Abstract
Background:
Congenital heart diseases (CHDs) are often associated with other congenital anomalies, dysmorphic features, and developmental delay, and only a few cases of chromosomal abnormalities are detected by conventional cytogenetic techniques. The microarray comparative genomic hybridization (CGH) analysis allows the identification of submicroscopic genomic rearrangements.
Methods:
During the past 3 y, 55 of 330 patients referred for array CGH had CHD of unknown etiology plus at least one additional indication of abnormal chromosomal phenotype. High-resolution 1 × 244K or 4 × 180K Agilent arrays were used in this study (average resolution 7–13 kb).
Results:
Copy-number variations were detected in 37 of 55 patients, and in 29 of 37 patients there were genes that have been associated with CHD. All 37 patients had at least one additional phenotypic abnormality: 30 of 37 had one or more other congenital anomalies, 23 of 37 had dysmorphic features, 16 of 37 had intellectual disability, 13 of 37 had abnormal magnetic resonance imaging, 10 of 37 had hypotonia, and 7 of 37 had seizures. In 9 of 55 patients, unexpected genomic rearrangements in relation to their phenotype were identified.
Conclusion:
In patients with CHD and at least one additional indication of abnormal chromosomal phenotype, array CGH analysis could detect possible submicroscopic chromosomal abnormalities and provide proper genetic counseling.
Similar content being viewed by others
Main
Congenital heart disease (CHD), with a frequency of 19 to 75 in 1,000 births, is a major cause of childhood morbidity and mortality worldwide (1). Recent advances in medical and surgical management have resulted in 85% of affected children surviving to adulthood (2). Classic studies, including the Baltimore–Washington Infant Study, have shown that CHD is multifactorial/complex in nature because of both genetic predisposition and environmental factors (3).
Chromosomal abnormalities are a common cause of CHD, but conventional cytogenetic techniques (G-banded karyotype) are able to detect imbalances 5–10 Mb in size. Submicroscopic aberrations can be detected using more recent genetic diagnostic methodologies such as high-resolution comparative genomic hybridization (CGH) technology, which can also identify copies of DNA, called copy-number variations (CNVs). A CNV is defined as a chromosomal region of at least 1 kb in size that differs in copy number compared with the reference human genome. The CNV can be a benign variation (without clinical significance), or it could have unclear clinical significance or be pathogenic. For clinical relevance, the CNV must be categorized as benign, of unclear significance, or pathogenic, thus contributing to the patient’s phenotype. To further interpret the nature of the CNV, the qualifier copy-number loss (deletion) or copy-number gain (duplication) should also be included. Microdeletions or microduplications, which are clinically significant genomic rearrangements, have been identified in patients with intellectual disability/developmental delay and/or multiple congenital anomalies, with otherwise normal conventional karyotype (4). The main advantage of array CGH is its ability to detect any quantitative changes in DNA; it is 10–10,000-fold more detailed than conventional karyotype, depending on the size of the target and the coverage and density of probes in the array (5). This study describes the application of array CGH to detect submicroscopic genomic rearrangement in children with CHD and syndromic features.
Results
Of the 55 patients with CHD who were examined by array CGH, large genomic rearrangements (CNVs) were detected in 37 patients (67%) (20 males/17 females). In 23 patients, more than 1 CNV was detected, and in total, 77 deletions and 22 duplications were identified, ranging in size from 0.08 to 19.01 Mb ( Table 1 ). The types of heart defect in each of the 37 patients with a pathogenic CNV detected are shown in Table 1 . The assignment of CNVs pathogenicity was based on the gene content according to the University of California Santa Cruz Genome Browser database (http://genome.ucsc.edu/) human genome build 18 or 19 (6). In addition, these patients presented with the following: 30 of 37 had one or more other congenital anomalies, 23 of 37 had dysmorphic features, 16 of 37 had intellectual disability, 16 of 37 had other anomalies, 13 of 37 had abnormal magnetic resonance imaging, 10 of 37 had hypotonia, and 7 of 37 had seizures. Array CGH performed on parental DNA for 5 patients, indicated that the genomic rearrangement was of maternal origin in 2 and de novo in the remaining 3.
Discussion
In this study, using array CGH, we examined 55 patients with CHD and at least one of the following conditions: other congenital anomalies, dysmorphic features, or developmental delay. CNVs were detected in 37 of 55 patients (67%). In 29 of 37 patients, CHD was attributed to genes identified in specific genomic regions that are considered to be associated with heart disease. In the remaining 8 patients, the CNVs identified did not include known genes associated with heart disease ( Table 1 ).
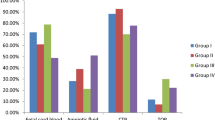
The overall clinical phenotype in 23 of 55 patients resulted from a combination of several CNVs. In 14 patients, we identified known microdeletion and microduplication syndromes: DiGeorge (3), 1p36 microdeletion (3), 9q subtelomeric microduplication (3), Williams syndrome (2), CHARGE (Coloboma of the eye, Heart defects, Atresia of the choanae, Retardation of growth and/or development, Genital defect, Ear anomalies and/or deafness) (1), 17q21–31 microduplication (1), and Jacobsen syndrome (1) ( Figure 1 ). In general, it is given that phenotypes of microduplications are milder as compared with those caused by microdeletions in the same chromosomal region; this was confirmed by our cases and previously published results (6).
It is interesting that unexpected genomic rearrangements in relation to their phenotype were identified in nine patients. Specifically, two patients showed CNVs involving the genes KCNQ1 and CACNB2 (patients 34 and 38), which are associated with long QT and Brugada syndrome, respectively (7,8), whereas in the remaining seven patients (patients 4, 9, 18, 23, 28, 36, and 37) ( Table 1 ) the identified CNVs were associated with channelopathies (9). Genetic counseling proves problematic in cases where the CNVs include ion channel genes because it is not certain that they will lead to a late-onset severe cardiac disease.
Most studies of a similar nature rely on determining whether the finding is de novo before assigning pathogenicity. Among the limited parental tests performed, in two instances where the CNVs were of maternal origin the maternal phenotype was normal. We acknowledge the paucity of parental testing as a weakness of our study, but because the array CGH test is expensive and is not covered by the Greek National Health Insurance system, the remaining parents refused testing.
The current study indentified the genes relating to CHD in 78% of patients with array CGH. The higher percentage of patients containing CNVs with genes relating to CHD in this study as compared with two previously published studies is probably a result of the different number of patients studied and the higher array CGH resolution (10,11).
Thienpont et al. (10) were the first to study array CGH techniques in patients with CHD and other congenital anomalies and normal conventional karyotype. In their study of 60 patients, CNVs were detected in 30% of cases, whereas in 17% some CNVs were located in genomic regions containing genes contributing substantially to the development of the heart, such as NKX2.5 and NOTCH1. However, in most of the genomic aberrations, the genes identified were not associated with CHD.
One year later, Richards et al. (11) investigated 40 patients (20 with isolated CHD and 20 with additional congenital anomalies and/or developmental delay) using array CGH. CNVs were detected in 5 of 20 children (25%) with CHD and additional congenital anomalies, whereas no CNVs were found in the remaining 20 children with isolated CHD.
Recently, Sørensen et al. (12) examined 402 CHD patients (378 with isolated CHD and 24 with extra cardiac malformations) with a specific multiplex ligation-dependent probe amplification designed for CHD screening. They identified 14 rare CNVs in 13 (3.2%) patients, with >80% of the detected imbalances found in children younger than 5 y. The authors conclude that the multiplex ligation-dependent probe amplification assay should be used as a first-tier screen to detect clinically relevant CNVs for the identification of syndromic patients at an early stage.
The development of new technologies has resulted in a better understanding of genome structure and the role of CNVs. The major importance of our findings in patients with CHD and syndromic features is the association of the CNVs related to CHD, as well as the possible clinical impact of such results for the genetic counseling of families.
Methods
Subjects
During a period of 3 y, among the 330 patients evaluated with array CGH, we investigated 55 patients (23 males and 22 females) with array CGH who had CHD according to the available history of complete cardiac evaluation, echocardiogram, and/or cardiac catheterization and operative reports. The types of CHD varied and included the following: 14 subjects with ostium secundum atrial septal defect, 9 with aortic regurgitation, 7 with pulmonic valve stenosis, 5 with a sinus venosus atrial septal defect, 5 with perimembranous ventricular septal defect, 4 with atrioventricular septal defect, 3 with dysplastic mitral valve, 3 with aortic coartaction, 1 with aortic coartaction and perimembranous ventricular septal defect, 1 with aortic coartaction and atrial septal defect, 1 with atrial septal defect and double chamber right ventricle with congestive cardiac failure, 1 with atrial septal defect and aortic dilatation, and 1 with ventricular septal defect and pulmonary hypertension. All subjects had at least one additional indication of chromosomal abnormality: (i) dysmorphic features (26 of 55 patients), (ii) other congenital anomalies (5 urogenital, 15 skeletal, and 17 others), (iii) varying degrees of intellectual disability or learning difficulties (19 of 55 patients), and (iv) neurological disorders (7 seizures, 10 hypotonia, and 15 abnormal magnetic resonance imaging results). Detailed clinical history and examination were provided by experienced clinical geneticists. Clinical data of patients and the results from the array CGH were entered into a database kept at the Department of Medical Genetics. All patients were previously studied by conventional karyotype and/or other diagnostic tests, which were all normal.
The study was approved by the Medical Genetics Review Board of the National Kapodistrian University of Athens, and informed consent for genetic studies was obtained directly from all family members included in the study.
Array CGH Analysis
We used high-resolution commercial Agilent technologies arrays (Santa Clara, CA): the 244K and 4 × 180K platforms (SurePrint G3 arrays). The 244K platform is composed of >236,000 60-mer oligonucleotide probes for the mapped genes or unique DNA sequences with an average spatial resolution of 7.9–8.9 kb (annotated against National Center for Biotechnology Information build 36, hg18). The 4 × 180K platform is composed of >170,000 60-mer oligonucleotide probes with average spatial resolution of 13–25 kb (annotated against National Center for Biotechnology Information build 36, hg18, and National Center for Biotechnology Information build 37, hg19). An array CGH test was performed for each patient using the standardized protocol recommended by the manufacturer and as described previously (6). Slides were scanned with an Agilent microarray scanner G2565CA, software version 4.8.4.1. Image data were extracted and converted to text files with Feature Extraction Agilent Technologies version 10.10.1.1. DNA Analytics v.3.5 and/or Agilent Genomic Workbench 6.5 (Santa Clara, CA) were used to plot the log2 ratio of the signal intensity of each probe. The CNVs were visualized along each chromosome with correspondent National Center for Biotechnology Information annotated gene information for each probe. For the analysis, we used the software built-in aberration detection method (ADM1, threshold 6.7). The cutoff for recording an alteration was ≥4 consecutive probes. For the interpretation of the results, the following databases were used: database of genomic variants (http://projects.tcag.ca/variation/), DECIPHER database (http://www.sanger.ac.uk/PostGenomics/decipher/), and the International Standards for Cytogenomic Arrays (https://www.iscaconsortium.org/) (6).
Statement of Financial Support
No financial assistance was received to support this study.
References
Hoffman JI, Kaplan S . The incidence of congenital heart disease. J Am Coll Cardiol 2002;39:1890–900.
Richards AA, Garg V . Genetics of congenital heart disease. Curr Cardiol Rev 2010;6:91–7.
Ferenez C, Rubin JD, Loffredo CA . Use of prescription and non-prescription drugs in pregnancy. The Baltimore-Washington Infant Study Group. J Clin Epidemiol 1993;46:581–9.
Southard AE, Edelmann LJ, Gelb BD . Role of copy number variants in structural birth defects. Pediatrics 2012;129:755–63.
Kitsiou-Tzeli S, Tzetis M, Sofocleous C, et al. De novo interstitial duplication of the 15q11.2-q14 PWS/AS region of maternal origin: clinical description, array CGH analysis, and review of the literature. Am J Med Genet A 2010;152A:1925–32.
Tzetis M, Kitsiou-Tzeli S, Frysira H, Xaidara A, Kanavakis E . The clinical utility of molecular karyotyping using high-resolution array-comparative genomic hybridization. Expert Rev Mol Diagn 2012;12:449–57.
Cordeiro JM, Marieb M, Pfeiffer R, Calloe K, Burashnikov E, Antzelevitch C . Accelerated inactivation of the L-type calcium current due to a mutation in CACNB2b underlies Brugada syndrome. J Mol Cell Cardiol 2009;46:695–703.
Barc J, Briec F, Schmitt S, et al. Screening for copy number variation in genes associated with the long QT syndrome: clinical relevance. J Am Coll Cardiol 2011;57:40–7.
Klaver EC, Versluijs GM, Wilders R . Cardiac ion channel mutations in the sudden infant death syndrome. Int J Cardiol 2011;152:162–70.
Richards AA, Santos LJ, Nichols HA, et al. Cryptic chromosomal abnormalities identified in children with congenital heart disease. Pediatr Res 2008;64:358–63.
Thienpont B, Mertens L, de Ravel T, et al. Submicroscopic chromosomal imbalances detected by array-CGH are a frequent cause of congenital heart defects in selected patients. Eur Heart J 2007;28:2778–84.
Sørensen KM, El-Segaier M, Fernlund E, et al. Screening of congenital heart disease patients using multiplex ligation-dependent probe amplification: early diagnosis of syndromic patients. Am J Med Genet A 2012;158A:720–5.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Syrmou, A., Tzetis, M., Fryssira, H. et al. Array comparative genomic hybridization as a clinical diagnostic tool in syndromic and nonsyndromic congenital heart disease. Pediatr Res 73, 772–776 (2013). https://doi.org/10.1038/pr.2013.41
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2013.41
This article is cited by
-
Copy number variant analysis for syndromic congenital heart disease in the Chinese population
Human Genomics (2022)
-
Chromosomal microarray analysis in developmental delay and intellectual disability with comorbid conditions
BMC Medical Genomics (2018)
-
Identification of Novel Congenital Heart Disease Candidate Genes Using Chromosome Microarray
Pediatric Cardiology (2018)
-
Chromosome microarray analysis in the investigation of children with congenital heart disease
BMC Pediatrics (2017)
-
Human Induced Pluripotent Stem Cell-Derived Cardiomyocytes as a Model for Heart Development and Congenital Heart Disease
Stem Cell Reviews and Reports (2015)