Abstract
Among the molecular variants of human GH, the monomeric 22-kD is the predominant isoform, whereas the 20-kD is the second most abundant isoform. Because little is known on the pattern of human GH isoforms in the early postnatal period, we evaluated serum levels of 22-kD GH by an immunofluorometric assay and of 20-kD GH by an ELISA using an anti-20-kD antibody, and measured GH bioactivity with the Nb2 cell bioassay in 19 preterm neonates (gestational age, 32 ± 0.5 wk; mean ± SEM) on the fourth and 15th days of life. As control subjects, we studied 19 full-term neonates (gestational age, 39 ± 0.3 wk) on the fourth day of life and 20 healthy adults, aged 20 ± 0.3 y. Four-day-old preterm neonates showed significantly higher serum values of 20-kD GH (0.99 ± 0.14 ng/mL) than full-term neonates (0.33 ± 0.07 ng/mL;p < 0.001) and adults (0.09 ± 0.02;p < 0.0001). Likewise, 22-kD GH and GH levels by Nb2 cell bioassay were also significantly higher (p < 0.001) in preterm than in full-term neonates and young adults. A significant decrease (p < 0.01) in 20-kD, 22-kD, and Nb2-determined GH was observed in preterm neonates on the 15th day of life The percentage of the 20-kD isoform was similar in the preterm infants at the fourth and 15th day, in full-term infants, and in adults (2.7%, 2.7%, 2.8%, and 3.16%, respectively). Our results indicate that 20-kD GH serum levels change throughout life as regards total amount, but not as regards percentage.
Similar content being viewed by others
Main
Serum GH is represented mainly by the 22-kD form and by several other monomeric size variants (1, 2). The 20-kD variant, which differs from the 22-kD form in that residues 32–46 are deleted (3), is reported to be the second most common circulating isoform (4, 5) and is believed to be produced by alternative splicing (6, 7). It has recently been shown that the 22-kD and the 20-kD forms are under the pituitary drive in normal and short children and that the serum levels of the 20-kD isoform parallel those of the 22-kD after pharmacologic stimuli as well as during spontaneous secretion (8). Up to date, there is only one report (9), based on conventional RIA, concerning the secretion of these GH isoforms in the neonatal period, when the secretion of GH is peculiar. High GH serum levels are reported at birth (10, 11), particularly in the premature infant (11, 12), which decrease significantly in the following months of postnatal life (13). The aim of this study was to verify with a highly sensitive assay (ELISA) the behavior of the 20-kD variant and its relationship with the 22-kD form and GH bioactivity in a group of premature neonates in the first 2 wk of life.
METHODS
Patients
We studied 19 healthy preterm neonates (10 boys, 9 girls; 32 ± 0.5 wk gestational age) with a birth weight of 1587 ± 123 g and length of 41.2 ± 0.9 cm. For comparison, we studied 19 full-term neonates (11 boys, 8 girls; 39 ± 0.3 wk) with a birth weight of 3372 ± 106 g and length of 50 ± 0.5 cm, and 20 healthy adults (12 men, 8 women), aged 20 ± 0.3 y. The premature infants came under the practices and general management of our neonatal intensive care unit. Breast milk or a hypoallergenic formula was started on the first day of life and at the end of the second week was integrated with a preterm formula or breast milk fortifier. None of the infants received total or partial parenteral nutrition in the first 2 wk of life. All infants had normal plasma creatinine levels, normal liver function, and normal blood urea nitrogen values during the study period. All infants were discharged alive.
Study protocol
Blood samples were collected 60 min after feeding between 0800 and 0900 on d 4 and on d 15 in the premature group, and on d 4 in the full-term group. Only a basal sample after nighttime fast was obtained in the adults. Serum samples were stored at −20°C and assayed within 6 mo. Informed consent was obtained from all parents, and this study was approved by the ethical committee of our hospital. Blood was taken after feeding in the neonates because it is known that feeding represents a physiologic stimulus for GH secretion in the perinatal period (14). A stimulated GH sample was used because of the very low serum levels of the 20-kD variant and because stimuli do not influence the pattern of the GH isoforms secreted by the pituitary (15). Thus, it was possible to make a comparison with the percentage of 20-kD GH obtained in basal samples in adults, too.
The percentage of the 20-kD isoform was calculated as a percentage of the total 22-kD and 20-kD forms with the following equation:MATH The relationship between the weight and length of the neonates was expressed as ponderal index (PI; weight/length3). The values are shown as mean ± SEM. Statistical analysis was performed using the t test, Pearson correlation, multiple regression analysis, and ANOVA. A p value of <0.05 was considered significant.

Analytical methods
22-kD serum GH values.
22-kD serum GH values were measured using a time-resolved immunofluorometric assay (Delfia; LKB-Wallac, Turku, Finland) based on the direct sandwiching technique in which two MAb are directed against two separate, but unspecified, antigenic determinants on the hGH molecule. The immunofluorometric assay is specific for the 22-kD form of hGH and has a low cross-reactivity with other GH molecular variants or pituitary hormones. The intra- and interassay coefficient of variation was 2.1–5.0% and 4.2–6.3%, respectively.
GH bioactivity evaluated by Nb2-GH.
The bioassay was performed according to the method of Tanaka et al. (16) modified by Walker et al. (17) with further minor changes, as previously described (18). The intra- and interassay coefficient of variation was 6% and 7.6%, respectively.
20-kD variant.
Serum 20-kD was measured by specific ELISA. Briefly, 0.1 mL of assay buffer (150 mM PBS containing 1% BSA, 1 M NaCl, and 10 mg/L heterophilic blocking reagent; Scantibodies Laboratory, Santee, CA, U.S.A.) and 0.025 mL of standards (Mitsui Pharmaceuticals, Inc., Tokyo, Japan) or serum samples were added to monoclonal anti-20-kD antibody (anti-hGH-antibody DO5, Mitsui Pharmaceuticals) precoated microtiter plates and incubated for 2 h at room temperature. After thorough washing (0.01 M Tris-HCL, pH 8.0, containing 0.05% Tween-20), 0.1 mL (0.5 mg/L) of peroxidase-labeled anti-20-kD MAb (POD-D14, Mitsui Pharmaceuticals) was added and incubated for 2 h at room temperature. After a further washing step, 0.1 mL of substrate solution (100 mM citrate buffer containing 65 mg/L 3,3′,5,5′-tetramethylbenzidine and 4 mM H2O2, pH 3.8) was added, and the plates were incubated for 30 min at room temperature. The absorbance was read at 450 nm after interrupting the enzyme reaction with 0.1 mL of H2SO4, pH 3.8. The detection limit was 5 pg/mL, and cross-reactions with 22-kD, human prolactin, and human placental lactogen were <0.1%. Samples with 20-kD values >1 ng/mL were diluted with the zero standard.
RESULTS
At 4 d of life (Table 1), the 22-kD and 20-kD forms as well as Nb2-GH were significantly higher in preterm than in full-term neonates (p < 0.01) and in adults (p < 0.0001). At 15 d, both isoforms decreased significantly in preterm neonates, but still remained more elevated than in adults (p < 0.001). Likewise, Nb2-GH also decreased significantly in preterm infants (p < 0.05), but still remained more elevated than in adults (p < 0.0001). However, the percentage of 20-kD isoforms remained constant in preterm neonates at d 4 and 15 and did not differ in comparison with full-term infants or adults.
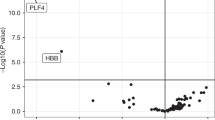
22-kD GH was positively correlated with 20-kD GH (p < 0.0001) but negatively with PI (p < 0.005) and GA (p < 0.05). 20-kD was also negatively correlated with PI (p < 0.0005) and GA (p < 0.01). Nb2-GH was positively correlated with 20-kD (p < 0.0001) but negatively correlated with PI (p < 0.01) and GA (p < 0.01;Fig. 1). Multiple regression analysis showed that the PI was the main determinant for the correlation between the 22-kD and 20-kD isoforms and the Nb2-GH. For the 20-kD isoform in particular, regression analysis gave the following result: MATH

DISCUSSION
With a highly specific antibody, we were able to directly assay the 20-kD GH variant in serum samples of preterm and full-term neonates and to correlate the results with those obtained from two other assays, one specific for the 22-kD form and the other evaluating GH bioactivity. It should be remembered that the Nb2 cell bioassay measures lactogenic, as opposed to somatogenic, GH bioactivity; however, a good correlation has been shown between the results of this assay and the auxometric findings (18–20). Both 20-kD and 22-kD serum levels at birth were shown to be significantly higher in preterm than in full-term neonates and adults and to rapidly decrease in the following weeks, as previously reported using conventional RIA (11). In only two premature babies with the lowest GA, very low levels of 20-kD and 22-kD forms were found, which both increased at 15 d of life. Furthermore, the 20-kD serum level was found to be significantly lower than that previously reported by RIA, in which circulating GH levels of up to 60% were shown (9). This dissimilarity could be explained by the different sensitivity of the antibody used. The fact that the two GH isoforms were always significantly correlated and that the percentage of the 20-kD isoform never differed suggests a common regulatory mechanism in the pituitary. Similar findings of an unchanged 20-kD percentage were recently reported by Ishikawa et al. (8) in normal and short children. The biologic activity of GH mirrored the pattern of 20-kD and 22-kD forms and was particularly related to 20-kD serum levels. Although these data must be viewed cautiously because of the low coefficient of correlation, they seem to suggest that the 20-kD form might play a role in the biologic activity of GH in the perinatal period. Even if 20-kD form serum levels are much lower than those of 22-kD GH, the somatogenic activity of the 20-kD isoform is reported to be almost the same as that of the 22-kD form (21). Nutritional state has been suggested to positively influence the non-22-kD GH isoform (22); on the other hand, Ishikawa et al. (8), by direct measurement of the 20-kD isoform, did not find such a relationship. In our study, on the contrary, we found a negative correlation between the PI and the 20-kD and 22-kD isoforms and the biologic activity of GH, suggesting a negative influence of body weight on GH secretion, similarly to what has been reported in obese prepubertal children (23).
As to the influence of GA, higher values of both isoforms were found in the more immature neonates, as previously reported by RIA (11).
In conclusion, we have shown that the 20-kD and 22-kD isoforms are secreted in a similar way during the perinatal period. However, inasmuch as differences in function (21, 24, 25) have been reported for the two isoforms as well as differences in binding affinity for the GH receptor (26), further research is needed to clarify the relative contribution to the physiologic postnatal adaption.
Abbreviations
- Nb2-GH:
-
GH bioactivity evaluated by Nb2 cell bioassay
- PI:
-
ponderal index
- GA:
-
gestational age
- hGH:
-
human GH
References
Baumann G 1991 Growth hormone heterogeneity: genes, isohormones, variants and binding proteins. Endocr Rev 12: 424–449.
Lewis UJ, Dunn JT, Bonewald LF, Seavey BK, Vanderlaan WP 1978 A naturally occurring structural variant of human growth hormone. J Biol Chem 253: 2679–2687.
Lewis UJ, Bonewald LF, Lewis LJ 1980 The 20,000-dalton variant of human growth hormone: location of the amino acid deletions. Biochem Biophys Res Commun 92: 512–516.
Baumann G 1990 Growth hormone binding proteins and various forms of growth hormone: implication for measurements. Acta Paediatr Scand Suppl 370: 72–80.
Baumann G, Winter RJ, Shaw M 1987 Circulating molecular variants of growth hormone in childhood. Pediatr Res 22: 21–22.
DeNoto FM, Moore DD, Goodman HM 1981 Human growth hormone DNA sequence and mRNA structure: possible alternative splicing. Nucleic Acids Res 9: 3719–3730.
Cooke NE, Ray J, Watson MA, Estes PA, Kuo BA, Liebhaber SA 1988 Human growth hormone gene and the highly homologous growth hormone variant gene display different splicing patterns. J Clin Invest 82: 270–275.
Ishikawa M, Yokoya S, Tachibana K, Hasegawa Y, Yasuda T, Tokuhiro E, Hashimoto Y, Tanaka T 1999 Serum levels of 20-kilodalton human growth hormone (GH) are parallel to those of 22-kilodalton human GH in normal and short children. J Clin Endocrinol Metab 84: 98–104.
King KC, Chasalow FI, Faklis EJ, Blethen SL 1994 Post-natal changes in growth hormone isoforms in preterm and term infants. letter Endocrinol Metab 1( Suppl B): 13.
Cornblath M, Parker ML, Reisner SH, Forbes AE, Daughaday WH 1965 Secretion and metabolism of growth hormone in premature and full-term infants. J Clin Endocrinol 25: 209–218.
Radetti G, Bozzola M, Paganini C, Valentini R, Gentili L, Tettoni K, Tatò L 1997 Growth hormone bioactivity and levels of growth hormone, growth hormone-binding protein, insulinlike growth factor I, and insulinlike growth factor-binding proteins in premature and full-term newborns during the first month of life. Arch Pediatr Adolesc Med 151: 170–175.
Miller JD, Wright NM, Esparza A, Jansons R, Yang HC, Hahn H, Mosier HD 1992 Spontaneous pulsatile growth hormone release in male and female premature infants. J Clin Endocrinol Metab 75: 1508–1513.
Bozzola M, Tettoni K, Locatelli F, Radetti G, Belloni, Autelli M, Zecca M, Valentini R, Severi F, Tatò L 1996 Postnatal variations of growth hormone bioactivity and growth hormone dependent factors. Arch Pediatr Adolesc Med 150: 1068–1071.
Adrian TE, Lucas A, Bloom SR, Aynsley-Green A 1983 Growth hormone response to feeding in term and preterm neonates. Acta Paediatr Scand 72: 251–254.
Baumann G, Stolar MW 1986 Molecular forms of human growth hormone secreted in vivo: non-specificity of secretory stimuli. J Clin Endocrinol Metab 62: 789–790.
Tanaka T, Shiu RPC, Gout PW, Beer CT, Noble RL, Friesen HG 1980 A new sensitive and specific bioassay for lactogenic hormones: measurement of prolactin and growth hormone in human serum. J Clin Endocrinol Metab 51: 1058–1063.
Walker A, Croze F, Friesen HG 1987 A serum-free medium for culturing lactogen dependent and autonomous Nb2 node lymphoma cells. Endocrinology 120: 2389–2397.
Bozzola M, Zecca M, Locatelli F, Radetti G, Pagani S, Autelli M, Tatò L, Chatelain P 1998 Evaluation of growth hormone bioactivity using the Nb2 cell bioassay in children with growth disorders. J Endocrinol Invest 21: 765–770.
Takahashi Y, Shirono H, Arisaka O, Takahashi K, Yagi T, Koga J, Kaji J, Okimura Y, Abe H, Tanaka T, Chihara K 1997 Biologically inactive growth hormone caused by an amino acid substitution. J Clin Invest 100: 1159–1165.
Binder G, Benz MR, Elmlinger M, Pflaum CD, Strasburger CJ, Ranke MB 1999 Reduced human growth hormone (hGH) bioactivity without a defect of the GH-1 gene in three patients with rhGH responsive growth failure. Clin Endocrinol 51: 89–95.
Lewis UJ, Markoff E, Culler FL, Hayek A, Wanderlaan WP 1987 Biological properties of the 20K-dalton variant of human growth hormone: a review. Endocrinol Jpn 34: 73–85.
Boguszewski CL, Jansson C, Boguszewski MCS, Rosberg S, Carlson B, Albertsson-Wikland K, Carlsson L 1997 Increased proportion of circulating non-22-kilodalton growth hormone isoforms in short children: a possible mechanism for growth failure. J Clin Endocrinol Metab 82: 2944–2949.
Radetti G, Bozzola M, Pasquino B, Paganini C, Aglialoro A, Livieri C, Barreca A 1998 Growth hormone bioactivity, insulin-like growth factors and their binding proteins in obese children. Metabolism 47: 1490–1493.
Lewis UJ, Singh RNP, Tutwiler GF 1981 Hyperglycemic activity of the 20,000-dalton variant of human growth hormone. Endocr Res Commun 8: 155–164.
Frigeri LG, Peterson SM, Lewis UJ 1979 The 20,000-dalton structural variant of human growth hormone: lack of some early insulin-like effects. Biochem Biophys Res Commun 91: 778–782.
Wada M, Uchida H, Ikeda M, Tsunekawa B, Naito N, Banba S, Tanaka E, Hashimoto Y, Honio M 1998 The 20-kilodalton (kDa) human growth hormone (hGH) differs from the 22-kDa hGH in the complex formation with cell surface hGH receptor and hGH-binding protein circulating in human plasma. Mol Endocrinol 12: 146–156.
Acknowledgements
The authors thank Dr. Birgit Gellersen for providing the Nb2 cell line. We also thank Karen Doyle for revising the English manuscript.
Author information
Authors and Affiliations
Additional information
Dr. Giorgio Radett, Department of Paediatrics, Regional Hospital of Bolzano, via L Boehler 5, 39100 Bolzano, Italy 39100.
Rights and permissions
About this article
Cite this article
Radetti, G., Bozzola, M., Pagani, S. et al. Circulating GH Isoforms and GH Bioactivity in Preterm Neonates. Pediatr Res 48, 244–247 (2000). https://doi.org/10.1203/00006450-200008000-00020
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200008000-00020
This article is cited by
-
Molecular heterogeneity of human GH: From basic research to clinical implications
Journal of Endocrinological Investigation (2003)