Abstract
Introduction:
Air-displacement plethysmography (ADP) is an age-appropriate method for measuring relative fat mass (%FM) in children; however, the accuracy of this method has not been evaluated in children aged 5 y or younger.
Results:
Mean %FM values measured by ADP (17.9 ± 8.0%) and by total body water (TBW) (23.7 ± 6.3%) were significantly different (P < 0.001). Regression analysis of %FM by ADP vs. TBW provided a line of best fit with a slope of 0.089, r2 = 0.013, and standard error of the estimate (SEE) = 6.3% FM (P = 0.40).
Discussion:
The error was related to child weight and %FM, but not to behaviors (movement or vocalizations) occurring during the test sequence. A large portion of the error was attributable to imprecision in measuring small volumes. As currently designed, ADP is not an accurate method for measuring %FM in young children. Further investigation of the sources of variability will provide insight into ways of improving the accuracy of this technology for this population.
Methods:
This study examined the accuracy of an ADP system modified for young children (BOD POD; Life Measurement, Concord, CA) by comparing %FM results from ADP with those obtained from TBW by deuterium (D2O) dilution (reference method) in 72 children aged 6–48 mo.
Similar content being viewed by others
Main
The most recent data from the National Health and Nutrition Examination Survey (2007–2008) show that ~10% of children younger than 2 y exceed the 95th percentile weight for length and 21% of 2- to 5-y-old children exceed the 85th percentile body mass index for age and sex (1). The development of this level of overweight early in life is considered a major health concern because early childhood is a critical window for susceptibility to environmental influences that raise the risk of becoming overweight or obese later in life (2,3,4,5). Studies consistently show that early excess weight gain predisposes some children to health problems later in life, particularly obesity and metabolic syndrome (3,6,7,8).
Unlike adults, for whom weight gain largely reflects an increase in fat mass (FM), children accrue all major molecular-level components, including minerals, water, proteins, and FM, during normal growth and development (9,10). Despite this complexity of growth, little research has documented the composition of weight gain during early childhood and whether it may be a more sensitive and specific indicator of risk for later health outcomes than weight gain alone (6). One reason for this lack of crucial research is that most body-composition assessment techniques commonly used in adults, including dual X-ray absorptiometry, skinfold thicknesses, and underwater weighing, are not appropriate for young children because the techniques are behaviorally unsuitable, are invalidated by the “chemically immature” body, or have not been suitably developed and validated in this age group (11,12,13,14). The advancement of child body-composition research depends on developing and/or identifying methods that are accurate, safe, noninvasive, and practical for use in children (12,15,16).
Air-displacement plethysmography (ADP) is a whole-body densitometric technique based on displacement of air, rather than water. The adult ADP system, commercially produced under the trade name BOD POD (Life Measurement, Concord, CA), has been validated in adult populations (17,18) and shows promise for the measurement of body composition of children aged 5 y and older (12,19,20,21,22,23,24,25,26,27). To date, no published studies report the accuracy of the adult ADP system in children younger than 4 y. In this study, we investigated the accuracy of a modified ADP system in healthy children aged 6–48 mo. Relative FM (%FM) measured by ADP was compared with a reference method, deuterium (D2O) dilution. On the basis of results of ADP validation studies in children older than 5 y, we hypothesized that the prediction error (standard error of the estimate (SEE)) of ADP would be ≤2.5% FM, a level considered to be excellent by body-composition standards (28).
Results
Seventy-two children (94% non-Hispanic white, 2% Asian, and 4% other) were enrolled in the study; however, not all the children were willing or able to complete all study procedures. Three children were dismissed from the study because of unwillingness to have anthropometric measurements taken, leaving 69 children remaining in the sample. Anthropometric data are available for 96% of the sample, and D2O data are available for 94% of the sample. For ADP, 76% of children completed two test sequences, 14% completed only one test sequence, and 10% did not complete a single sequence. Table 1 shows the characteristics of children with complete anthropometric data (N = 69).The average age was 25.4 ± 13.1 mo, average weight-for-age percentile was 50.9 ± 25.9, and average stature-for-age percentile was 46.2 ± 27.5 (mean ± SD).
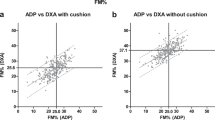
The ADP system did not provide %FM results for 11 children weighing less than 8 kg; the software did not contain thoracic gas volume and body surface area artifact correction equations for children of this weight. The remaining sample of children (n = 58) completed at least one ADP test for which %FM results were calculated. The mean ± SD %FM was 17.9 ± 8.0 for ADP and 23.7 ± 6.3 for D2O (P < 0.001). A scatter plot showing the relationship between D2O and ADP for the measurement of %FM is presented in Figure 1 . Regression analysis produced a line of best fit (Y = 0.089X + 22.1, r2 = 0.013, SEE = 6.3% FM), which was not statistically significant (P = 0.40).
%FM by D2O vs. ADP for children aged 4–48 mo. The solid line is the line of best fit (Y = 0.089X + 22.1, r2 = 0.013, SEE = 6.3% FM, P = 0.40); the dashed line is the line of identity. ADP, air-displacement plethysmography; D2O, deuterium oxide; %FM, relative fat mass; SEE, standard error of the estimate.
Analysis of the error between methods showed a mean difference in %FM between techniques (D2O − ADP) of 5.8 ± 9.6 and a two-SD limit of agreement between methods of −13.4 to 25% FM. Figure 2 is a plot depicting the difference in %FM between methods (residuals) vs. the average %FM between the methods ( Figure 2a ) and child weight ( Figure 2b ). Regression analysis revealed that the residuals were statistically related to both %FM (Y= −0.651X + 19.1, r2 = 0.15, P = 0.003) and body weight (Y= 1.17X − 9.7, r2 = 0.09, P = 0.02). Figure 3 is a Bland–Altman plot depicting the difference in %FM between residuals vs. the agitation score ( Figure 3a ) and stillness score ( Figure 3b ). Visual inspection of the plots did not reveal a noticeable relationship between the subjectively scored behaviors and the difference in %FM between techniques.
Bland–Altman plots showing individual differences in %FM between ADP and D2O vs. (a) the mean %FM between both methods and (b) child weight. For (a), the short dash line represents the mean difference and the long dash line represents the ±2 SD limits for the difference values. For (a) and (b), the solid line represents the line of best fit. ADP, air-displacement plethysmography; D2O, deuterium oxide; %FM, relative fat mass.
Figure 4 shows a comparison of coefficient of variation (CV) values for raw body volumes generated during testing of children and volume phantoms. The CV values were threefold higher for the child-size tank (~20 l) and 18-fold higher for the infant-size tank (~3 l) compared with the standard adult-size tank (~50 l). In addition, raw body volume measurement of children had a sixfold higher CV than typically seen for adults measured in our laboratory setting.
Discussion
Childhood poses multiple challenges to the development of safe and valid body-composition measurement techniques, including both chemical and behavioral immaturity (9,10,29). The purpose of this study was to investigate the accuracy of ADP as a method for measuring body composition in children aged 6–48 mo. Our results suggest that our current ADP system, which includes several hardware and software modifications for use with young children, does not provide valid measurements of %FM in children aged 6–48 mo.
To date, ADP validity studies have evaluated children as young as 5 y, but more typically those aged 10 y and older. In studies comparing ADP to gold standard methods in school age children (7–14 y), the low mean %FM differences between methods suggest that ADP is reasonably accurate on a group level (20,27,30). However, accuracy on an individual basis remains a concern, with 95% limits of agreement at ±4.2% FM in a previous study (27).
The results from our study suggest that ADP lacks the accuracy necessary for routine use in clinical and research settings in children aged 6–48 mo. SEE values exceeding 6.0% FM are considered poor by current standards (28). Thus, the SEE of 6.3% FM observed in this sample ( Figure 1 ) suggests that this ADP system is unable to measure %FM accurately in young children. On average, ADP overestimated %FM compared with D2O by ~5% FM, and the error was related in part to both adiposity and size of child. For children who weigh less than 10 kg and have high %FM, ADP was most likely to underestimate %FM relative to D2O. In contrast, for older and larger children, who tend to be leaner than infants, ADP was more likely to overestimate %FM relative to D2O, as shown in Figure 2 .
Small body size may present measurement difficulties for ADP because small body volume results in less air displacement and consequently, a lower “signal-to-noise” ratio (27). Previous observations suggest that the CVs of repeated volume measurements increase substantially at volumes less than 40 l (31). In our data shown in Figure 4 , the ~20-l phantom had 3 times the CV, and the ~3-l phantom had 18 times the CV of the 50-l phantom measurements. The average variability in volume measurement of the 3-l tank (0.478%) would propagate into an approximate ±2.59% FM error for the average size child (12.2 kg) in this study. In addition, the mean CV during child body-volume measurement (0.665%) was substantially greater than the precision typically observed during measurements of adults in our laboratory (0.117%) and other laboratories (0.071–0.127%) (20,32,33). The decreased precision of volume measurement in measuring small children is a methodological barrier that must be overcome before ADP can be widely used in clinical and research settings. Future research should systematically evaluate all possible sources of precision problems, including child size and behavioral response to testing (movement and vocalizations; data shown in Figure 3 ), to determine whether additional modifications to the ADP system may improve accuracy and precision.
Although D2O dilution is commonly used as the reference technique for body-composition studies of young children,(24,27,34,35) its limitations should be acknowledged. Its accuracy, safety, and noninvasiveness (36) make it an appealing gold standard; however, the method assumes complete and equal equilibration of D2O in all body water compartments within 4 h. The method also requires adjustment for overestimation of total body water (TBW) in children younger than 2 y because of variability in body fatness during infancy (34). We acknowledge that the measurement error associated with estimating thoracic gas volumes in young children also may contribute to measurement error. Although Fields et al. developed suitable predictive equations for children aged 6–17 y, the performance of prediction equations for very young children requires more research (37).
In summary, to our knowledge, this is the first published study to examine the accuracy of the BOD POD ADP system in children aged 6 mo to 4 y. We found that ADP measurement is feasible in this age–range because 90% of children completed at least one complete test sequence in this study. However, our data suggest that, as currently designed, ADP does not provide a valid measurement of body-composition components, in part due to poor precision in measuring smaller volumes. Changes in ADP test-chamber design, software, or hardware may improve the accuracy of body-volume measurements in young children. Further research is needed to make this technology, which is well-suited for use in young children, accurate enough for research and clinical applications.
Methods
Subjects and Protocol
A convenience sample of 72 healthy children aged 6–48 mo was recruited from Centre County, Pennsylvania, and the surrounding areas. During the 5-h laboratory visit, children’s growth and body composition were measured using anthropometry, ADP, and D2O dilution. Children who were known to be claustrophobic, recently ill, or dehydrated were screened out of the study. The study protocol was approved by the institutional review board at The Pennsylvania State University, and all parents provided written informed consent for the participation of their child.
Anthropometry
For children aged 6–23 mo, recumbent length was measured to the nearest millimeter using an infantometer (Seca Model 416; Seca, Hamburg, Germany), and weight was measured using an infant scale (Seca Model 374; Seca). For children aged 24–48 mo, standing height was measured to the nearest millimeter using a wall-mounted stadiometer (Seca Model 240; Seca), and weight was measured using the scale provided with the ADP device (scale, Model BWB-627-A; Tanita, Tokyo, Japan). Anthropometric measurements were performed by the two coauthors in duplicate using standard measurement techniques (38), and all equipment was calibrated each day.
ADP
Body density was measured using the BOD POD body-composition measurement system (Life Measurement Instruments, Concord, CA) according to the manufacturer’s instructions and as previously detailed by other authors (39). All quality-control procedures were completed each day. Manufacturer recommendations for testing attire were followed: children wore a spandex swim cap and a tight-fitting swimsuit or were nude. Lung volume (VTG) was estimated for each subject according to age, sex, and height as described by Fields (37,40).
Several modifications were made to the ADP system to enable testing of young children. We used a specifically designed child seat with removable tray that securely attached to the bench seat to safely confine the child during testing. In addition, a child-sized (~20 l) National Institute of Standards and Technology–traceable volume phantom was used for system calibration to more closely match the body volume of young children. Finally, Life Measurement provided modified software to facilitate body-composition testing of small children. We attached a portable DVD player or test-compatible toys to the tray of the child seat to entertain children during the testing procedure. These items were added to the testing chamber during system calibration and were “zeroed out” from child body-volume measurements.
A complete body-composition test sequence included measurement of body mass and three 45-s measurements of body volume. The two body-volume measurements closest in agreement were used by the system software to calculate the average body volume and body density (Db) of the child. We calculated percent fat mass (% FM) from Db using the equation below and a value of 0.901 g/ml for the density of FM (DF) and age- and sex-specific density of fat-free mass (DFFM) as provided by Butte et al. (41):

On the basis of our laboratory’s previous observation that child movement and vocalizations may relate to error in volume measurement, we elected to subjectively score the child’s behavioral response to testing. For each of the three volume measurements, child agitation (vocalization) was subjectively scored as: 1, quiet; 2, fussy/talking; or 3, crying/yelling/singing; and child stillness was subjectively scored as: 1, still; 2, some movement (arms); or 3, substantial movement (entire body). The three scores were added to produce a score ranging from 3 to 9 for both agitation and stillness.
TBW
TBW determination by D2O dilution was performed as previously described by Schoeller (36). In brief, a baseline urine sample was collected from disposable gel-free diapers (Tushies, Eau Claire, WI) or from a potty seat on arrival at the laboratory. Then, each subject consumed a dose of 0.06 g D2O/kg body weight diluted with tap water (16.7% D2O) to increase dose volume (Cambridge Isotope Laboratories, Andover, MA). Fruit flavoring was added to the dose solution to increase acceptance. Urine samples were collected at 3 and 4 h after dosing from either a gel-free diaper or potty seat. Urine samples were frozen and stored at −80 °C until the time of analysis. D2O enrichment values were determined using isotope ratio mass spectrometry, and the resultant TBW values were corrected for nonaqueous exchange of hydrogen (36). TBW values obtained from the 4-h postdose urine sample were used for data analyses, except when a sample was not produced at that time point, and the 3-h postdose TBW value was used.
TBW values were adjusted to account for the limited food and beverage intake during the equilibration period (0–3 h). Intake of foods or beverages and infant formula was measured to the nearest tenth of a gram. Breast milk intake from nursing was measured to the nearest gram. Water intake from foods and beverages was calculated using Nutrition Data System for Research 2009 software (University of Minnesota, Minneapolis, MN) and then subtracted from TBW results. Fat-free mass was calculated from TBW by using age- and sex-specific hydration of fat-free mass coefficients as described by Butte et al. (41) for children up to 2 y of age and as described by Fomon (9) for children aged 2 to 4 y.
Precision Study
Approximately 125 volume measurements per phantom were collected over a 3-mo period on National Institute of Standards and Technology–certified volume phantoms of ~3, 20, and 50 l. The data were used to evaluate precision, defined as the mean CV for the entire pool of measurements made on a phantom. Using the quality-control volume feature of the ADP software, we completed the two-point calibration procedure, and then the ADP system made six volume measurements on the phantom. The ADP system was calibrated using the same size phantom to be measured, except that the 20-l phantom was used to calibrate for 3-l tank measurements because of software restrictions.
Statistical Analysis
Percentiles and z-scores for anthropometric data were calculated using age- and sex-specific 2000 Centers for Disease Control and Prevention growth chart reference data and the SAS program (version 9.1.3; SAS Institute, Cary, NC). IBM SPSS Statistics (version 18; SPSS, Somers, NY) was used for all subsequent analyses. We used linear regression analysis to compare %FM values between ADP and D2O methods, including calculation of the line of best fit and measures of data scatter (r2, SEE, and total error). The mean and two-SD difference between methods were calculated, and a paired-sample two-tailed t-test was used to determine whether this difference was significant. Bland–Altman plots (42) were used to visually explore the relationship between residuals (error) and %FM, child weight, movement during testing, and agitation during testing. For precision testing of calibration phantoms and people, the CV of volume measurements was calculated. Statistical significance was set at P ≤ 0.05.
Statement of Financial Support
Life Measurement, Inc., provided prototype equipment and software for the project and technical support at no cost. They did not provide any input in the writing of this article.
References
Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM . Prevalence of high body mass index in US children and adolescents, 2007-2008. JAMA 2010;303:242–9.
Chomtho S, Wells JC, Williams JE, Davies PS, Lucas A, Fewtrell MS . Infant growth and later body composition: evidence from the 4-component model. Am J Clin Nutr 2008;87:1776–84.
Dennison BA, Edmunds LS, Stratton HH, Pruzek RM . Rapid infant weight gain predicts childhood overweight. Obesity (Silver Spring) 2006;14:491–9.
Gungor DE, Paul IM, Birch LL, Bartok CJ . Risky vs rapid growth in infancy: refining pediatric screening for childhood overweight. Arch Pediatr Adolesc Med 2010;164:1091–7.
Adair LS . Child and adolescent obesity: epidemiology and developmental perspectives. Physiol Behav 2008;94:8–16.
Wells JC, Chomtho S, Fewtrell MS . Programming of body composition by early growth and nutrition. Proc Nutr Soc 2007;66:423–34.
Stettler N, Stallings VA . Adult obesity and growth in childhood. Association of birth weight with adult weight is confounded by maternal body mass index. BMJ 2002;324:674.
Ong KK, Ahmed ML, Emmett PM, Preece MA, Dunger DB . Association between postnatal catch-up growth and obesity in childhood: prospective cohort study. BMJ 2000;320:967–71.
Fomon SJ, Haschke F, Ziegler EE, Nelson SE . Body composition of reference children from birth to age 10 years. Am J Clin Nutr 1982;35:Suppl 5:1169–75.
Fomon SJ, Nelson SE . Body composition of the male and female reference infants. Annu Rev Nutr 2002;22:1–17.
Lohman TG . Assessment of body composition in children. Ped Exerc Sci 1989;1:19–30.
Fields DA, Goran MI . Body composition techniques and the four-compartment model in children. J Appl Physiol 2000;89:613–20.
Paineau D, Chiheb S, Banu I, et al. Comparison of field methods to estimate fat mass in children. Ann Hum Biol 2008;35:185–97.
Baur L . Body composition measurement in normal children: ethical and methodological limitations. Asia Pacific J Clin Nutr 1995;4:35–38.
Elberg J, McDuffie JR, Sebring NG, et al. Comparison of methods to assess change in children’s body composition. Am J Clin Nutr 2004;80:64–9.
Radley D, Fields DA . Need for optimal body composition data analysis using air-displacement plethysmography in children and adolescents. J Nutr 2006;136:709; author reply 710.
McCrory MA, Gomez TD, Bernauer EM, Molé PA . Evaluation of a new air displacement plethysmograph for measuring human body composition. Med Sci Sports Exerc 1995;27:1686–91.
Fields DA, Goran MI, McCrory MA . Body-composition assessment via air-displacement plethysmography in adults and children: a review. Am J Clin Nutr 2002;75:453–67.
Nuñez C, Kovera AJ, Pietrobelli A, et al. Body composition in children and adults by air displacement plethysmography. Eur J Clin Nutr 1999;53:382–7.
Dewit O, Fuller NJ, Fewtrell MS, Elia M, Wells JC . Whole body air displacement plethysmography compared with hydrodensitometry for body composition analysis. Arch Dis Child 2000;82:159–64.
Nicholson JC, McDuffie JR, Bonat SH, et al. Estimation of body fatness by air displacement plethysmography in African American and white children. Pediatr Res 2001;50:467–73.
Buchholz AC, Majchrzak KM, Chen KY, Shankar SM, Buchowski MS . Use of air displacement plethysmography in the determination of percentage of fat mass in african american children. Pediatr Res 2004;56:47–54.
Lockner DW, Heyward VH, Baumgartner RN, Jenkins KA . Comparison of air-displacement plethysmography, hydrodensitometry, and dual X-ray absorptiometry for assessing body composition of children 10 to 18 years of age. Ann N Y Acad Sci 2000;904:72–8.
Plasqui G, den Hoed M, Bonomi A, Westerterp KR . Body composition in 10-13-year-old children: a comparison between air displacement plethysmography and deuterium dilution. Int J Pediatr Obes 2009;4:397–404.
Claros G, Hull HR, Fields DA . Comparison of air displacement plethysmography to hydrostatic weighing for estimating total body density in children. BMC Pediatr 2005;5:37.
Ittenbach RF, Buison AM, Stallings VA, Zemel BS . Statistical validation of air-displacement plethysmography for body composition assessment in children. Ann Hum Biol 2006;33:187–201.
Wells JC, Fuller NJ, Wright A, Fewtrell MS, Cole TJ . Evaluation of air-displacement plethysmography in children aged 5-7 years using a three-component model of body composition. Br J Nutr 2003;90:699–707.
Lohman TG . Advances in Body Composition Assessment. Champaign, IL: Human Kinetics, 1992.
Heyward VH, Wagner DR . Applied Body Composition Assessment, 2nd edn. Champaign, IL: Human Kinetics, 2004:109–121.
Wells JC, Douros I, Fuller NJ, Elia M, Dekker L . Assessment of body volume using three-dimensional photonic scanning. Ann N Y Acad Sci 2000;904:247–54.
Collins AL, McCarthy HD . Evaluation of factors determining the precision of body composition measurements by air displacement plethysmography. Eur J Clin Nutr 2003;57:770–6.
Wells JC, Fuller NJ . Precision of measurement and body size in whole-body air-displacement plethysmography. Int J Obes Relat Metab Disord 2001;25:1161–7.
Anderson DE . Reliability of air displacement plethysmography. J Strength Cond Res 2007;21:169–72.
Wells JC, Fewtrell MS, Davies PS, Williams JE, Coward WA, Cole TJ . Prediction of total body water in infants and children. Arch Dis Child 2005;90:965–71.
Ma G, Yao M, Liu Y, et al. Validation of a new pediatric air-displacement plethysmograph for assessing body composition in infants. Am J Clin Nutr 2004;79:653–60.
Schoeller DA . Hydrometry. In: Roche A, Heymsfield S, Lohman T, eds. Human Body Composition. Champaign, IL: Human Kinetics, 1996:25–44.
Fields DA, Hull HR, Cheline AJ, Yao M, Higgins PB . Child-specific thoracic gas volume prediction equations for air-displacement plethysmography. Obes Res 2004;12:1797–804.
Lohman TG, Roche AF . Anthropometric Standardization Reference Manual. Champaign, IL: Human Kinetics, 1988.
Dempster P, Aitkens S . A new air displacement method for the determination of human body composition. Med Sci Sports Exerc 1995;27:1692–7.
Higgins PB, Silva AM, Sardinha LB, et al. Validity of new child-specific thoracic gas volume prediction equations for air-displacement plethysmography. BMC Pediatr 2006;6:18.
Butte NF, Hopkinson JM, Wong WW, Smith EO, Ellis KJ . Body composition during the first 2 years of life: an updated reference. Pediatr Res 2000;47:578–85.
Bland JM, Altman DG . Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986;1:307–10.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rosendale, R., Bartok, C. Air-displacement plethysmography for the measurement of body composition in children aged 6–48 months. Pediatr Res 71, 299–304 (2012). https://doi.org/10.1038/pr.2011.42
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2011.42
This article is cited by
-
Air displacement plethysmography (pea pod) in full-term and pre-term infants: a comprehensive review of accuracy, reproducibility, and practical challenges
Maternal Health, Neonatology and Perinatology (2018)
-
Body composition of term healthy Indian newborns
European Journal of Clinical Nutrition (2016)
-
Challenges in infant body composition
Pediatric Research (2012)