E. et al. Genome-wide DNA methylation profiling and exome sequencing resolved a long-time misdiagnosed case. J Hum Genet 67, 547–551 (2022). https://doi.org/10.1038/s10038-022-01043-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s10038-022-01043-y