Abstract
Posthemorrhagic hydrocephalus (PHHC) represents a major complication of preterm birth. The aim of this study was to determine whether cerebrospinal fluid (CSF) levels of the pro-inflammatory cytokines IL-1β, IL-18, and interferon (IFN)-γ are altered in the CSF of preterm infants with PHHC and may serve as a marker of white matter damage (WMD). Twenty-seven preterm infants with PHHC were included in the study; 13 of them had signs of cystic WMD (cWMD) on ultrasound examinations. CSF sample 1 was obtained at first ventriculostomy, sample 2 at shunt implantation. Results were compared with a control group of 20 age-matched patients without neurologic diseases. IL-1β concentrations were elevated in CSF sample 1 of PHHC patients without WMD and in sample 1 of patients with cWMD. Concentrations of IL-18 were increased in both samples of patients without WMD and in sample 2 of patients with cWMD. CSF levels of IFN-γ were elevated in sample 1 of PHHC patients with cWMD. The pro-inflammatory cytokine IL-1β and IL-18 levels in the CSF are elevated in patients with PHHC. Higher IFN-γ levels are detected in a subgroup of patients developing cWMD, indicating its involvement in the pathogenesis of cWMD in the context of PHHC.
Similar content being viewed by others
Main
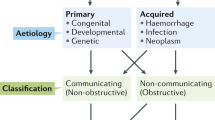
Hydrocephalus following IVH represents a major complication of preterm birth and may result in adverse neurologic outcome in later life. IVH is associated with damage to the white matter, which is exacerbated by hydrocephalus (1). Pressure, distortion, ischemia, and inflammation seem to contribute to this process (2). Although shunting CSF is often an effective treatment, it may prevent only some of the neurologic changes. The identification of mechanisms, mediators, and markers of hydrocephalus appears critical to improve the treatment and prevention of neurologic disability caused by hydrocephalus and associated WMD.
It is now widely accepted that immune and inflammatory processes take place in the brain in response to diverse insults such as infection, neurodegenerative disorders, trauma, hemorrhage, and hypoxia-ischemia (3–5). Brain inflammation is characterized by infiltration of circulating immune cells and by activation of resident cells, including microglia. These cells can express, release, and respond to inflammatory mediators. In the CNS, one of the most widely studied is the pro-inflammatory cytokine IL-1β. In the immature brain, caspase-1, which is responsible for cleavage of the pro-inflammatory cytokines IL-1β and IL-18 into their biologically active forms, seems to be an important mediator of brain injury (6). There is extensive evidence of direct involvement of IL-1β in adult and also in developmental brain injury (7–11). The next member of the IL-1 family, previously designated “IFN-γ inducing factor,” has many properties similar to IL-1β. To date, only few studies have addressed the function of IL-18 in the context of injury to the immature CNS. Data from animal experiments indicate that IL-18 has an influence on the development of WMD in the immature brain (12). IL-18 itself may induce the production of other pro-inflammatory cytokines, e.g. IFN-γ, IL-1β, and tumor necrosis factor-α (TNF-α) (13–15). IFN-γ is an important regulator of immune and inflammatory responses that activates natural killer cells and cytotoxic T cells (16) and stimulates macrophages to produce a variety of toxic substances such as reactive oxygen intermediates (ROI) (17). There is considerable evidence suggesting that IFN-γ produced by CNS infiltrating T cells contributes to the pathogenesis of myelin disorders, e.g. multiple sclerosis (18–20). Experiments on transgenic mice showed that IFN-γ is detrimental to the myelination process in the developing brain (21). Based on in vitro data of immature brain cells, a particular susceptibility of developing brain cells during the myelination process to IFN-γ can be assumed (22). Furthermore, IFN-γ has been shown to be elevated in brain sections of former preterm patients with WMD compared with healthy controls (23).
Aims of the study were to characterize the expression of pro-inflammatory IL-1β, IL-18 and IFN-γ in the CSF of patients with PHHC in comparison to infants without neurologic disease, and to investigate whether levels of these cytokines correlate with the presence of cWMD.
SUBJECTS AND METHODS
Patient selection.
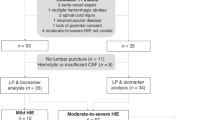
CSF was analyzed from either premature infants <32 wk gestational age with PHHC or neonates who underwent lumbar puncture for septic work-up (Table 1). All infants were treated at one of the three study centers (Department of Neonatology, University of Bonn; Department of Neonatology, CVK, Charité Universitätsmedizin Berlin; Wilhelmina Children's Hospital, University Medical Center, Utrecht) between March 1999 and September 2005.
A total of 54 ventricular CSF samples were obtained from 27 premature infants admitted for surgical treatment. In all patients, IVH was documented by ultrasound. Classification of IVH was performed in concordance with the criteria of Papile (24): grade I—germinal matrix hemorrhage with no or minimal IVH (mild); grade II (moderate) —intraventricular hemorrhage of 10–50% of ventricular area in parasagittal scan (moderate); grade III—IVH of >50% of ventricular area in parasagittal scan (severe), and as a distinct criteria apparent periventricular hemorrhagic infarction. Severe IVH was defined as either IVH grade III or IVH with apparent periventricular hemorrhagic infarction. WMD was defined as single or multiple cystic periventricular leukomalacia or gross cystic white matter defect after hemorrhagic infarction of the periventricular white matter (25). Thirteen of the 27 patients had signs of cystic WMD on ultrasound at 28 d postnatal age (Table 2).
Neurosurgical intervention was indicated by the attending physicians if one or more of the following criteria were met: Clinical symptoms of increased ICP (apnea-bradycardia, hypoventilation, seizures), bulging fontanel with widening of the sagittal suture, excessive enlargement of head circumference (>2 cm/wk, daily measurement), or signs of IVH and progressive ventricular dilatation identified by ultrasound (ventricular width >97% percentile according the criteria of Levene (26). All patients with WMD had cystic lesions, which can easily be identified using ultrasound (27).
Two CSF samples were taken from each patient for analysis: sample 1 was taken at first ventriculostomy, sample 2 was taken at the time of permanent shunt placement representing chronic stages of brain damage due to PHHC (Table 1). All CSF samples were immediately centrifuged after sampling and stored at –40°C before analysis. To exclude a confounding effect of protein denaturation after a storage time of >3 y aliquots of CSF samples of seven patients were analyzed for IL-6 concentrations for a second time (28). Correlation analysis (Pearson test; SPSS Inc., Chicago, IL) did not reveal a difference between the two measurements (correlation coefficient, 0.96; p = 0.0001).
In the control group, CSF samples were collected from 20 neonates who underwent lumbar puncture for septic work-up to rule out meningitis (Table 1). In all of these neonates, CSF leukocyte counts and total protein content were within normal ranges and bacterial cultures were negative. None of the infants suffered from neurologic deficits on clinical and ultrasound examinations. CSF was immediately centrifuged and stored at –20°C until further analysis. All CSF samples were taken for diagnostic or therapeutic purposes.
The study was performed according to the ethical guidelines of the study centers and received approval from the local ethical committees of the University of Bonn, the Charité–Universitätsmedizin Berlin, and the University Medical Center in Utrecht.
Written parental consent was obtained for all infants included in this study.
IL-18, IL-1β, and IFN-γ assays.
Concentrations of IL-18, IL-1β, and IFN-γ were determined using commercially available sandwich ELISA (R&D Systems, Wiesbaden, Germany) according to the manufacturer's instructions. The sensitivity of the assay was 12.5 pg/mL for IL-18, <1 pg/mL for IL-1β, and <8.0 pg/mL for IFN-γ. The intra-assay coefficient of variation was 5.0% for IL-18 (mean = 276 pg/mL, n = 8), 8.5% for IL-1β (mean = 18.9 pg/mL, n = 20), and 4.7% for IFN (mean = 79.2 pg/mL, n = 20). All assays were carried out in duplicate. All ELISA 96-well microtiter plates were analyzed using a microplate photometer (Dynotech MR5000, Denkendorf, Germany).
Data analysis.
For statistical analysis, the Mann-Whitney U test was used with two-sided p values to compare continuous nonparametric groups of values, as the distribution of values was non-Gaussian. Statistical analyses were processed by the use of statistical software SPSS 12.0 (SPSS Inc.).
RESULTS
Concentrations of the cytokines IL-1β, IL-18, and IFN-γ were measured in the CSF of preterm infants with PHHC with and without cWMD to characterize the expression of pro-inflammatory cytokines and to determine whether altered cytokine expression may serve as a pathogenetic marker of cystic WMD. To compare earlier stages after hemorrhage with later stages, two samples were used for analysis: sample 1 at first ventriculostomy, sample 2 at permanent shunt implantation after several weeks of CSF wash out and clearance of previously released cytokines.
In the CSF of PHHC patients without WMD (Fig. 1), IL-1β concentrations were significantly higher in sample 1 compared with controls (median 14.3 pg/mL, quartiles 8.52–19.8 versus median 1.37 pg/mL, quartiles 1.0–1.61; p < 0.01), but not in sample 2. Concentrations of IL-18 were significantly elevated in both samples of these patients (sample 1: median 90.5 pg/mL, range 34.9–122.3; sample 2: median 77.9 pg/mL, quartiles 47.2–124.8) compared with controls (median 12.5, quartiles 12.5–30.4 pg/mL, p < 0.005). In both patient samples, levels of IFN-γ did not differ from controls.
CSF cytokine levels of patients with PHHC without cWMD. Sample 1 at first ventriculostomy and sample 2 at definite shunt placement of neonates with PHHC without signs of cWMD (n = 14). Control: Neonates with CSF taken at sepsis work up for exclusion of meningitis (n = 20). In comparison to controls, levels of IL-1β were significantly higher in sample 1 (*p < 0.01) but not in sample 2; levels of IL-18 were significantly elevated in sample 1 and in sample 2 (**p < 0.005); levels of IFN-γ were not elevated in either samples. Values are median and 25th and 75th percentile (boxes) and 5th to 95th percentile (whiskers).
In the CSF of PHHC patients with cWMD (Fig. 2), IL-1β concentrations were significantly elevated in sample 1 (median 4.43, quartiles 1.0–26.4 pg/mL) compared with controls (p < 0.01) but not in sample 2. Concentrations of IL-18 were significantly elevated in sample 2 of these patients (median 22.7, quartiles 12.5–47.2 pg/mL) compared with controls (p < 0.05) but not in sample 1. In this patient group with signs of WMD, CSF levels of IFN-γ in sample 1 were significantly higher than in the control group (median 21.4 pg/mL, quartiles 12.9–52.3 versus median 8.0 pg/mL, quartiles 8.0–32.2; p < 0.05).
CSF cytokine levels of patients with PHHC with cWMD. Sample 1 at first ventriculostomy and sample 2 at definite shunt placement of neonates with PHHC and signs of cWMD (n = 13). Control: Neonates with CSF taken at sepsis work up for exclusion of meningitis (n = 20). In sample 1, levels of IL-1β and interferon-γ were significantly higher than in controls (*p < 0.01 and **p < 0.05, respectively). In sample 2, levels of IL-18 were significantly higher than in controls (**p < 0.05). Values are median and 25th and 75th percentile (boxes) and 5th to 95th percentile (whiskers).
DISCUSSION
The present study revealed elevated levels of IL-1β and IL-18 in the CSF of preterm infants with PHHC. CSF levels of IFN-γ were significantly elevated only in PHHC patients with concomitant cWMD but not in patients without cWMD.
IL-1β is one of the best described cytokines to exert pro-inflammatory actions in the brain, such as induction of fever and exacerbation of neurodegeneration (29). In rats, maternal administration of the endotoxin lipopolysaccharide led to induction of IL-1β in the fetal brain (3). It has been shown that elevated levels of IL-1β in amniotic fluid are associated with the development of white matter cysts in preterm infants (30). Moreover, CSF levels of IL-1β have been reported to be increased in preterm infants with posthemorrhagic ventricular dilatation (31). Our data confirm an association of elevated IL-1β levels in the CSF of preterm neonates with PHHC. In the first CSF samples obtained at ventriculostomy, IL-1β levels were significantly higher in PHHC patients compared with controls, regardless of whether they had cWMD or not. These data therefore extend previous findings that IL-1β is not a reliable marker for cWMD in the context of PHHC (31). In the second sample at permanent shunt implantation, IL-1β levels in PHHC patients reversed and did no longer differ from controls. Apparently, intracranial IL-1β expression is increased in rather acute stages of brain injury but does not play a role at later stages of PHHC.
In contrast to IL-1β, increased concentrations of IL-18 in PHHC patients without cWMD were detected in both the first and in the second sample. This observation is supported by animal studies showing a constant up-regulation of IL-18 expression in contrast to a short peak of IL-1β expression after hypoxic-ischemic brain injury (32). A long-term increase of IL-18 was also found in our PHHC patients with cWMD, in whom IL-18 levels were significantly elevated only in the first but not in the second sample. To date, only a few studies have addressed the function of IL-18 in the context of injuries to the immature brain. Elevated IL-18 protein concentrations have been observed in homogenated brain tissue of immature rats following exposure to supraphysiological oxygen concentrations leading to neural cell death (33). In IL-18 knock-out mice, WMD after hypoxic-ischemic injury was significantly attenuated compared with wild-type mice (12). IL-18 has moreover been shown to be elevated in the CNS during acute stages of demyelinating diseases in animal models (34) and in the serum and CSF of adults with multiple sclerosis (35). High cord blood concentrations of IL-18 seem to correlate with the development of WMD and cerebral palsy in neonates (36). The results presented here indicate that IL-18 in the CSF of preterm infants correlates with late stages of PHHC and of cWMD. However, early stages of cWMD were not associated with elevated IL-18 levels in this study.
IFN-γ seems to be the major cytokine that exerts detrimental effects on cerebral myelination. It apparently contributes to the demyelination process in adults with multiple sclerosis (18,19) and in neonatal transgenic mice (17). In vitro data indicate its direct toxic effect on premyelinating, immature oligodendrocytes (20). In this study, CSF levels of IFN-γ were significantly elevated in patients with PHHC and gross WMD but not in patients without WMD. This is in contrast to a study in which CSF levels of INF-γ in preterm infants with posthemorrhagic ventricular dilatation and WMD were not significantly elevated compared with controls (31). A reason for this difference could be that samples were obtained at a lower median postnatal age of 17 d in that study compared with 27 d in our investigations, and inflammatory processes involving IFN-γ produced by activated T-lymphocytes and/or microglia might need longer time spans to be detectable in the CSF. Our observations are confirmed by data in brain sections demonstrating specifically elevated IFN-γ expression in the presence of WMD rather than in the context of nonspecific injury such as germinal matrix hemorrhage (22). In a recent study on cytokine levels in the serum of preterm infants of <32 gestational weeks after premature rupture of membranes, elevated serial levels of IFN-γ from 6 to 72 h after birth were found to be associated with the development of WMD until the age of 40 gestational weeks (37). However, it was an objective of that study to determine whether increased circulating levels of IFN-γ also reflect elevated levels in the CSF. In a recent study by Ellison et al. (38) in premature infants with signs of WMD on MRI imaging, CSF levels of IFN-γ did not differ from controls without WMD. In theory, this might be caused by the higher sensitivity of MRI compared with ultrasound to detect mild white matter alterations. Although the majority of very preterm infants in that study had severe WMD, including ventriculomegaly or cysts, the severity of WMD in that study population seems to be comparable to that of our 13 patients with white matter lesions. Remarkably, only 2 of the 40 samples by Ellison et al. had IFN-γ concentrations above detection limit. This could be explained by different patient populations, because in that study preterm infants without other CNS diseases than WMD were analyzed, whereas the results presented here were obtained in preterm infants with signs of gross WMD in the context of PHHC.
Diagnosis of WMD was made by ultrasound, being the most common and cost-effective bedside imaging technique with high sensitivity for cystic lesions (27). Nevertheless one has to consider that ultrasound may underestimate diffuse WMD (39).
In summary, the present results indicate that not only IL-1β but also IL-18 is significantly elevated in the CSF of patients with PHHC and may play a role in inflammatory processes in this context. Interestingly, increased levels of IL-18 in the CSF are maintained over a longer period of time than IL-1β. In this analysis, IFN-γ is increased only in the CSF of PHHC patients with WMD but not in PHHC patients without WMD. IFN-γ levels in the CSF may specifically distinguish the inflammatory process taking place in cWMD from that in PHHC and serve as a pathogenetic marker of cWMD.
Abbreviations
- CSF:
-
cerebrospinal fluid
- cWMD:
-
cystic white matter damage
- IVH:
-
intraventricular hemorrhage
- PHHC:
-
posthemorrhagic hydrocephalus
- WMD:
-
white matter damage
References
Cherian S, Whitelaw A, Thoresen M, Love S 2004 The pathogenesis of neonatal post-hemorrhagic hydrocephalus. Brain Pathol 14: 305–311
Del Bigio MR 2004 Cellular damage and prevention in childhood hydrocephalus. Brain Pathol 14: 317–324
Cai Z, Pan ZL, Pang Y, Evans OB, Rhodes PG 2000 Cytokine induction in fetal rat brains and brain injury in neonatal rats after maternal lipopolysaccharide administration. Pediatr Res 47: 64–72
Sharief MK, Hentges R 1991 Association between tumor necrosis factor-alpha and disease progression in patients with multiple sclerosis. N Engl J Med 325: 467–472
Barone FC, Hillegass LM, Price WJ, White RF, Lee EV, Feuerstein GZ, Sarau HM, Clark RK, Griswold DE 1991 Polymorphonuclear leukocyte infiltration into cerebral focal ischemic tissue: myeloperoxidase activity assay and histologic verification. J Neurosci Res 29: 336–345
Liu XH, Kwon D, Schielke GP, Yang GY, Silverstein FS, Barks JD 1999 Mice deficient in interleukin-1 converting enzyme are resistant to neonatal hypoxic-ischemic brain damage. J Cereb Blood Flow Metab 19: 1099–1108
Allan SM, Tyrrell PJ, Rothwell NJ 2005 Interleukin-1 and neuronal injury. Nat Rev Immunol 5: 629–640 Review.
Lu KT, Wang YW, Yang JT, Yang YL, Chen HI 2005 Effect of interleukin-1 on traumatic brain injury-induced damage to hippocampal neurons. J Neurotrauma 22: 885–895
Hailer NP, Vogt C, Korf HW, Dehghani F 2005 Interleukin-1beta exacerbates and interleukin-1 receptor antagonist attenuates neuronal injury and microglial activation after excitotoxic damage in organotypic hippocampal slice cultures. Eur J Neurosci 21: 2347–2360
Szaflarski J, Burtrum D, Silverstein FS 1995 Cerebral hypoxia-ischemia stimulates cytokine gene expression in perinatal rats. Stroke 26: 1093–1100
Yoon BH, Jun JK, Romero R, Park KH, Gomez R, Choi JH, Kim IO 1997 Amniotic fluid inflammatory cytokines (interleukin-6, interleukin-1beta, and tumor necrosis factor-alpha), neonatal brain white matter lesions, and cerebral palsy. Am J Obstet Gynecol 177: 19–26
Hedtjarn M, Mallard C, Arvidsson P, Hagberg H 2005 White matter injury in the immature brain: role of interleukin-18. Neurosci Lett 373: 16–20
Nakamura K, Okamura H, Nagata K, Komatsu T, Tamura T 1993 Purification of a factor which provides a costimulatory signal for gamma interferon production. Infect Immun 61: 64–70
Okamura H, Tsutsui H, Komatsu T, Yutsudo M, Hakura K, Tanimoto T, Torigoe K, Okura T, Nukada Y, Hattori K 1995 Cloning of a new cytokine that induces IFN-gamma production by T cells. Nature 378: 88–91
Tsutsui H, Matsui K, Kawada N, Hyodo Y, Hayashi N, Okamura H, Higashino K, Nakanishi K 1997 IL-18 accounts for both TNF-alpha- and Fas ligand-mediated hepatotoxic pathways in endotoxin-induced liver injury in mice. J Immunol 159: 3961–3967
Degliantoni G, Murphy M, Kobayashi M, Francis MK, Perussia B, Trinchieri G 1985 Natural killer (NK) cell-derived hematopoietic colony-inhibiting activity and NK cytotoxic factor. Relationship with tumor necrosis factor and synergism with immune interferon. J Exp Med 162: 1512–1530
Schreiber GH, Schreiber RD 2003 Interferon-γ. In: Thomason AW, Lotze MT (eds.). The Cytokine Handbook, 4th Ed. Elsevier Science Ltd, London, pp 567–601
Hirsch RL, Panitch HS, Johnson KP 1985 Lymphocytes from multiple sclerosis patients produce elevated levels of gamma interferon in vitro. J Clin Immunol 5: 386–389
Panitch HS, Hirsch RL, Schindler J, Johnson KP 1987 Treatment of multiple sclerosis with gamma interferon: Exacerbations associated with activation of the immune system. Neurology 37: 1097–1102
Mana P, Linares D, Fordham S, Staykova M, Willenborg D 2006 Deleterious role of IFN gamma in a toxic model of central nervous system demyelination. Am J Pathol 168: 1464–1473
Corbin JG, Kelly D, Rath EM, Baerwald KD, Suzuki K, Popko B 1996 Targeted CNS expression of interferon-gamma in transgenic mice leads to hypomyelination, reactive gliosis, and abnormal cerebellar development. Mol Cell Neurosci 7: 354–370
Baerwald KD, Popko B 1998 Developing and mature oligodendrocytes respond differently to the immune cytokine interferon-gamma. J Neurosci Res 52: 230–239
Folkerth RD, Keefe RJ, Haynes RL, Trachtenberg FL, Volpe JJ, Kinney HC 2004 Interferon-γ expression in periventricular leukomalacia in the human brain. Brain Pathol 14: 265–274
Papile LA, Burstein J, Burstein R, Koffler H 1978 Incidence and evaluation of subependymal haemorrhage: a study of children with a birth weights less than 1,500 gM. J Pediatr 92: 529–534
Paneth N 1999 Classifying brain damage in preterm infants. J Pediatr 134: 527–529
Levene MI 1981 Measurement of the growth of the lateral ventricles in preterm infants with real-time ultrasound. Arch Dis Child 56: 900–904
Roelants-van Rijn AM, Groenendaal F, Beek FJ, Eken P, van Haastert IC, de Vries LS 2001 Parenchymal brain injury in the preterm infant: comparison of cranial ultrasound, MRI and neurodevelopmental outcome. Neuropediatrics 32: 80–89
Heep A, Stoffel-Wagner B, Bartmann P, Benseler S, Schaller C, Groneck P, Obladen M, Felderhoff-Mueser U 2004 Vascular endothelial growth factor and transforming growth factor-beta1 are highly expressed in the cerebrospinal fluid of premature infants with posthemorrhagic hydrocephalus. Pediatr Res 56: 768–774
Allan SM, Rothwell NJ. 2003 Inflammation in central nervous system injury. Philos Trans R Soc Lond B Biol Sci 358: 1669–1677 Review.
Yoon BH, Jun J, Romero R, Park K, Gomez R, Choi JH, Kim IO 1997 Amniotic fluid inflammatory cytokines (interleukin-6, interleukin-1β, and tumor necrosis factor-alpha), neonatal brain white matter lesions, and cerebral palsy. Am J Obstet Gynecol 177: 19–26
Savman K, Blennow M, Hagberg H, Tarkowski E, Thoresen M, Whitelaw A 2002 Cytokine response in cerebrospinal fluid from preterm infants with posthaemorrhagic ventricular dilatation. Acta Paediatr 91: 1357–1363
Hedtjarn M, Leverin AL, Eriksson K, Blomgren K, Mallard C, Hagberg H 2002 Interleukin-18 involvement in hypoxic-ischemic brain injury. J Neurosci 22: 5910–5919
Felderhoff-Mueser U, Sifringer M, Polley O, Dzietko M, Leineweber B, Mahler L, Baier M, Bittigau P, Obladen M, Ikonomidou C, Buhrer C 2005 Caspase-1 processed interleukins in hyperoxia-induced cell death in the developing brain. Ann Neurol 57: 50–59
Jander S, Stoll G 1998 Differential induction of interleukin-12, interleukin-18, and interleukin-1beta converting enzyme mRNA in experimental autoimmune encephalomyelitis of the Lewis rat. J Neuroimmunol 91: 93–99
Losy J, Niezgoda A 2001 IL-18 in patients with multiple sclerosis. Acta Neurol Scand 104: 171–173
Minagawa K, Tsuji Y, Ueda K, Koyama K, Tanizawa H, Okamura T, Hashimoto-Tamaoki T 2002 Possible correlation between high levels of IL-18 in the cord blood of preterm infants and neonatal development of periventricular leukomalacia and cerebral palsy. Cytokine 17: 164–170
Hansen-Pupp I, Harling S, Berg AC, Cilio C, Hellstrom-Westas L, Ley D 2005 Circulating interferon-gamma and white matter brain damage in preterm infants. Pediatr Res 58: 946–952
Ellison VJ, Mocatta TJ, Winterbourn CC, Darlow BA, Volpe JJ, Inder TE 2005 The relationship of CSF and plasma cytokine levels to cerebral white matter injury in the premature newborn. Pediatr Res 57: 282–286
Mirmiran M, Barnes PD, Keller K, Constantinou JC, Fleisher BE, Hintz SR, Ariagno RL 2004 Neonatal brain magnetic resonance imaging before discharge is better than serial cranial ultrasound in predicting cerebral palsy in very low birth weight preterm infants. Pediatrics 114: 992–998
Acknowledgements
The authors thank Evelyn Strauss for skilled technical assistance and Boris Metze for statistical support.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was supported by BMBF grant Z01ZZ0101.
Rights and permissions
About this article
Cite this article
Schmitz, T., Heep, A., Groenendaal, F. et al. Interleukin-1β, Interleukin-18, and Interferon-γ Expression in the Cerebrospinal Fluid of Premature Infants with Posthemorrhagic Hydrocephalus—Markers of White Matter Damage?. Pediatr Res 61, 722–726 (2007). https://doi.org/10.1203/pdr.0b013e31805341f1
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/pdr.0b013e31805341f1
This article is cited by
-
Pro-inflammatory cerebrospinal fluid profile of neonates with intraventricular hemorrhage: clinical relevance and contrast with CNS infection
Fluids and Barriers of the CNS (2024)
-
Posthemorrhagic hydrocephalus associates with elevated inflammation and CSF hypersecretion via activation of choroidal transporters
Fluids and Barriers of the CNS (2022)
-
Pathophysiologic mechanisms and strategies for the treatment of post-hemorrhagic hydrocephalus of prematurity
Child's Nervous System (2022)
-
Elevated CSF inflammatory markers in patients with idiopathic normal pressure hydrocephalus do not promote NKCC1 hyperactivity in rat choroid plexus
Fluids and Barriers of the CNS (2021)
-
Opportunities in posthemorrhagic hydrocephalus research: outcomes of the Hydrocephalus Association Posthemorrhagic Hydrocephalus Workshop
Fluids and Barriers of the CNS (2018)