Abstract
Helicobacter pylori infection is a major cause of upper gastrointestinal disease throughout the world. Colonization begins in childhood, although little is known about its age of onset, rate, or mode of colonization. Our aim was to identify the age of acquisition of H. pylori colonization in Gambian children. A cohort of 248 Gambian children aged 3 to 45 months was studied at intervals of 3 months for 2 years, using the 13C-urea breath test, specific IgM and specific IgG serology. The prevalence of positive breath tests rose from 19% at 3 months of age to 84% by age 30 months. Elevated specific IgG and IgM antibody levels were associated with positive breath tests, although there was discrepancy between breath test results and serology, particularly IgG serology, during the 1st year of life. Neither IgG nor IgM serology could be validated as reliable diagnostic tools for infant H. pylori colonization compared with the 13C-urea breath test. Reversion to negative breath test, in association with declining specific antibody levels, occurred in 48/248 (20%) of children. On the assumption that the 13C-urea breath test is a reliable index of H. pylori colonization, we conclude that the infection is extremely common from an early age in Gambian children. Transient colonization may occur. Previous studies relying on serodiagnosis may have significantly underestimated the true early prevalence of colonization in the developing world, where the target age for intervention studies is probably early infancy.
Similar content being viewed by others
Main
Helicobacter pylori is one of the most common causes of chronic bacterial infection of mankind, and is now regarded as a major cause of upper gastrointestinal disease throughout the world (1). There is a drive to develop population level intervention strategies, which could include the use of new vaccines, to decrease the prevalence of colonization and thus prevent the development of gastroduodenal disease (2).
Colonization usually begins in childhood and, once established, may persist throughout life (3). However, little is known about the age of onset, rate, or mode of colonization by H. pylori in early life. It is well established that H. pylori-associated gastritis occurs more frequently at all ages in the developing world than in developed nations, and several recent studies have suggested that the age of colonization in communities with a high prevalence of infection may be much younger than previously suspected (4,5).
Studies relying entirely on serodiagnosis (6) often appear to describe a lower prevalence of infection in early childhood in developing nations than those using the 13C-urea breath test (4,5). The aim of this study was to use the 13C-urea breath test to measure the rate of H. pylori colonization in Gambian children, within a community that is known to have a high prevalence of infection, to establish the age of peak incidence of H. pylori colonization, and to measure the changes in specific IgG and IgM serology that accompany infant H. pylori colonization.
METHODS
A prospective longitudinal cohort study was undertaken over a 2-year period at the Medical Research Council (MRC) Dunn Nutrition Unit's Overseas Research Station in Keneba, The Gambia. The local population is rural subsistence farmers, living in large family groups, who draw water either from shallow surface wells or from communal taps served by a deep bore hole. All children aged 3-24 months residing in three villages (population approximately 2500) were enrolled after parental consent was obtained. Study protocols were approved by the Joint MRC and Gambian Government Ethical Committee, and by a meeting of village elders.
Children who were under 2 years old at the outset of the study were followed for 2 years, and all children born during the 1st of these 2 years were enrolled and followed until the end of the study period. Children were studied from age 3 months, at intervals of 3 months thereafter, coinciding wherever possible with attendance at welfare clinics. A record was made of clinic visits and all antibiotic prescriptions during the course of the study.
On test days a baseline breath sample was obtained shortly after awakening (7). A solution of 50 mg 13C-urea (99 atom % excess, Cambridge Isotopes, MA), 50 mg naturally abundant urea, 0.5 mg/kg lactulose elixir (B.P.) to detect small bowel contamination, and a test meal of 5 g glucose polymer (Polycose, Abbott Laboratories, Queenborough, U.K.) dissolved in an appropriate amount of water was given orally. Validation studies showed that neither lactulose nor Polycose test meal had a significant effect on 13C enrichment of breath. Breath samples were collected 5, 15, 30 and 60 min after administration of the solution.
Breath samples were stored in 20 mL vacutainers (Becton Dickinson, Oxford, U.K.) and transported to Cambridge, U.K. Carbon dioxide was analyzed by gas isotope-ratio mass spectroscopy (SIRA 10, VG Isotech, UK). Isotopic enrichment was expressed as Craig-corrected (8) delta (‰) relative to the international standard Pee Dee Belemnite limestone (PDB). δ‰ = (Rsample/RPDB) - 1) × 103, where R is the isotopic ratio (13C:12C) of the sample or standard.
The urea breath test was deemed positive or negative according to analysis of 13C baseline enrichment in breath 30 min after ingestion of substrate. Data sets of 13C-urea breath test results at this time point can be divided into two subpopulations, corresponding to positive and negative results (9–11). The existence of these two subpopulations within our data were sought by viewing a smoothed histogram of the data, after which the EM algorithm was used to calculate both means and variances (12), and an appropriate cut-off was determined.
Blood samples (approximately 0.5 mL) were collected from children by finger pricks. The presence of specific H. pylori IgM and IgG antibodies were detected using an ELISA (ELISA) as previously described (13). Briefly, a crude whole cell antigen was prepared from a pool of four isolates of H. pylori, two from Gambian adults, one from a British adult, and one from British child. Campylobacter sp. infections are common in West African children (14), and because of the possibility of antibodies to Campylobacter sp. cross-reacting in our assay, samples were diluted 1:100 in blocking buffer (PBS [pH 7.0] plus 0.05% [vol/vol] Tween 20 plus 1% [wt/vol] BSA [Sigma Chemical Co.]), with the addition of crude Campylobacter jejuni antigen (13), and incubated at 4°C overnight, before assay. Six control sera that covered the useful range of the assay were included on each plate. Results were expressed as OD ratios standardized to these controls. If control values fell outside the previously determined 95% confidence limits, plates were re-assayed.
IgG and IgM seropositivities were determined as follows. For the IgG ELISA, the cut off value was the OD corresponding to the 95th centile of sera from 68 Gambian children aged 1 year, who had serial negative urea breath tests since birth (0.436). In addition, sera from a previous study in The Gambia were also assayed (15), and the lowest specific IgG value measured from an H. pylori colonized adult taken as an alternative cut-off. This value was also 0.44. For the IgM ELISA, the cut off value was the 95th centile of 93 sera from Gambian children aged 3 or 6 months, all of whom had negative 13C-urea breath tests (0.44) A cut-off value of 0.44 was therefore used for both the IgG and IgM ELISAs.
RESULTS
Two hundred sixty-one children were eligible for inclusion in the study. Parental consent was withheld in 13 cases, so that 248/261 (90%) children were enrolled, and studied at intervals of 3 months. Of these, 123 were aged between 3 months and 2 years when the study began, and were followed at 3-month intervals for 2 years. The remaining 125 children were born during the 1st year of the study and followed at 3 monthly intervals until the end of the 2-year study period, by which time they were between 1 and 2 years old.
A complete set of urea breath test data were obtained in 155/248 cases (62.5%) missed one breath test and 42/248 (17%) missed more than one. A full set of blood samples was obtained in 124/248 (50%) cases, 73/248 (29.4%) missed one blood test, and 51/248 (20.6%) missed more than one blood test. One child died aged 4 months, but most missing data were due to children living away from the village for periods during the study.
The existence of two subpopulations within our 13C-urea breath test data were confirmed by viewing a smoothed histogram of the entire data set of values for baseline enrichment of 13CO2 at 30 min after ingestion of substrate. The EM algorithm was then used to calculate means and variances for both subpopulations (12), showing that the most appropriate cut-off to separate these two subpopulations was 5.5 δ ‰ relative to PDB above baseline. This value was therefore taken as our cut-off to separate positive and negative urea breath test results. Subsequent analysis of baseline enrichment of 13CO2 at 30 min after ingestion of substrate revealed that only 39/1474 results (2.6%) lay between 5 and 6 δ ‰ rel. PDB.
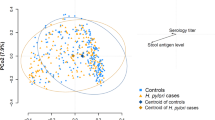
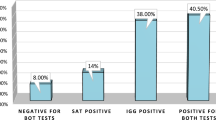
The age-related point prevalence of positive urea breath tests, and both IgG and IgM seropositivity, increased throughout the first 3 years of life, as shown by the cross-sectional data illustrated in Figure 1. In total, 1474 sets of data were available for comparison of urea breath tests with serology, which showed that both specific IgG and IgM antibody levels increased in children with positive urea breath tests (Table 1). While IgG and IgM seropositivities determined using the appropriate cut-offs were also significantly associated with breath test positivity (χ2 = 6.3 and 91.3 respectively, p < 0.0001), the sensitivity and specificity of serology when compared with the 13C-urea breath test were poor. This was particularly true when the possible confounding influence of both positive serology and positive breath tests becoming more common with increasing age was accounted for by comparing seropositivity and breath test positivity during the 1st year of life (Tables 2 and 3). The contingency table analysis shows that while there was a strong association between positive breath tests and positive serology (particularly IgM serology) at this age, there were significant numbers of infants whose serology results did not agree with the urea breath test result. When compared with the 13C-urea breath test, IgG serology had a specificity of 55%, but a sensitivity of only 25%, and IgM serology had a specificity of 62% and sensitivity of 35‰. This lack of agreement between tests among children aged less than 1 year was also suggested by the cross-sectional data shown in Figure 1.
Data from a cross-section of 220 study children over a 3-month period, showing: A, Age-related point-prevalence of positive 13C-urea breath tests. The numbers within each bar represent the number of children at each age at this time point within the study. B, Age-related point-prevalence of positive specific IgM serology. C, Age-related point-prevalence of positive specific IgG serology.
Because of this apparent discrepancy between results in infancy and early childhood, we examined the longitudinal relationship between urea breath tests and specific serology for the 85/125 children born during the study period, for whom we had a complete set of breath test data from 3 months to 1 year of age. Table 4 summarizes the change in specific IgG and IgM antibody levels among these children, divided into five groups according to the age of the first positive urea breath test. There was an increase in both IgG and IgM antibody levels with increasing age in all groups of children, the significance of which was assessed by comparing the change in specific antibody level at each age with that measured at three months of age in each child using paired t-tests. This trend did not achieve significance for IgM among children with no positive 13C-urea breath tests during their first year, but all other groups of children did show a significant rise in specific IgM levels at around the time of the first positive 13C-urea breath test (Table 4). Mean specific IgG levels did not rise with age among non-colonized children, although the gradual rise in IgG levels among other infants only achieved significance at 12 months among those first colonized at that age. A comparison between non-colonized and colonized children throughout the first year of life revealed a trend toward increased specific antibody levels (both IgG and IgM) among colonized infants, which only achieved accepted levels of significance for specific IgM antibody at age 9 months (Table 5).
There were no differences in site of residence in village, parental age or quantifiable family wealth between the 18 children who had no positive urea breath tests during their first year and other children. In three instances, children from this group of 18 came from the same family (having the same father but a different mother), and thus from the same family compound, as children who had positive breath tests from three months of age.
Within the entire cohort of 248 children, a negative urea breath test followed at least one positive test in 48/248 (20%) children. This involved a clear change from a breath test in the positive sub-population (median baseline 13C enrichment of initial positive breath test 13.07, interquartile range 7.40 to 21.09) to the negative sub-population (median baseline 13C enrichment of subsequent negative breath test 2.88, interquartile range 1.86 to 4.37). This was accompanied by a significant fall in mean specific IgG (0.65 to 0.5, p = 0.005) and IgM (0.59 to 0.52, p = 0.04) antibody levels. Although antibiotics were prescribed on 520 occasions per year to 193/248 children, there was no significant difference between antibiotic usage among the 48 children who had a negative urea breath test after a positive test and the remaining children. Breath tests became positive again during the study period in 31 of these 48 children. This second positive breath test conversion was also accompanied by a significant rise in both mean specific IgM (0.45 to 0.58, p = 0.005,) and mean IgG (0.41 to 0.48, p = 0.04) antibody levels.
DISCUSSION
This study shows that positive 13C-urea breath tests and positive IgG and IgM serology against H. pylori are common from an early age in Gambian children. Interpreting these results in the absence of direct evidence of H. pylori colonization among such young children raises some questions. The urea breath test is accepted as a sensitive and specific index of gastric urease activity, and has been widely used to diagnose H. pylori infection in all age groups, but there is little experience of its use in children aged less than two years, and no direct validation studies at this age in developing countries (4,5,16). Our data conformed to the recognized pattern of 13C-urea breath test data sets, by generating two sub-populations of results with very few values lying close to the cut-off. The use of any value between 5 and 6 δ ‰ baseline enrichment rel. PDB as a cut-off level (all in line with previous reports (4,5,9,16)), made no significant difference to the overall results, supporting the assumption that the 13C-urea breath test was detecting gastric urease activity in infants as young as three months of age.
Simultaneous measurement of breath hydrogen concentration showed no significant elevation by 30 min after ingestion of substrate, indicating that the lactulose in the test meal had not reached a fermentative bacterial population. We assumed therefore that the urea had also not reached bacterial populations in either the large or contaminated small bowel by this time. Many subjects showed a transient rise in 13C enrichment in expired breath above baseline five minutes after ingestion of substrate that was not maintained at other time points, which may have been due to oral bacterial urease activity.
It is unlikely that other bacteria cause significant gastric urea hydrolysis in this population. The only bacterial source of gastric urease that has been described from West Africa is H. pylori, which can be identified in most adult subjects from endoscopic studies (15,17). Among 16 children aged under two years who previously underwent gastroduodenoscopy in our unit in The Gambia, H. pylori was identified in 15, and among adults who have undergone endoscopy in The Gambia as part of our studies, we have failed to identify gastric H. pylori colonization in only one (15), making H. pylori the most likely source of the gastric urease activity detected by our urea breath test. Moreover positive IgG serology to H. pylori was present in 64/65 mothers that we studied in another cohort from the same community (18).
The associations between positive urea breath tests and serology among the youngest children in our study differed from that described among adults and older children (19). A specific circulating IgM response directed against H. pylori has been described in one volunteer ingestion experiment (20), although we have previously failed to find evidence of a circulating IgM antibody response against H. pylori among British children (13). IgM producing cells have been identified at an early stage of human H. pylori infection (21), and a transient circulating IgM response has been described in animal models of acute Helicobacter sp. infection (22,23). Data consistent with the detection of a transient IgM response in acute naturally acquired infection in childhood have been reported (24). It is possible that the high levels of specific IgM that we describe were also part of a transient response, detected because of the high numbers of children monitored during their initial colonization by H. pylori. It is clear from our data, however, that in keeping with most other researchers, we have been unable to validate specific IgM serology as a useful tool for the diagnosis of H. pylori colonization.
Specific circulating IgG levels were associated with positive urea breath tests during the 1st year of life, but there were substantial numbers of infants with positive IgG serology and negative breath tests, and even more with negative IgG serology and positive breath tests (Table 2). The cross-sectional data shown in Figure 1 suggest that positive IgG serology was more common in the first 6 months of life than later in infancy. The most likely explanation is that transplacentally acquired maternal IgG produced a seropositive result in uncolonized infants (18), leading to IgG seropositive children with negative urea breath tests. Passively acquired levels of specific IgG above our cut-off may not persist for long in many infants, as most children were already IgG seronegative by age 3 months (Fig. 2C), despite most Gambian adults, including their mothers being seropositive.
Our data raise the possibility that the time interval between colonization and IgG seroconversion in normal infants may be longer than that seen in adult ingestion studies (20). Although specific IgG levels rose after urea breath tests became positive in our children, the mean IgG levels for this population did not reach our serological cut-off until 9 months after the first positive urea breath test. A similar time interval between H. pylori colonization and IgG seroconversion has been described in a primate model (25).
The previously reported occurrence of H. pylori in gastric mucosal biopsies from Gambians of all ages, and the association between urea breath tests and specific serological responses described in this study, mean that the most likely explanation of our data are that the urea breath test was detecting H. pylori colonization in Gambian infants. The inferred annual incidence of H. pylori colonization, of between 50% and 75% calculated from this series of 13C-urea breath tests in 248 children, is extremely high, consistent with extensive transmission of infection between individuals, probably by a fecal-oral route (26). In many respects, this is more directly comparable to gut colonization with normal adult flora than with infection by other known enteropathogens. High levels of H. pylori colonization in early life have also been reported in other developing countries using noninvasive tests (4,5,16,27,28). Our data suggest an explanation of the apparent lower prevalence of early H. pylori colonization in developing countries, reported in studies that have relied entirely upon IgG serodiagnosis (6).
We could find no evidence that socioeconomic differences or site of residence within the village influenced H. pylori colonization of children. We found several instances where children living in the same family compound, with the same father but different mothers, were colonized from 3 months of age while their half-siblings remained free from colonization to age 1 year. This apparent difference in susceptibility to H. pylori colonization between children from different mothers apparently living in the same environment may be due to our previous observation that colonized mothers produce differing levels of breast milk anti-H. pylori IgA, high levels of which are associated with delayed infant H. pylori colonization (29).
The longitudinal data from this study show that 20% of children studied had negative 13C-urea breath tests, after at least one positive test. This observation has been described in young children in a longitudinal study from Peru (16). The changes in specific antibody levels that accompanied negative and positive breath test conversion among our children can be interpreted in two ways. Either some children had a level of gastric colonization with H. pylori that intermittently fell below that which could be detected by our indirect tests, or clearance and re-colonization occurred. Medical care of the children resulted in extensive use of antibiotics to treat infectious diseases, but there was no excess use of antibiotics (particularly of agents effective against H. pylori) during the 3-month interval between the initial positive and subsequent negative breath tests among children in whom H. pylori was apparently eradicated. Among chronically infected adults and older children, it seems that H. pylori infection is persistent, but there have been at least two reports of spontaneous resolution of short-lived colonization (13,30). A study by Guelrud et al. (31) describes endoscopically proven spontaneous clearance of H. pylori colonization during the 1st year of life. It is possible, therefore, that some cases of acute naturally acquired H. pylori colonization resolve without leading to chronic infection. Our data suggest that children who may have recovered from one episode of colonization remain vulnerable to further episodes. A similar finding has been described in rhesus monkeys, in which in addition to the expected persistent colonization following challenge, transient colonization occurred in some individuals, who remained susceptible to re-colonization (25).
H. pylori colonization of Gambian children does not appear to occur in the manner that we would have predicted, although there are striking similarities between our data and that obtained from a primate model (25). In The Gambian, a typical developing world community, colonization appears to most commonly occur in infancy, and to be a more dynamic process than hitherto appreciated. Transient colonization may occur before established long-term colonization ensues. The 13C-urea breath test needs to be validated in young children from the developing world, but assuming that it is a reliable index of gastric H. pylori colonization, for the reasons argued above, we believe that our data suggest that IgG serology is a poor guide to early colonization. Studies relying on IgG serodiagnosis may significantly underestimate the prevalence of H. pylori colonization in early childhood. A specific IgM response often accompanies colonization, but may be transient. The age at which colonization first occurs, and therefore the age group at which intervention strategies aimed at decreasing population levels of colonization should be targeted, is likely to be early infancy.
Abbreviations
- IgG:
-
IgG
- IgM:
-
IgM
- IgA:
-
Immunoglobulin A
- ELISA:
-
Enzyme-linked immunosorbant assay
- PDB:
-
Pee Dee Belemnite Limestone
References
Hunt RH 1996 The role of Helicobacter pylori in pathogenesis: the spectrum of clinical outcomes. Scand J Gastroenterol Suppl 220: 3–9
Lee A, Buck F 1996 Vaccination and mucosal responses to Helicobacter pylori infection. Aliment Pharmacol Ther 10( suppl 1): 129–138
Taylor DN, Blaser MJ 1991 The epidemiology of Helicobacter pylori infection. Epidemiol Rev 13: 42–59
Sarker SA, Rahman MM, Mahalanabis D, Bardham PK, Hildebrand P, Beglinger C, Gyr K 1995 Prevalence of Helicobacter pylori infection in infants and family contacts in a poor Bangladeshi community. Dig Dis Sci 40: 2669–2672
Goodman K, Correa P, Tenganá Aux HJ, Ramírez H, DeLany JP, Pepinosa OG, López Quiñones M, Parra TC 1996 Helicobacter pylori infection in the Colombian Andes: a population-based study of transmission pathways. Am J Epidemiol 144: 290–299
Perez-Perez GI, Taylor DN, Bodhitta L, Wongsrichanalai J, Baze WB, Dunn BE, Echeverria PD, Blaser MJ 1990 Seroprevalence of Helicobacter pylori infections in Thailand. J Infect Dis 161: 1237–1241
Weaver LT, Thomas JE, McClean P, Harding M, Coward WA 1993 Stable isotope breath tests: their use in paediatric practice. In: Jenssens J (ed) Progress in Understanding and Management of Gastrointestinal Motility Disorders. Louvain University Press, Louvain, Belgium, 156–188.
Craig H 1957 Isotopic standards for carbon and oxygen and correction factors for mass-spectrometric analysis of carbon dioxide. Geochim Cosmochim Acta 12: 133–149
Logan RPH 1996 The 13C urea breath test. In: Lee A, Mégraud F (eds) Helicobacter pylori: Techniques for Clinical Diagnosis and Basic Research. W. B. Saunders, London, 74–81.
Mion F, Rosner G, Rousseau M, Minare Y 1997 13C-urea breath test for Helicobacter pylori: cut-off point determination by cluster analysis. Clin Sci 93: 3–6
Kinderman A, Demmelmair H, Koletzko B, Wiebecke B, Koletzko S 1997 Diagnostic value and errors of the 13C-urea breath test (UBT) in children. Gut 41( suppl 1): A67 ( abstr)
Dempster AP, Laird NM, Rubin DB 1977 Maximum likelihood from incomplete data via the EM algorithm (with discussion). J R Stat Soc B 39: 1–38
Thomas JE, Whatmore AM, Barer MR, Eastham EJ, Kehoe MA 1990 Serodiagnosis of Helicobacter pylori infection in childhood. J Clin Microbiol 28: 2641–2646
Molbak K, Wested N, Hojlyng N, Scheutz F, Gottschau A, Aaby P 1994 The etiology of early childhood diarrhea: a community study from Guinea-Bissau. J Infect Dis 169: 581–587
Sullivan PB, Thomas JE, Wight DGD, Neale G, Eastham EJ, Corrah T, Lloyd-Evans N, Greenwood BM 1990 Helicobacter pylori in Gambian children with chronic diarrhoea and malnutrition. Arch Dis Child 65: 189–191
Klein PD, Gilman RH, Leonbarrua R, Diaz F, Smith EO, Graham DY 1994 The epidemiology of Helicobacter pylori in Peruvian children between 6 and 30 months of age. Am J Gastroenterol 89: 2196–2200
Holcombe C, Umar H, Lucas S B, Kaluba J 1994 Low incidence of clinically significant gastroduodenal pathology despite a high incidence of Helicobacter pylori infection. Trans R Soc Trop Med Hyg 5: 569–571
Bunn JEG, Thomas JE, Harding M, Coward WA, Weaver LT 1996 Transplacental anti-H. pylori IgG does not protect Gambian infants from colonisation. Gut 39( suppl 2): A47 ( abstr)
Thijs JC, Vanzwet AA, Thijs WJ, Oey HB, Karrenbeld A, Stellard F, Luijt DS, Meyer BC, Kleibeuker JH 1996 Diagnostic tests for Helicobacter pylori: a prospective evaluation of their accuracy, without selecting a single test as the gold standard. Am J Gastroenterol 91: 2125–2129
Morris A, Ali MR, Nicholson G, Perez-Perez G, Blaser M 1991 Long-term follow-up of voluntary ingestion of Helicobacter pylori. Ann Intern Med 114: 662–663
Sobala GM, Crabtree JE, Dixon MF, Schorah CJ, Taylor JD, Rathbone BJ, Heatley R V, Axon ATR 1991 Acute Helicobacter pylori infection: clinical features, local and systemic immune responses, gastric mucosal histology, and gastric juice ascorbic acid concentrations. Gut 32: 1415–1418
Fox JG, Blanco M, Murphy JC, Taylor NS, Lee A, Kabok Z, Pappo J 1993 Local and systemic immune responses in murine Helicobacter felis active chronic gastritis. Infect Immun 61: 2309–2315
Eaton KA, Morgan DR, Krakowka S 1990 Persistence of Helicobacter pylori in conventionalised piglets. J Infect Dis 161: 1299–1301
Blecker U, Vandenplas Y 1994 Usefulness of specific IgM in the diagnosis of Helicobacter pylori infection. Pediatrics 93: 342–343
DuBois A, Berg DE, Incecik ET, Fiala N, Hemanackah LM, Perez-Perez GI, Blaser MJ 1996 Transient and persistent experimental infection of non-human primates with Helicobacter pylori: implications for human disease. Infect Immun 64: 2885–2891
Thomas JE, Gibson GR, Darboe MK, Dale A, Weaver LT 1992 Isolation of Helicobacter pylori from human faeces. Lancet 340: 1194–1195
Glupczynski Y, Bourdeaux L, Verhas M, DePrez C, DeVos D, Devreker T 1992 Use of a urea breath test versus invasive methods to determine the prevalence of Helicobacter pylori in Zaire. Eur J Clin Microbiol Infect Dis 11: 322–327
Holcombe C, Tsimiri S, Eldridge J, Jones DM 1993 Prevalence of antibody to Helicobacter pylori in children in northern Nigeria. Trans R Soc Trop Med Hyg 87: 19–21
Thomas JE, Austin S, Dale A, MacClean P, Harding M, Coward WA, Weaver LT 1993 Specific human milk IgA antibody protects against Helicobacter pylori infection in infancy. Lancet 342: 121( letter)
Marshall B, Armstrong J, McGechie D, Glancy R 1985 Attempt to fulfill Koch's postulates for pyloric Campylobacter. Med J Aust 142: 436–439
Guelrud M, Mujica C, Jaen D, Machuca J, Essenfeld H 1994 Prevalence of Helicobacter pylori in neonates and young children undergoing ERCP for diagnosis of neonatal cholestasis. J Pediatr Gastroenterol Nutr 18: 461–464
Acknowledgements
We should like to thank Dr. P. B. Sullivan for making available data on patients who underwent upper gastrointestinal endoscopy in The Gambia, and Babah Jabateh, Mustapha Sanyang, and Lamin Jarjou, field workers from Keneba, The Gambia. Grant support: This work was supported by a grant from The Thrasher Research Fund, and by the Medical Research Council of Great Britain.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Thomas, J., Dale, A., Harding, M. et al. Helicobacter pylori Colonization in Early Life. Pediatr Res 45, 218–223 (1999). https://doi.org/10.1203/00006450-199902000-00010
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199902000-00010
This article is cited by
-
PCR-based genotyping of Helicobacter pylori of Gambian children and adults directly from biopsy specimens and bacterial cultures
Gut Pathogens (2011)
-
Prevalence of Helicobacter pylori in HIV‐infected, HAART‐naïve Ugandan children: a hospital‐based survey
Journal of the International AIDS Society (2011)
-
Helicobacter pyloriin apparently healthy children aged 0-12 years in urban Kampala, Uganda: a community-based cross sectional survey
BMC Gastroenterology (2010)
-
Helicobacter pylori infection does not influence the efficacy of iron and vitamin B12 fortification in marginally nourished Indian children
European Journal of Clinical Nutrition (2010)
-
H. pylori-infection and antibody immune response in a rural Tanzanian population
Infectious Agents and Cancer (2006)