Abstract
The aim of this study is to describe the effect of sedation and analgesia on postoperative amplitude-integrated EEG (aEEG) in newborns with congenital heart disease (CHD) undergoing heart surgery. This is a consecutive series of 26 newborns with CHD of which 16 patients underwent cardiopulmonary bypass (CPB) surgery and 10 patients did not. aEEG was monitored for at least 12 h preoperatively and started within the first 6 h postoperatively for 48 h. Outcome was assessed at 1 year of age. All 26 patients showed a normal preoperative continuous cerebral activity with sleep-wake cycles (SWC). The postoperative duration to return to normal background activity with SWC was similar for both groups. Independent of group assignment, patients requiring midazolam had a significantly later onset of a normal SWC than those without midazolam (p = 0.03). Three patients in the CPB group and two in the non-CPB group showed continuous low voltage or flat trace after administration of fentanyl. These changes did not correlate with neurodevelopmental outcome. Sedation with midazolam has a transient effect on the background activity, whereas fentanyl can induce a severe pathologic background pattern. The significance of these changes on outcome is not yet clear. Thus, more attention should be paid to these effects when interpreting aEEG in this population.
Similar content being viewed by others
Main
Amplitude-integrated electroencephalography (aEEG) is a widely used tool in the neonatal intensive care unit. In newborns with hypoxic ischemic encephalopathy (HIE), aEEG is used to detect infants suitable for inclusion in cooling trials (1) and is a valuable prognostic tool for the outcome in this patient group (2–5). Patients with congenital heart disease (CHD) may face a variety of long-term neurodevelopmental sequelae (6). However, in this patient group, aEEG is not used as a routine monitoring and little is known about aEEG changes and their prognostic value (7). Toet et al. (7) described that the postoperative sleep-wake cycle (SWC) normalization varied significantly. Postoperative medications for pain relief and sedation are routinely used in the cardiac population, but their influence on aEEG has not been reported so far. In neonates with seizures due to HIE, the administration of midazolam was associated with a background depression (8). When interpreting the aEEG in infants receiving sedation or analgesia, it is however important to know whether medication could alter aEEG findings and therefore limit the predictive strength of the aEEG.
Thus, the aim of this study is to describe postoperative aEEG changes in newborns with CHD undergoing heart surgery and to examine the effect of sedation and analgesia on postoperative aEEG. Additionally we correlated these findings with 1 year neurodevelopmental outcome.
METHODS AND PATIENTS
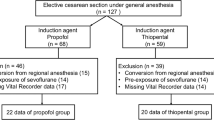
This is a consecutive series of 26 newborns with CHD undergoing surgical repair in the neonatal period between June 2006 and June 2008. Because analgesia and sedation are more frequently used in patients with complex CHD undergoing cardiopulmonary bypass surgery (CPB), we compared two groups of cardiac patients: one group with CPB surgery (16 patients) and the other group (10 patients) without CPB surgery. Infants in the group with CPB surgery were all diagnosed with transposition of the great arteries with simple anatomy. Infants with congenital or acquired brain injury, detected by routine head ultrasound, and/or with other (chromosomal and metabolic) abnormalities were excluded. The study was approved by the ethical committee of the University Children's Hospital Zurich and the ethical committee of the Canton of Zurich, and written informed consent was obtained from all parents.
Monitoring electrocortical brain activity.
A continuous aEEG recording BRM2 Brain Monitor (BrainZ Instruments Ltd, Auckland, New Zealand) was used to monitor electrical brain activity. The BRM2 records a two-channel EEG from four central and parietal needle electrodes corresponding to C3, C4 and P3, P4, respectively, (according to the international EEG classification 10–20 classification, ground FZ). The filtered signal is rectified, smoothed, and amplitude-integrated. aEEG pattern classifications and abbreviations are used according to de Vries et al. (9), which is based on the definition by Hellstöm-Westas et al. (4) and Toet et al. (10) as continuous normal voltage (CNV), discontinuous normal voltage (DNV), burst suppression (BS), continuous low voltage (CLV), and flat tracing (FT). Epileptic activity was identified according to Toet et al. (11). Sleep-wake cycles (SWC) were analyzed as no sleep-wake cycling, imminent/immature SWC and normal respectively developed SWC (10). All aEEGs were analyzed by one experienced clinician (V.B.) and double checked by an independent neurophysiologist blinded to the patients history and perioperative course (G.W.).
Preoperative aEEG was monitored for at least 12 h preoperatively. aEEG was started within the first 6 h after surgery (median 5.5 h, range 2.0–8.5). In three infants, the recording was started later than 6 h after surgery (6.5, 7.5, and 8.5 h postoperatively). The aEEG recording continued for ∼48 h postoperatively (median 45.5 h, range 20.3–67.4 h). Five children had recordings that lasted shorter than 36 h but a minimum of 20 h. This time frame was used to insure the stability of the patients postoperatively.
A transient DNV was defined if infants developed a normal background pattern within the recording time. A persistent DNV was defined if no recovery occurred within the recording time.
SWC onset was defined as the time (h) at which a SWC occurred after surgery. If the SWC was present when the aEEG was placed (e.g. 6 h postoperatively), then 6 h was used as the time of onset. Accordingly, if no SWC were recorded until the aEEG was dismounted, the duration the aEEG was placed (e.g. 48 h) was added to the duration until the aEEG was placed postoperatively (e.g. 48 plus 6 h). Delayed SWC was defined according to Osredkar et al. (12) if SWC did not occur within 36 h after surgery.
Anesthesia and perfusion techniques.
Surgery was performed by two pediatric cardiac surgeons. In all patients, anesthesia was induced i.v. with etomidate, midazolam, and sufentanyl or fentanyl for the patients on CPB. Patients without bypass surgery usually required midazolam and fentanyl or sufentanyl for anesthesia induction. Ventilator settings were adapted to maintain normocapnia. Routine monitoring consisted of ECG, invasive arterial and central venous pressures, pulse oximetry, central and peripheral temperature measurements and bispectral index (BIS) (Aspect Medical Systems, Inc, Newton, MA) for all patients. Alpha-stat blood gas management was routinely applied. CPB surgery was performed in normal or mild hypothermia (rectal temperature >32°C) with a pump flow rate at 100 to 150 mL/kg per minute to achieve a mean arterial pressure of 40 to 50 mm Hg. Modified ultrafiltration at the end of CPB was performed in all patients on bypass. During weaning from CPB, all patients required adrenaline supplemented by milrinone and/or noradrenaline to wean the patients off CPB. Patients without bypass were on milrinone with or without adrenaline. In the pediatric cardiac intensive care unit, all patients were placed on continuous morphine infusion at 20 μg/kg/h. Midazolam was preferably given as continuous infusion and sometimes supplemented by bolus administration. Maximal infusion doses and length of administration were recorded for midazolam and morphine. Mechanical ventilation was discontinued when the patient was in a stable cardiopulmonary condition requiring low dose or no inotropic support. In patients with delayed sternal closure, fentanyl boluses of 10 μg/kg were given for surgical closure. None of the patients received fentanyl as continuous infusion. Lactate and glucose levels were monitored.
Outcome.
All infants who underwent CPB surgery were followed at the Child Development Center of the University Children's Hospital Zurich. Follow-up was available for all surviving infants (n = 15) in the CPB group. In the surviving infants without CPB (n = 9), outcome was available for three children. Overall, outcome data were available for 18 of 24 children (75%). At 1 year of age the Bayley Scales of Infant Development II providing a mental development index (MDI) and a psychomotor developmental index (PDI) (13) was administered. In addition, a standardized neurologic examination resulting in a neurologic severity score (14) was performed.
Statistics.
Comparisons between groups were performed with the Mann-Whitney U test for continuous or categorical variables and with χ2 and Fishers exact for dichotomous variables. Correlations were performed using the Spearman rank correlation. Comparisons with the reference norms for the MDI and PDI were performed using the Wilcoxon sign-rank test. We also performed multiple linear regression analysis including group (with CPB and without CPB) and medication as independent variables and onset of SWC as the dependent variable.
RESULTS
Patient's characteristics are shown in Table 1. The patients operated on CPB were all diagnosed with transposition of the great arteries with simple anatomy and had an arterial switch operation. The other patients were diagnosed with varying cardiac lesions such as coarctation (n = 3), ventricular septal defect (n = 2) and one each with interrupted aortic arch, tetralogy of Fallot, pulmonary atresia, hypoplastic left heart syndrome, and double outlet right ventricle. Surgical procedure in this group was either resection of the coarctation, pulmonary banding or placement of an aterial to pulmonary shunt.
Patient characteristics (Table 1) were not different between the two groups except for 10 min Apgar scores, which were lower in the CPB group compared with the non-CPB group. Postoperatively, blood glucose levels in the first 24 h were significantly higher, and the days on ventilation were longer in the CPB group compared with the non-CPB group. Accordingly, duration of anesthesia and surgery was longer in the CPB group compared with the non-CPB group. One patient in each group died: in the non-CPB group, a 6-mo-old infant died after the second operation consisting of a cavopulmonary anastomosis, and in the CPB group, a 3-mo-old infant died because of myocardial infarction.
aEEG results.
The aEEG results are presented in Table 2. Duration of preoperative aEEG monitoring was similar for the CPB group and the non-CPB group (median 20.4 h vs 19.6 h, p = 0.86). All patients in both groups showed a normal preoperative continuous background pattern with SWC.
Postoperative aEEG findings.
None of the patients in both groups showed postoperative seizure activity on aEEG. Transient DNV occurred more frequent in the CPB group (68%) compared with the non-CPB group (40%) but did not reach statistical significance (p = 0.18). Only one child was diagnosed with persistent DNV. This child had a recording time of 42 h, which lies in the range for all recordings. The duration to return to a normal background pattern with SWC was similar for both groups (Fig. 1). We compared the recovery of normal background activity to occurrence of SWC in the group of patients with transient DNV. Normalization of the background pattern occurred earlier than occurrence of SWC (median 9 vs 10.7 h, respectively, p = 0.01). Three patients in the CPB group and two patients in the non-CPB group did not show any SWC during the whole time of the monitoring with an otherwise CNV pattern.
We also examined whether the time to return to normal SWC was related to perioperative parameters. There was no relationship between the length of CPB (R = −0.39, p = 0.18) or the duration of surgery (R = 0.06, p = 0.79) with the time to return to SWC (Table 3). However, there was a significant correlation between administration of midazolam and the duration of surgery and mechanical ventilation (Table 3).
Two patients in the CPB group showed a CLV background. In one of these two patients, CLV occurred directly postoperatively with no intraoperative correlate in the BIS monitoring and CPB-related complication. In the second patient, initially a DNV was present, but after delayed sternal closure and fentanyl administration, a CLV activity was observed for the following 6 h until the end of aEEG monitoring. During the time of delayed sternal closure, both patients had blood pressure and oxygen saturation in a normal range as well as a normal renal and hepatic function. Postoperative cranial ultrasound was normal in both patients. In addition to these two patients, three other patients received fentanyl for delayed sternal closure. These patients showed a CLV background activity but recovered between 1.5 and 6.5 h to normal background pattern.
Sedation, analgesia, and aEEG.
All patients except one in the CPB group required midazolam infusion compared with four in the non-CPB group. Midazolam administration was significantly more frequent in the CPB group than in the non-CPB group (p = 0.005), but when administered, the duration was similar (Table 2). For all patients, those requiring midazolam had a significantly later onset of a normal SWC than those without midazolam (p = 0.03). However, the duration of midazolam administration did not correlate with the onset of sleep-wake cycling (R = −0.13; p = 0.83, Table 3). When group (CPB or non-CPB) was included in a logistic regression analysis in addition to the variable midazolam administration, the CPB group was not associated with SWC onset (p = 0.73). However, midazolam administration remained associated with later onset of SWC, but this association did not reach statistical significance (p = 0.14).
For the total group, there was no effect of the dosage of midazolam (p = 0.95) or morphine (p = 0.34) on persistence CNV or return to SWC. The two patients with persistent CLV had midazolam infusion only for 1.5 and 4 h, respectively.
We also detected transient CLV in those infants who underwent delayed sternal closure with fentanyl sedation. In the CPB group, the two patients with CLV developed CLV after fentanyl administration and continued to show CLV and one showed a FT (Fig. 2). One patient in the CPB group showed transient CLV also in association with fentanyl administration but returned to normal background pattern. Similarly, two patients in the non-CPB group showed transient CLV, both in association with fentanyl administration secondary to sternal closure.
Outcome.
Neurodevelopmental outcome is presented in Table 4 for the total group and stratified for different subgroups. Overall MDI and PDI were significantly lower than the normal population (p = 0.02, p = 0.003, respectively). No significant difference in outcome was found between the subgroups in Table 4. For the entire group, there was no correlation between time of onset of SWC and neurodevelopmental outcome (MDI: R = 0.12, p = 0.68; PDI: R = 0.32, p = 0.26; neuroscore: R = 0.011, p = 0.97). We also looked whether the delayed SWC onset (>36 h) was associated with adverse outcome. Again, no such association was detected (data not shown). The same was true for the persistence of CLV and outcome; no association between persistent CVL or FT (n = 2) and neurodevelopmental outcome (Mann-Whitney: MDI: p = 0.84; PDI: p = 0.84; neuroscore: R = −0.12, p = 0.83) was found. However, the numbers were small.
DISCUSSION
The aim of this study was to describe the influence of sedation and analgesia on postoperative aEEG findings in patients with CHD undergoing cardiac surgery.
We could show that most patients showed a DNV activity postoperatively, which recovered to a CNV pattern. In the non-CPB group, two patients showed a pathologic CLV at the end of the aEEG monitoring period. In addition, the onset of SWC in patients requiring midazolam was significantly later, but the duration of midazolam treatment showed no effect on reoccurrence of SWC. The most impressive change in the aEEG was the effect of fentanyl administration causing CLV or flat trace recording. In addition, we did not find a correlation between aEEG changes and outcome at 1 year.
Today, aEEG is a bedside tool in many neonatal intensive care units, mostly used to monitor newborns with hypoxic-ischemic encephalopathy (HIE). The good predictive value of this monitoring tool has been validated in several studies; specifically, time to recover to a normal background pattern and the onset of SWC has been identified as important prognostic factors in patients with HIE (10,15–18). Little is known about the influence of different medication on aEEG, so far. Van Leuven et al. (8) described a transient background depression of 2 h in 4 of 15 newborns with therapeutic doses of midazolam for asphyxiated newborn with seizures. However, the main type of background pattern (DNV) did not change considerably or was transient, especially in the patients with a good prognosis. This is comparable with our findings. In our study, treatment with midazolam delayed the beginning of sleep-wake cycling, but even under this treatment normalization of the background pattern with SWC occurred. Niemarkt et al. (19) published a patient who received an accidental overdose (5000 μg/kg) of morphine and who developed a change of the background pattern from CNV to DNV. No other changes were found. In preterm infants morphine, diazepam and phenobarbitol can cause a depression on the background patterns of the EEG (20). The patients in our study recovered to a normal continuous background pattern with SWC even when still treated with continuous i.v. morphine.
The study of Toet et al. (7) showed that normalization of aEEG with occurrence of SWC after open heart surgery varied between 8 h and several days. They did not address the role of sedation in their study, but their postoperative treatment with morphine and midazolam was comparable with our treatment regime. Nguyen et al. (21) described the effect of sufentanyl on EEG in preterm infant. They showed that the EEG pattern after bolus injection induced a significant increase of EEG discontinuity in preterm. Interestingly, the range of sufentanyl serum concentration was extremely wide despite that all patients received the same dose per kilogram. They could not show a relationship between EEG changes and sufentanyl serum concentration. The severe drop of the aEEG amplitude to low-voltage pattern in the five patients receiving fentanyl for delayed sternal closure in our study may be explained by the high variability of pharmacokinetics in newborn. The two patients in which the low-voltage pattern persisted showed normal blood pressure and renal function at the time of fentanyl administration. Despite normal vital parameters in our patients, variability of pharmacokinetics in newborn has been demonstrated in several studies (22–26). Opiates are metabolized in the liver by nonspecific monoamine oxidases, and inactive metabolites are excreted in urine (27–28). The hepatic and renal function of sick newborns (especially after CPB) may induce individual metabolic variations with a significant effect on the metabolism of drugs such as fentanyl.
In infants with HIE, aEEG has a strong predictive value for the neurodevelopmental outcome (2–5). To date, this is the only condition where aEEG has been shown to have a high predictive value for later neurodevelopmental outcome. In our small population of infants undergoing heart surgery for CHD, we could not find a correlation between aEEG changes because of medication and neurodevelopmental outcome. Therefore, medication might be a potential confounder, which may lessen the predictive power of the aEEG in this special patient group. However, our patient sample is small and thus limits the power to detect an association between aEEG changes and outcome. In addition, no statistical subgroup analysis was possible.
A limitation of our study is that we do not have a continuous aEEG during surgery. Instead, the BIS monitor is currently used during anesthesia, but, so far, no study has been published on the validity of the BIS in this population. However, we have started a study to compare BIS monitoring with aEEG during open heart surgery. The lack of continuous aEEG monitoring leads to a period where intraoperative asphyxia may occur unnoticed. Another limitation is the incomplete follow-up data. This is because of the concept that in our institution children with CHD will only included in a structured follow-up program if they need operation on CPB. We report here preliminary results, but we aim to continue this study to obtain more information on the effect of sedation and analgesia on aEEG and long-term neurodevelopmental outcome. Outcome at 1 year is early and higher cognitive functions cannot be assessed at this time; however, a certain correlation exists between early childhood and later cognitive function.
In conclusion, we showed that sedation with midazolam has a transient effect on the background activity in children undergoing heart surgery. Analgesia with morphine showed no influence on the aEEG amplitude but fentanyl induced a severe pathologic background pattern. The duration of this effect and the significance of these changes on outcome are not yet fully understood. Thus, more attention should be paid to the effects of sedation and analgesia when interpreting aEEG in this population to avoid misinterpretation regarding the predictive value of aEEG on neurodevelopmental outcome. In particular, the time to return to normal background pattern may be different when infants are sedated. More research is needed in this patient population to improve the interpretation of aEEG in the presence of medication, in particular regarding long-term neurodevelopmental outcome.
Abbreviations
- aEEG:
-
amplitude-integrated electroencephalogram
- BIS:
-
bispectral index
- BS:
-
burst suppression
- CHD:
-
congenital heart disease
- CLV:
-
continuous low voltage
- CPB:
-
cardiopulmonary bypass
- CNV:
-
continuous normal voltage
- SWC:
-
sleep-wake cycle
- DNV:
-
discontinuous normal voltage
- HIE:
-
hypoxic-ischemic encephalopathy
- FT:
-
flat tracing
- MDI:
-
mental developmental index
- PDI:
-
psychomotor developmental index
References
Gluckman PD, Wyatt JS, Azzopardi D, Ballard R, Edwards AD, Ferriero DM, Polin RA, Robertson CM, Thoresen M, Whitelaw A, Gunn AJ 2005 Selective head cooling with mild systemic hypothermia after neonatal encephalopathy: multicentre randomised trial. Lancet 365: 663–670
Thornberg E, Ekstrom-Jodal B 1994 Cerebral function monitoring: a method of predicting outcome in term neonates after severe perinatal asphyxia. Acta Paediatr 83: 596–601
Eken P, Toet MC, Groenendaal F, de Vries LS 1995 Predictive value of early neuroimaging, pulsed Doppler and neurophysiology in full term infants with hypoxic ischaemic encephalopathy. Arch Dis Child Fetal Neonatal Ed 73: F75–F80
Hellström-Westas L, Rosen I, Svenningsen NW 1995 Predictive value of early continuous amplitude integrated EEG recordings on outcome after severe birth asphyxia in full term infants. Arch Dis Child Fetal Neonatal Ed 72: F34–F38
al Naqeeb N, Edwards AD, Cowan FM, Azzopardi D 1999 Assessment of neonatal encephalopathy by amplitude-integrated electroencephalography. Pediatrics 103: 1263–1271
Bellinger DC, Wypij D, du Plessis AJ, Rappaport LA, Jonas RA, Wernovsky G, Newburger JW 2003 Neurodevelopmental status at eight years in children with dextro-transposition of the great arteries: the Boston Circulatory Arrest Trial. J Thorac Cardiovasc Surg 126: 1385–1396
Toet MC, Flinterman A, Laar I, Vries JW, Bennink GB, Uiterwaal CS, Bel F 2005 Cerebral oxygen saturation and electrical brain activity before, during, and up to 36 hours after arterial switch procedure in neonates without pre-existing brain damage: its relationship to neurodevelopmental outcome. Exp Brain Res 165: 343–350
van Leuven K, Groenendaal F, Toet MC, Schobben AF, Bos SA, de Vries LS, Rademaker CM 2004 Midazolam and amplitude-integrated EEG in asphyxiated full-term neonates. Acta Paediatr 93: 1221–1227
de Vries LS, Toet MC 2006 Amplitude integrated electroencephalography in the full-term newborn. Clin Perinatol 33: 619–632
Toet MC, Hellström-Westas L, Groenendaal F, Eken P, de Vries LS 1999 Amplitude integrated EEG 3 and 6 hours after birth in full term neonates with hypoxic-ischaemic encephalopathy. Arch Dis Child Fetal Neonatal Ed 81: F19–F23
Toet MC, van der Meij W, de Vries LS, Uiterwaal CS, van Huffelen KC 2002 Comparison between simultaneously recorded amplitude integrated electroencephalogram (cerebral function monitor) and standard electroencephalogram in neonates. Pediatrics 109: 772–779
Osredkar D, Toet MC, van Rooij LG, van Huffelen AC, Groenendaal F, de Vries LS 2005 Sleep-wake cycling on amplitude-integrated electroencephalography in term newborns with hypoxic-ischemic encephalopathy. Pediatrics 115: 327–332
Bayley N 1993 Bayley Scales of Infant Development. 2nd ed. The Psychological Corporation, San Antonio, TX, pp 1–374
Kuenzle C, Baenziger O, Martin E, Thun-Hohenstein L, Steinlin M, Good M, Fanconi S, Boltshauser E, Largo RH 1994 Prognostic value of early MR imaging in term infants with severe perinatal asphyxia. Neuropediatrics 25: 191–200
van Rooij LG, Toet MC, Osredkar D, van Huffelen AC, Groenendaal F, de Vries LS 2005 Recovery of amplitude integrated electroencephalographic background patterns within 24 hours of perinatal asphyxia. Arch Dis Child Fetal Neonatal Ed 90: F245–F251
ter Horst HJ, Sommer C, Bergman KA, Fock JM, van Weerden TW, Bos AF 2004 Prognostic significance of amplitude-integrated EEG during the first 72 hours after birth in severely asphyxiated neonates. Pediatr Res 55: 1026–1033
Spitzmiller RE, Phillips T, Meinzen-Derr J, Hoath SB 2007 Amplitude-integrated EEG is useful in predicting neurodevelopmental outcome in full-term infants with hypoxic-ischemic encephalopathy: a meta-analysis. J Child Neurol 22: 1069–1078
Azzopardi D, Guarino I, Brayshaw C, Cowan F, Price-Williams D, Edwards AD, Acolet D 1999 Prediction of neurological outcome after birth asphyxia from early continuous two-channel electroencephalography. Early Hum Dev 55: 113–123
Niemarkt HJ, Halbertsma FJ, Andriessen P, Bambang Oetomo S 2008 Amplitude-integrated electroencephalographic changes in a newborn induced by overdose of morphine and corrected with naloxone. Acta Paediatr 97: 132–134
Bell AH, Greisen G, Pryds O 1993 Comparison of the effects of phenobarbitone and morphine administration on EEG activity in preterm babies. Acta Paediatr 82: 35–39
Nguyen The Tich S, Vecchierini MF, Debillon T, Péréon Y 2003 Effects of sufentanil on electroencephalogram in very and extremely preterm neonates. Pediatrics 111: 123–128
Koehntop DE, Rodman JH, Brundage DM, Hegland MG, Buckley JJ 1986 Pharmacokinetics of fentanyl in neonates. Anesth Analg 65: 227–232
Greeley WJ, de Bruijn NP 1988 Changes in sufentanil pharmacokinetics within the neonatal period. Anesth Analg 67: 86–90
Meistelman C, Benhamou D, Barre J, Levron JC, Mahe V, Mazoit X, Ecoffey C 1990 Effects of age on plasma protein binding of sufentanil. Anesthesiology 72: 470–473
Marlow N, Weindling AM, Van Peer A, Heykants J 1990 Alfentanil pharmacokinetics in preterm infants. Arch Dis Child 65: 349–351
Greeley WJ, de Bruijn NP, Davis DP 1987 Sufentanil pharmacokinetics in paediatric cardiovascular patients. Anesth Analg 66: 1067–1072
Santeiro ML, Christie J, Stromquist C, Torres BA, Markowsky SJ 1997 Pharmacokinetics of continuous infusion fentanyl in newborns. J Perinatol 17: 135–139
Jacqz-Aigrain E, Burtin P 1996 Clinical pharmacokinetics of sedatives in neonates. Clin Pharmacokinet 31: 423–443
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by the Anna Muller Grocholski-Foundation and the Foundation for Scientific Research of the University of Zurich.
Rights and permissions
About this article
Cite this article
Bernet, V., Latal, B., Natalucci, G. et al. Effect of Sedation and Analgesia on Postoperative Amplitude-Integrated EEG in Newborn Cardiac Patients. Pediatr Res 67, 650–655 (2010). https://doi.org/10.1203/PDR.0b013e3181da44ba
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/PDR.0b013e3181da44ba
This article is cited by
-
Continuous electroencephalography (cEEG) in infants with congenital heart disease (CHD)
Pediatric Research (2023)
-
EEG monitoring during anesthesia in children aged 0 to 18 months: amplitude-integrated EEG and age effects
BMC Pediatrics (2022)
-
Pseudo-sawtooth pattern on amplitude-integrated electroencephalography in neonatal hypoxic–ischemic encephalopathy
Pediatric Research (2020)
-
Amplitude-integrated electroencephalography during the first 72 h after birth in neonates diagnosed prenatally with congenital heart disease
Pediatric Research (2018)
-
Impact of perinatal factors on continuous early monitoring of brain electrocortical activity in very preterm newborns by amplitude-integrated EEG
Pediatric Research (2014)