Abstract
The present study was designed to investigate the early maturation of the brainstem regulation of the cochlear function in preterm neonates. Evoked otoacoustic emissions (EOAE) and their regulation via the medial olivocochlear efferent (MOC) reflex were investigated in a large population of preterm neonates and compared with full-term neonates and young babies from birth to 4 y and school-aged children. In 28-wk preterm neonates, EOAE were seen in the mid-frequency range. These responses extended both to the low (down to 1025 Hz) and high (up to 6152 Hz) frequency ranges at 38 wk of gestational age and remained stable up to 4 mo. At this stage, the amplitude of EOAE overlapped adult values. EOAE amplitudes then decreased to reach adult values at 3 y of age. Maturation of MOC efferents innervating the outer hair cells was investigated by studying the suppressive effect of contralateral sound on the EOAE amplitudes (MOC reflex). The first MOC responses were recorded in preterm neonates of 32–33 wk of gestational age, reaching adult-like values at 37 wk of gestational age. The maximum effect of MOC efferent activation occurred between 2000 and 4000 Hz. These results suggest that, in humans, MOC efferents mature in utero. Thus, testing the MOC reflex may have a clinical relevance to detect an abnormal development of the auditory pathways, particularly of a brainstem circuitry not explored through conventional testing.
Similar content being viewed by others
Main
The cochlea, the auditory organ of the inner ear, contains two types of mechanosensory hair cells, inner hair cells, and OHC. OHC are precisely adapted for mechanoreception, i.e. transduction of cochlear partition vibration into a bioelectrical signal. OHC electromotile properties (1) led to the concept of a “cochlear amplifier” involving active biomechanical feedback from OHC to the basilar membrane. This assumption is further supported by the cochlea's ability to produce acoustic energy, which can be easily detected by a sensitive microphone placed in the ear canal (2). The emitted responses, named evoked otoacoustic emissions (EOAE), are vulnerable to the same forms of interference that reduce or destroy OHC function (3).
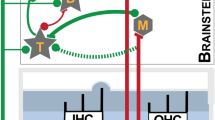
The CNS controls the motor activity of the OHC via MOC neurons, originating in the medial nuclei of the superior olivary complex. Three populations of neurons projecting from the MOC efferents to each cochlea have been shown: 1) the largest group of efferent units, which are the most responsive to ipsilateral sound stimulation, originates in the contralateral medial olivary complex and constitutes the crossed projection; 2) a group consisting of efferent units, which respond best to a contralateral sound stimulation, originates in the ipsilateral medial olivary complex and constitutes the uncrossed projection; 3) a group of efferent neurons, which respond to both ipsi- and contralateral stimulation (4). Interrupting the MOC efferents at the floor of the fourth, which severed all the efferents crossing the middle line, but spared most of the uncrossed fibers, did not affect the suppression of auditory nerve responses induced by the contralateral sound stimulation (5). However, when cuts damaged both the crossed and uncrossed fibers at the vestibulocochlear anastomosis, the suppressive effect of the contralateral sound stimulation on auditory nerve responses was eliminated. Consequently, the suppressive effect of the contralateral sound stimulation is mediated by the uncrossed part of MOC efferents. Given that similar findings were also observed on distortion product otoacoustic emissions (6), the suppressive effect of the contralateral sound stimulation had been attributed to a direct action of the uncrossed MOC efferent on OHC, which alters the mechanical nonlinearity of the cochlear partition, and consequently reduces distortion product otoacoustic emissions.
Although EOAE constitute a noninvasive test that can be easily used in humans, few studies provide data on the physiologic maturation of the MOC efferent in preterm and full-term neonates. Studying a sample of 120 full-term neonates, a suppression of the amplitude of the EOAE in 88.5% was shown (7), suggesting that MOC efferents are mature at birth. Evoked and spontaneous otoacoustic emissions recorded in preterm neonates suggested that MOC efferents mature shortly after birth, although the small size of preterm groups did not allow clear description of the time course of the maturation (8–12). The aim of this study was to investigate the early maturation of EOAE and of the MOC efferent system in statistically significant population of preterm neonates.
METHODS
Subjects.
Recordings were made under aseptic conditions in Caremeau Hospital (Nîmes, France) in the neonate pediatric department for preterm neonates and in the ENT department for babies, infants, and young adults. Informed consent was obtained from the parents of all subjects, except subjects up to 16 y old. Approval for the study was obtained from the Ethical Committee of the Centre Hospitalo-Universitaire de Nîmes. Preterm neonates with any risk factors for hearing loss were excluded from the study (e.g. a family history of hearing impairment, neurologic abnormalities, severe anoxia, fetal or neonatal infection, ototoxic treatment during gestation or after birth, or ENT malformations).
Sound-evoked otoacoustic emission recordings.
EOAE were elicited, recorded, averaged, and analyzed by otodynamic ILO88 software and hardware (Otodynamics Ltd., Herts, UK). The stimulus was an unfiltered click (intensity 80 ± 3 dB SPL, duration 80 μs, presentation rate 50/s). This particular intensity was chosen in consideration of previous works done on humans (8,13). Two hundred responses were averaged during 20 ms (the first 2.5 ms were eliminated during the data processing treatment). Two different probes were used, depending on the size of the ear canal: a classical adult probe to investigate children and young adults and a smaller baby-adapted probe to investigate preterms and full terms. In preterm neonates, babies, and children (up to 4 y old), EOAE were elicited and recorded with a ILO88 SND-type neonate probe (Otodynamics Ltd.), which is designed for very small auditory meatus and contains an attenuator to avoid high levels of stimulation due to the small size of the ear canal volume. In adults, EOAE were elicited and recorded with an ILO88 SGD-type adult probe (Otodynamics Ltd.).
Contralateral white noise stimulation.
Contralateral broad white noise was calibrated in an artificial ear by using a calibrated 1/2-inch Brüel & Kjær (Nærum, Denmark) microphone (4134) and a Brüel & Kjær calibrating amplifier (2606). Contralateral white noise stimulation was delivered by an Interacoustic audiometer AD 17 (Interacoustic, Assens, Denmark) and presented to the contralateral ear at 50 dB HL by a 2 cm diameter Sony earphone (Sony, Tokyo, Japan).
Measurements and statistics.
The EOAE amplitude was recorded according to a band of 200 Hz, yielding 23 frequency bands from 781 and 6201 Hz. Only responses 3 dB above noise level for given frequency bands were taken into account. Statistical analysis was performed using a Mann-Whitney nonparametric U test. In all cases, the criterion of significance was p < 0.01.
Experimental protocol.
Recordings were performed at least 3 d after birth to avoid fluid secretions usually found in the outer and middle ear immediately after birth. When possible, preterm neonates were recorded over a period of several weeks after birth. Preterm neonates were recorded in their cradles or incubators after feeding. Babies and children up to 2 y old were recorded during postprandial sleep. Children older than 2 y and adults were recorded awake.
In babies, children, and adult subjects, EOAE recordings took place in one session, including EOAE recording with and without contralateral white noise stimulation. In preterm neonates, recording with contralateral white noise stimulation was performed when conditions were suitable (when noise and subject's movements were reduced enough). In all cases, the mothers accompanied the babies to the test room and, occasionally, cradled their babies in their arms.
RESULTS
EOAE were recorded in 151 preterm neonates (211 ears) ranging from 28 to 38 wk of gestational age, 153 babies and young children from birth to 4 y (249 ears), and 17 school-aged children/adolescents from 5 to 18 y (36 ears). The criterion to select the subjects was a percentage of reproducibility of EOAE up to 80%. According to this criterion of reproducibility, 466 out of the 497 tested ears were included in this study. Among the 466 ears, contralateral sound suppression has been successfully performed on 214 ears (see Table 1).
Development of the EOAE—amplitude analysis.
Figure 1a shows the amplitude of EOAE as the function of ages. Note that the variability of the EOAE amplitude was approximately comparable between age groups. EOAE amplitude increases from 28 wk (12.70 dB SPL ± 1.57, n = 4) to 37 wk conceptional age (21.15 dB SPL ± 0.75, n = 19). The mean amplitude for the different groups of ages between 30 and 36 wk were 14.80 dB SPL ± 1.25 (30–31 wk, n = 23), 17.90 dB SPL ± 1.50 (32–33 wk, n = 37), 19.60 dB SPL ± 1.02 (34–35 wk, n = 33), and 21.30 dB SPL ± 0.86 (36 wk, n = 28). The mean EOAE amplitude measured in neonates between 37 wk and 2 mo of conceptional age was highest than those measured in infants and young adults (Fig. 1a). The mean values were 23.15 dB SPL ± 1.00 (n = 19), 24.30 dB SPL ± 0.87 (n = 17), 24.80 dB SPL ± 1.00 (n = 20), 24.40 dB SPL ± 1.05 (n = 54), and 24.40 dB SPL ± 1.15 (n = 62) for 37, 38, 40 wk, and 1 and 2 mo of age, respectively. After 2 mo of age, a progressive decrease of EOAE amplitude was observed. Adult-like values were noticed at 3 y of age [17.54 dB SPL ± 1.19 at 3 y (n = 26) and 16.90 dB SPL ± 0.83 in young adults (n = 36)].
Maturation of cochlear micromechanics and of the medial olivocochlear efferent system. (a) Mean EOAE amplitude as function of age of subjects (in arbitrary scale). Four populations are shown: preterm neonates (28–38 wk), babies (40 wk to 10 mo), children (1–4 y), and young adults (16–20 y). EOAE amplitude quickly increased from 28 to 38 wk, remained stable until 2 mo, and slowly decreased to adult-like values at 3 y. (b) Spectrum analysis of EOAE from preterm neonates (30–31 wk, n = 19, black circles), babies (1 mo, n = 41, gray circles), and young adults (16–20 y, n = 34, white circles). In preterms, the first responses emerging from the noise floor (in gray) were ranged in the middle of frequencies (i.e. between 2246 Hz and 4687 Hz). Responses then increased and extended both to low (up to 1025 Hz) and high (up to 6152 Hz) frequency range in 1-mo-old babies. Note the decrease of the whole spectrum amplitude in young adult EOAE. (c) Percentage of contralateral sound suppression as a function of age. Note the monotonic increase of the contralateral sound suppression that reached adult-like values at 37 wk of gestational age. (d) Spectrum analysis of EOAE responses with (white circles) and without (black circles) contralateral white noise of 50 dB SPL recorded in 1-mo-old infants (n = 41). Note that the contralateral sound suppression was significant between 2 and 4 kHz. Histogram bars and points represent mean ± SEM, *p < 0.01. All statistical comparisons (Mann-Whitney nonparametric U test) were referenced by results obtained in the young adult population.
Spectrum frequency analysis. To further investigate changes during the development of EOAE, we performed spectral analysis from 781 Hz to 6201 Hz with steps of 244 Hz (Fig. 1b). Between 28 and 31 wk of gestation, preterm neonates presented small EOAE responses centered in the middle frequency range (i.e. between 2246 and 4687 Hz). Responses increased and extended with age both to low (up to 1025 Hz) and high (up to 6152 Hz) frequency range until 38 wk (Fig. 1b). Adult-like values result from the decrease of amplitude of the whole spectrum range of EOAE amplitudes (Fig. 1b).
Development of the contralateral sound suppressive effect—amplitude analysis.
To study the functional maturation of MOC efferents, we measured EOAE in the presence of 50 dB SPL contralateral white noise stimulation. All efforts were made to limit the background noise during the recording sessions. If refitting the probe was necessary between two recordings of the same ear, the recordings were discarded. Sound-evoked MOC activation with a contralateral white noise stimulation leads to an age-dependent reduction of EOAE. At 30–31 wk of conceptual age, preterm neonates did not present significant contralateral sound suppression (0.31 dB ± 0.62) of EOAE. Mean EOAE amplitude was 14. 80 dB SPL ± 1.25 and 14.49 dB SPL ± 1.22 (n = 19) before and during contralateral white noise stimulation, respectively. The first significant contralateral sound suppression (0.11 dB SPL ± 0.42, p < 0.01) was seen in preterm neonates of 32–33 wk of conceptual age (mean EOAE amplitude 17.90 dB SPL ± 1.50 and 17.79 dB SPL ± 1.20, n = 27, before and during contralateral white noise stimulation, respectively). Among the 27 preterm neonates of 32–33 wk of conceptual age, 4 did not show EOAE reduction in the presence of contralateral white noise stimulation. At 34–35 y of age, all the subjects presented significant contralateral sound suppression that increased with age. The mean contralateral sound suppression was, respectively, 0.655 ± 0.23 and 0.875 ± 0.20 for neonates of 34–35 wk (n = 29) and 36 wk (n = 22) of conceptual age. Adult-like values (1.01 ± 0.78, n = 34) were reached at 37 wk gestational age (1.28 ± 0.24, n = 14). The mean contralateral sound suppression was 1.475 ± 0.23 (n = 14) at 38 wk, 1.51 dB ± 0.32 (n = 14) at 40 wk of conceptual age, 1.59 dB ± 0.21 (n = 41) at 1 mo, and 1.01 dB ± 0.13 in young adults (n = 34). To avoid differences due to variation of EOAE amplitude, we plot the amount of suppression as a percentage of EOAE amplitude without contralateral white noise stimulation. Figure 1c shows a monotonic increase of the suppressive effect that reached adult-like values before birth.
Spectrum frequency analysis.
To further investigate changes during the development of MOC efferent, we analyzed the effect of contralateral white noise stimulation on the spectral bands of the EOAE from 781 Hz to 6201 Hz with steps of 244 Hz. Whatever the age, contralateral white noise reduced EOAE amplitude in the same frequency range. Figure 1d showed that contralateral white noise stimulation reduced EAOEs amplitude at frequencies between 2000 and 4000 Hz in 1-mo-old babies. Note the significant suppressive effect at 2070 Hz (5.87 dB ± 0.25, p < 0.01), 3000 (3.87 dB ± 0.25, p < 0.01), and 3020 Hz (2.87 dB ± 0.25, p < 0.01).
DISCUSSION
EOAE were recorded to study the maturation of cochlear micromechanics and of the MOC efferent system in a large contingent of preterm and full-term neonates and young adults. Whereas the development of EOAE amplitude displayed a complex and long time course of maturation (up to 3 y), the MOC efferent showed fast maturation, reaching adult value at 37 wk of conceptional age.
Development of the EOAE.
Morphologic data show that the maturation of cochlear structures in human fetuses is a rapid process. By 22 wk of gestation, OHC show both an elongated shape (14) and an adult-like pattern of stereocilia (15,16). In experimental animals, where functional correlations are available, these morphologic criteria just coincide with the onset of OHC electromotility (17,18). This strongly suggests that human OHC may start their active mechanisms by wk 20–25 and explains why the first attempt to record EOAE, performed at 28–29 wk, was successful. EOAE amplitude increased up to 38 wk of conceptional age. At this stage of development, the amplitude of EOAE was much higher than in young adults. A decrease in amplitude was seen after 2 mo to reach adult-like values reached in children of 3 y. This is consistent with other studies showing that the amplitude of EOAE is higher in full-term neonates than in young adults (13). The higher amplitude measured in neonates might be explained by morphologic and functional specificities related to external and/or middle ear immaturity, such as the small volume of neonate meatus or change in the external and middle ear transfer function due to the presence of vernix caseosa in the meatus or residual amniotic fluid into the middle ear (19). In the present study, EOAE were recorded at least 3 d after birth to avoid transmission factors due to the presence of amniotic fluid in the middle ear. In any case, the presence of secretions into the meatus and/or fluid into the middle ear would result in smaller, not higher, amplitudes in neonates than in adults (20). Thus, it is unlikely that the volume of meatus may explain this phenomenon inasmuch as we used a probe specifically designed for recordings in babies, and because the calibration took into account the volume of external ear canal. Alternatively, we report that the higher amplitude measured between 37 wk of conceptional age and 2 mo is not only due to an increase of EOAE amplitude but also to the occurrence of additional frequency responses toward the low- and high-frequency range. Spontaneous otoacoustic emissions are present in <50% of adult ears, but with greater prevalence in infants and neonates (21). Although we did not measure spontaneous otoacoustic emissions, the greater prevalence of spontaneous otoacoustic emissions may explain the stronger EOAE responses in neonates.
Development of the contralateral sound suppressive effect.
Whereas EOAE can be recorded for the first time at 28 wk postconception, there was not significant contralateral sound suppression observed before 32 wk. The first significant decrease of EOAE amplitude in the presence of contralateral stimulation was seen in 32–33 wk preterm neonates. Given that EOAE are a witness of OHC active mechanisms and that EOAE suppression reflects MOC efferents activity, these results show that the onset of function of the MOC so-called “reflex” (22) is slightly delayed compared with the onset of the OHC active mechanism. This is consistent with anatomical data, as maturation of the MOC efferent OHC synapses is one of the last morphologic events occurring in the cochlea (23). Ultrastructural examination of human cochlea indicates that the first efferent synapses at OHC can be seen by 22 wk after conception (14). Similarly, MOC neurons have been identified in the human brainstem at about the same stage (24). However, a complete development of OHC with fully developed efferent synapses may take several weeks, until the third trimester of pregnancy (14,25). In the present study, the functional maturation of the MOC efferents was completely achieved in 37 wk preterm neonates, thus 2 or 3 wk earlier than other studies reporting achievement of MOC efferent maturation shortly after birth (11,12). The 2 or 3 wk difference may be related to differences in otoacoustic emission measurements, i.e. distortion product otoacoustic emissions in the study of Abdala et al. (11) or to the smaller size of preterm age groups (11,12).
Results indicate that contralateral sound suppression reduces EOAE amplitude in a frequency range of 2000–4000 Hz in all age groups tested. This is consistent with results obtained on distortion product, showing a robust suppression at 1500 Hz and 3000 Hz for all ages (11). It is not clear why MOC efferents activation only affects this narrow range of frequencies, inasmuch as morphologic studies in humans suggest that the density of OHC efferent innervation follows the general trend of the mammalian cochlea, with a decrease from base to apex (26). However, in these studies, the very base of the cochleas (coding in humans for frequencies above 5 kHz) has never been carefully observed and the results are far from quantitative. Interestingly, the frequency range of MOC inhibition corresponds to the frequency spectrum of human speech (27). One explanation may be that the MOC efferents facilitate speech perception and understanding while inhibiting nonrelevant stimuli such as background noise (28). Another explanation is related to the potential protective role of the MOC system against acoustic trauma located in the same frequency range as suggested by others (22,29).
In conclusion, our study shows that human MOC efferents have a generally adult-like effect on cochlear mechanics by 37 wk of conceptional age, and thus MOC efferents immaturity clearly exists only before term birth. Thus, testing the MOC reflex may have a clinical relevance to detect an abnormal development of the auditory pathways in neonates. In fact, this test could be useful to investigate brainstem circuitry not explored through conventional testing, in which risk of hearing loss may appear, notably in low weight babies, hemorrhage in the inner ear, bilirubin, or aminoglycoside antibiotic toxicity or cytomegalovirus infection.
Abbreviations
- ENT:
-
ear, nose, and throat
- EOAE:
-
evoked otoacoustic emissions
- MOC:
-
medial olivocochlear
- OHC:
-
outer hair cells
References
Santos-Sacchi J 2001 Cochlear physiology. In: Jahn AF, Santos-Sacchi J (eds) Physiology of the Ear, 2nd Ed. Singular/Thompson Learning, San Diego pp 357–392
Kemp DT 1986 Otoacoustic emissions, travelling waves and cochlear mechanisms. Hear Res 22: 95–104
Lonsbury-Martin B, Martin GK 2001 Otoacoustic emissions. In: Jahn AF, Santos-Sacchi J (eds) Physiology of the Ear, 2nd Ed. Singular/Thompson Learning, San Diego pp 443–480
Liberman MC, Brown MC 1986 Physiology and anatomy of single olivocochlear neurons in the cat. Hear Res 24: 17–36
Warren EH 3rd, Liberman MC 1989 Effects of contralateral sound on auditory-nerve responses. I. Contributions of cochlear efferents. Hear Res 37: 89–104
Puel JL, Rebillard G 1990 Effect of contralateral sound stimulation on the distortion product 2F1-F2: evidence that the medial efferent system is involved. J Acoust Soc Am 87: 1630–1635
Durante AS, Carvalho RM 2002 Contralateral suppression of otoacoustic emissions in neonates. Int J Audiol 41: 211–215
Berlin CI, Hood LJ, Wen H, Szabo P, Cecola RP, Rigby P, Jackson DF 1993 Contralateral suppression of non-linear click-evoked otoacoustic emissions. Hear Res 71: 1–11
Ryan S, Piron JP 1994 Functional maturation of the medial efferent olivocochlear system in human neonates. Acta Otolaryngol 114: 485–489
Hamburger A, Ari-Even Roth D, Muchnik C, Kuint J, Hildesheimer M 1998 Contralateral acoustic effect of transient evoked otoacoustic emissions in neonates. Int Tinnitus J 4: 53–57
Abdala C, Ma E, Sininger YS 1999 Maturation of medial efferent system function in humans. J Acoust Soc Am 105: 2392–2402
Morlet T, Hamburger A, Kuint J, Ari-Even Roth D, Gartner M, Muchnik C, Collet L, Hildesheimer M 2004 Assessment of medial olivocochlear system function in pre-term and full-term newborns using a rapid test of transient otoacoustic emissions. Clin Otolaryngol Allied Sci 29: 183–190
Morlet T, Collet L, Salle B, Morgon A 1993 Functional maturation of cochlear active mechanisms and of the medial olivocochlear system in humans. Acta Otolaryngol 113: 271–277
Lavigne-Rebillard M, Pujol R 1990 Auditory hair cells in human fetuses: synaptogenesis and ciliogenesis. J Electron Microsc Tech 15: 115–122
Igarashi Y 1980 Cochlea of the human fetus: a scanning electron microscope study. Arch Histol Jpn 43: 195–209
Lavigne-Rebillard M, Pujol R 1986 Development of the auditory hair cell surface in human fetuses. A scanning electron microscopy study. Anat Embryol (Berl) 174: 369–377
Pujol R, Zajic G, Dulon D, Raphael Y, Altschuler RA, Schacht J 1991 First appearance and development of motile properties in outer hair cells isolated from guinea-pig cochlea. Hear Res 57: 129–141
He DZ, Evans BN, Dallos P 1994 First appearance and development of electromotility in neonatal gerbil outer hair cells. Hear Res 78: 77–90
Buki B, Wit HP, Avan P 2000 Olivocochlear efferent vs. middle-ear contributions to the alteration of otoacoustic emissions by contralateral noise. Brain Res 852: 140–150
Keefe DH, Zhao F, Neely ST, Gorga MP, Vohr BR 2003 Ear-canal acoustic admittance and reflectance effects in human neonates. I. Predictions of otoacoustic emission and auditory brainstem responses. J Acoust Soc Am 113: 389–406
Burns EM, Campbell SL, Arehart KH 1994 Longitudinal measurements of spontaneous otoacoustic emissions in infants. J Acoust Soc Am 95: 385–394
Maison SF, Liberman MC 2000 Predicting vulnerability to acoustic injury with noninvasive assay of olivocochlear reflex strength. J Neurosci 20: 4701–4707
Pujol R, Lavigne-Rebillard M, Lenoir M 1998 Development of sensory and neural structures in the mammalian cochlea. In: Rubel EW, Popper AN, Fay RR (eds) Development of the Auditory System. Springer, New-York pp 146–192
Moore JK, Simmons DD, Guan Y 1999 The human olivocochlear system: organization and development. Audiol Neurootol 4: 311–325
Pujol R, Lavigne-Rebillard M 2003 Development and plasticity of the human auditory system. In: Luxon LM, Martini A, Furman JM, Stephens D (eds) Textbook of Audiological Medicine: Clinical Aspects of Hearing and Balance. Martin Dunitz, London pp 147–156
Nadol JB Jr 1990 Degeneration of cochlear neurons as seen in the spiral ganglion of man. Hear Res 49: 141–154
Ru P, Chi T, Shamma S 2003 The synergy between speech production and perception. J Acoust Soc Am 113: 498–515
Giard MH, Collet L, Bouchet P, Pernier J 1994 Auditory selective attention in the human cochlea. Brain Res 633: 353–356
Rajan R 1995 Involvement of cochlear efferent pathways in protective effects elicited with binaural loud sound exposure in cats. J Neurophysiol 74: 582–597
Acknowledgements
The authors thank P. Gauer for help and advice regarding administrative considerations. We also thank Dr. R. Lloyd-Faulconbridge and Dr. Marc Lenoir for helpful criticism and careful editing of the manuscript; M. Sicard, J. Iniguez, and R. Rognon for technical assistance; Professor N. Bons, Professor J. Fourcade, Dr. M.-L. Bonnet, Professor M. Mondain, and J.P. Piron for fruitful discussions; and the personnel of the departments of neonatology and pediatrics at the Caremeau Hospital of Nîmes.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chabert, R., Guitton, M., Amram, D. et al. Early Maturation of Evoked Otoacoustic Emissions and Medial Olivocochlear Reflex in Preterm Neonates. Pediatr Res 59, 305–308 (2006). https://doi.org/10.1203/01.pdr.0000196739.16060.0a
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.pdr.0000196739.16060.0a