Abstract
Bilirubin, the breakdown product of heme from erythrocytes, accumulates in the neonate in the first days of life. In recent years, the antioxidant properties of bilirubin have been demonstrated in vitro and in vivo, yet it is clear that bilirubin can be toxic to cells. To study the range in which bilirubin exerts its beneficial effect, we used erythrocytes derived from cord blood and incubated them with 0-60 mg/dL bilirubin combined with 3 g/dL BSA (bilirubin/BSA) to mimic physiologic and pathologic conditions. Oxidative stress was induced by incubating the erythrocytes with a solution of 0.6 mM H2O2 and 0.15 M CuSO4 to generate hydroxyl radical mediated injury. The loss of fluorescence of cis-parinaric acid and the degree of protein oxidation of erythrocyte membranes were assessed. Additionally, we determined erythrocyte membrane integrity, glucose-6 phosphate dehydrogenase activity, and adenosine triphosphatase activity before and after incubation with bilirubin/BSA. Incubation with bilirubin/BSA at concentrations up to 60 mg/dL and a bilirubin/BSA molar ratio of two was associated with dose-dependent protection of erythrocytes against lipid peroxidation. However, concentrations of bilirubin equal to or exceeding 30 mg/dL and a bilirubin:BSA ratio of one were associated with increased protein oxidation, decreased erythrocyte glucose-6 phosphate dehydrogenase and adenosine triphosphatase activity, and altered cell membrane integrity. We conclude that bilirubin, at physiologic concentrations, protects neonatal red blood cells against oxidative stress in the presence of physiologic concentrations of BSA but that bilirubin concentrations of 30 mg/dL or higher and a bilirubin:BSA ratio of greater than one are associated with significant cytotoxicity.
Similar content being viewed by others
Main
In the degradation of heme, biliverdin is formed by the enzyme heme oxygenase, and bilirubin is then synthesized from biliverdin by biliverdin reductase. This energy-requiring process forms a water-insoluble, lipophilic, and potentially toxic pigment from a relatively innocuous, readily excretable compound, biliverdin(1). It has been shown that both biliverdin and bilirubin have protective antioxidant effects(2). However, no accumulation of biliverdin occurs as a result of rapid conversion to bilirubin by biliverdin reductase. In recent years, investigators have described bilirubin as an important physiologic antioxidant both in vitro and in vivo. Stocker et al.(3) have shown that bilirubin is a better antioxidant than vitamin E in preventing the autooxidation of linoleic acid. We have shown that congenitally jaundiced Gunn rats are more resistant to hyperoxia than their nonjaundiced counterparts and that this difference could not be explained by an elevation of other classical antioxidants(4). Nonetheless, the literature abounds with equally convincing examples of bilirubin toxicity both in vitro and in vivo. Incubation of unconjugated bilirubin with human fetal red cells(5) and neuroblastoma cells(6) was shown to decrease Na+/K+ ATPase activity. Furthermore, clinical cases have demonstrated that high levels of unconjugated bilirubin were associated with kernicterus(7–9) and hearing loss(10,11). Can we explain the dual nature of bilirubin by suggesting that it serves as an antioxidant at lower, more physiologic levels but when beyond a given threshold is no longer beneficial?
To study the range in which bilirubin exerts its cytoprotective effect, we used erythrocytes derived from cord blood. The neonatal erythrocyte has been well studied as to antioxidant levels(12–14), membrane enzyme activity(15,16), and susceptibility to oxidant stress(13,17,18). It is also known that oxidative damage of the red blood cell can lead to cell lysis and can also affect red cell membrane function(19,20). To evaluate the oxidative susceptibility of erythrocytes and other cells, several investigators have used a fluorescent polyunsaturated fatty acid probe, cis-parinaric acid [9,11,13,15-octadecatetraenoic acid, (cis-PnA)] that can intercalate in cell membranes(21–24). When subjected to oxidative stress, this compound undergoes lipid peroxidation and degradation. Measurement of the rate of decay of this lipid probe by fluorescence spectrophotometry has been shown to correlate with the amount of lipid peroxides formed and thus can serve as a sensitive index of oxidative injury(21,22). We therefore induced oxidation in neonatal erythrocyte ghosts with H2O2 and CuSO4 to generate hydroxyl radical mediated injury. To define the range of beneficial effects of bilirubin, we assessed the effect of preincubation of erythrocytes with varying concentrations of bilirubin in the presence of albumin on oxidative injury, cell integrity, and enzyme function.
MATERIALS AND METHODS
Reagents
BSA (fraction V, fatty acid free), human serum albumin (HSA: fraction V, fatty acid free), and ethanolamine and bilirubin from bovine gall stones were purchased from Sigma. Cis-parinaric acid (cis-PnA) was purchased from Molecular Probes, Inc. Ficoll-Paque was purchased from Pharmacia LKB Biotechnology. Hydrogen peroxide (30% H2O2) and copper sulfate (CuSO4) were purchased from J.T. Baker Inc. (Phillipsburg, NJ). All reagents were of the highest grade and quality.
Neonatal Erythrocyte Ghosts
Before sampling, protocol approval was obtained from the Medical Committee for the Protection of Human Subjects in Research of Stanford University. Umbilical cord blood was collected at Lucille Packard Children's Hospital at Stanford University Medical Center. Blood samples were collected from uncomplicated term (>37 wk) vaginal or cesarean deliveries. The blood was drawn from the umbilical vessels with an 18 gauge needle and quickly aliquoted into Vacutainers containing acid citrate dextrose (ACD, Becton Dickinson) to prevent coagulation. The samples were kept on ice during transportation to the laboratory and refrigerated for up to 3 d. The hematocrit of each sample was determined using an IEC MB Centrifuge (Damon, IEC Division, Needham Heights, MA). To keep the number of erythrocytes constant in all samples, these were diluted to a concentration equivalent to a hematocrit of 45% using buffer. This value for the hematocrit was chosen because it is in the range observed in newborns. Erythrocytes were isolated from the samples by using Ficoll-Paque as per the manufacturer's instructions(25). The samples were centrifuged at 1000 × g for 20 min at 4°C. The supernatant containing the Ficoll-Paque® gradient and white blood cells was aspirated and discarded. The remaining pellet containing the packed erythrocytes was washed once with 1 × PBS (pH = 7.4) and centrifuged at 1000 × g. The supernatant was discarded, and the pellet was washed once in 5 mM sodium phosphate buffer to allow for release of the Hb. The erythrocyte ghosts thus formed were then placed on ice for 20 min and then centrifuged at 26 890 × g for 10 min at 4°C using an Ultra-centrifuge (Du Pont), as described by Steck and Kant(26).
Incubation of Erythrocyte Ghosts or Erythrocytes with Bilirubin/BSA
Bilirubin was solubilized with ethanolamine (80 mM final concentration) and was mixed with 3 g/dL BSA in buffer (bilirubin/BSA). The same final concentration of ethanolamine was used for all dilutions of bilirubin/BSA. We verified that this amount of ethanolamine (80 mM) did not have any effects on any of the assays described here. Neonatal erythrocyte ghosts (200 µL) were incubated with bilirubin/BSA at bilirubin concentrations of 0, 5, 15, 30, 45, and 60 mg/dL for 15 min at 37°C. These concentrations were chosen because they reflect bilirubin concentrations in the physiologic and pathologic range. In some experiments (G-6-PD and Na+/K+ ATPase assays), intact erythrocytes rather than ghosts were incubated with bilirubin/BSA to allow for preservation of optimal enzyme function. In all experiments, the ghosts or intact erythrocytes were centrifuged and washed with 0.1 M sodium phosphate buffer, pH 7.4, containing 0.062 M Na2HPO4 and 0.038 M NaH2PO4, H2O (buffer) to remove excess bilirubin. The number of cells in the samples was estimated using a Coulter Counter (Coulter Electronics, Inc., Hialeah, FL). To control for the possible interfering effect of the commercial bilirubin in our determination of lipid peroxidation, some erythrocyte ghost samples were incubated with BSA solutions containing bilirubin that was purified, crystallized, and dried (gift of Dr. Antony McDonagh, The Liver Center, University of California at San Francisco), as previously described(27).
Determination of Lipid Peroxidation
Cis-PnA (30 µL, 1.5 nM final concentration in sample) in buffer was equilibrated for 2 min in a 2-mL quartz cuvette. Erythrocyte ghosts (750 µL) were added and the mixture stirred for 10 min, allowing the cis-PnA to incorporate into the membranes. Lipid peroxidation of the erythrocyte membranes was initiated by adding 50 µL of 0.03% H2O2 (0.6 mM) and 5 µL of 0.25 M CuSO4 (0.15 M final concentration) 1 min after beginning the experiment. The intensity of fluorescence of cis-PnA in the sample was monitored continuously with a Hitachi F-4010 Fluorescence Spectrophotometer (Hitachi, LTD., Tokyo) at excitation 315 nm (3-nm bandpass) and emission 413 nm (10-nm bandpass) for 10 min as an index of oxidative injury to the neonatal erythrocyte membrane while continuously stirring the solution. The rate of loss of fluorescence (fluorescence decay) for each sample (CF/min) was derived from the change in fluorescence intensity of the erythrocyte/cis-PnA/bilirubin/BSA mixture over time, using two sampling intervals and averaging the rate of change of the two intervals for each sample. The rate of decay for each sample remained linear for the duration of experiments. To control for the inherent fluorescence decay of the cis-PnA probe, some erythrocyte ghost samples were incubated with cis-PnA alone and assayed for fluorescence decay without initiation of lipid peroxidation. To control for the degree of photobleaching of bilirubin/BSA on cis-PnA, the excitation beam was diverted away from the sample except for very short intervals (2-3 s) every 2.5 min, when a fluorescence reading was obtained. The slope of fluorescence decay extrapolated from three experiments at all bilirubin/BSA concentrations was compared with that obtained with constant excitation. We also verified that bilirubin/BSA in the presence or absence of H2O2 and CuSO4 did not result in any fluorescence signal.
Determination of Protein Content in Erythrocyte Ghosts
Protein content of erythrocyte samples was determined by the method of Bradford(28).
Determination of Protein Carbonyl Content in Erythrocyte Ghosts
Protein carbonyl content as an index of protein oxidation was determined in the ghosts by modification of the methods of Shacter et al.(29). Briefly, 20 µg of the erythrocyte ghost protein from each sample was resuspended in a total volume of 20 µL with addition of 0.1 M sodium phosphate buffer containing 10% SDS. The mixture was reacted with 50 nM dinitrophenyl hydrazine (DNPH) in 2 N HCl for 30 min at room temperature. The samples were then neutralized by addition of 20 nM Tris base, 30% glycerol (vol/vol), and the total sample was subjected to electrophoresis on a 12% polyacrylamide gel (Bio-Rad) and transblotted onto a PVDF membrane (Immobilon, Millipore). The blots were incubated with 1:1000 mouse monoclonal IgE anti-DNPH antibody (Sigma) and then complexed to 1:5000 rat IgE anti-mouse horseradish peroxidase-labeled antibody (Southern Biotechnologies) and visualized by chemiluminescence (ECL kit, Amersham). Controls consisted of unoxidized cell samples treated with DNPH as described (negative control), and cells were incubated with 100 µM ferric chloride and 25 mM ascorbic acid to induce oxidation and then incubated with DNPH as described (positive control). To allow for comparison of the protein carbonyl content of the different experimental samples, densitometric quantitation of the band consistently showing the strongest signal in all samples was performed. To allow for comparison between experimental groups, the signal intensity of the band was normalized to that of the sample incubated with no bilirubin. Membranes were stained with Coomassie Blue to verify equal loading of the samples.
Determination of Erythrocyte Membrane Integrity
Intact erythrocytes were incubated with 0-60 mg/dL bilirubin/BSA for 30, 60, and 120 min at room temperature as described above. Aliquots were removed at the given time intervals, placed on glass slides, visualized under phase contrast microscope at 40× magnification, and photographed with an Olympus BH-2 phase contrast microscope (Japan).
Intact erythrocytes were incubated with 0-60 mg/dL bilirubin/BSA for 60 min at room temperature. The samples were centrifuged at 100 × g for 5 min, and the supernatant was collected for determination of Hb by incubating 100 µL of the supernatant with 2 mL of Drabkin's solution (Sigma) at room temperature for 15 min(30). The samples were then read at absorbance 540 nm, and measurements were expressed as g/dL released Hb using a standard curve with human Hb (Sigma). These units were selected because Hb concentrations are typically expressed as g/dL in clinical settings.
Determination of Erythrocyte Membrane Enzyme Activity
Glucose-6-phosphate dehydrogenase activity in intact erythrocytes. G-6-PD enzyme activity was measured with a commercially available kit (Sigma diagnostics kit #345-B). This assay was performed after incubation with 0-60 mg/dL bilirubin/BSA but before initiating oxidative stress in the samples (PRE-LP). The assay was repeated after the samples were subjected to lipid peroxidation as previously described (POST-LP). The lipid peroxidation reaction was stopped after 30 min by adding 10 µL of 6 mM EDTA in sodium phosphate buffer, pH 8. PRE-LP and POST-LP values were compared at each bilirubin/BSA concentration. Cell counts were determined for each condition PRE-LP and POST-LP, and enzyme activity was expressed as U/1012 red blood cells/min, as per the manufacturer's directions.
Adenosine triphosphatase activity in erythrocytes. After incubation with bilirubin/BSA, the cells were washed twice with Tris-buffered saline (TBS), pH 7.4, to remove any residual phosphate. PRE-LP and POST-LP samples were centrifuged, and a hemolysate was obtained by adding ice-cold water to packed erythrocytes (9:1 vol/vol). 100 µL of hemolysate from PRE-LP and POST-LP samples were incubated at 37°C for 5 min with a solution containing 0.24 mM Tris base, 65 µM magnesium sulfate, 65 µM potassium chloride, 0.78 mM sodium chloride, 1.3 µM EDTA, and 68 µM ATP. The reaction was then stopped by adding 20 µL of of ice-cold trichloroacetic acid at a final concentration of 2.45 mM. Supernatants were assayed for inorganic phosphorous (Pi) as an index of Na+/K+ ATPase activity using a commercially available kit (Sigma diagnostics kit #670-C). Cell counts were determined for each condition PRE-LP and POST-LP, and Na+/K+ ATPase activity was expressed as mg/dL Pi released/1010 cells/min as described by the manufacturer.
Statistical Analysis
For comparison between experimental groups, the null hypothesis that there was no difference between group means was tested by a single factor analysis of variance (ANOVA) for multiple groups or unpaired t test for two groups using computer software (Statview 4.02, Abacus Concepts, Inc.; Berkeley, CA). Statistical significance (p < 0.05) between and within groups was determined by means of the Fischer method of multiple comparisons.
RESULTS
Decay of cis-parinaric acid. In the experimentation time interval, there was no significant loss of fluorescence of the cis-PnA probe alone (when incubated without H2O2 and CuSO4. In contrast, a rapid loss of fluorescence of cis-PnA was noted in control samples after the addition of 0.6 mM H2O2 and 0.15 M CuSO4. However, samples incubated with all concentrations of bilirubin/BSA showed a significant concentration-dependent decrease in fluorescence decay of cis-PnA with lipid peroxidation (Fig. 1). To ensure that part of the loss in fluorescence observed was not the result of photobleaching of bilirubin, the excitation light was diverted from the sample except for very short intervals (2-3 s) every 2.5 min, when a fluorescence reading was obtained. The rate of fluorescence decay extrapolated from three experiments at all bilirubin/BSA concentrations was compared with that obtained with constant excitation. No significant differences in the slopes were noted between the two modes (1.2 ± 0.6 versus 1.8 ± 0.8 CF/min, p = 0.2), indicating no significant degree of photobleaching of bilirubin during experiments.
A, loss of cis-parinaric acid fluorescence after initiation of lipid peroxidation in neonatal erythrocyte ghosts incubated with bilirubin/BSA. Following equilibration with cis-PnA, H2O2 and CuSO4 were added to the sample (arrow) to initiate oxidative injury. Rapid loss of fluorescence of cis-PnA occurred when the erythrocyte ghosts were incubated with no bilirubin/BSA, as shown in the representative example on the left, whereas slower loss of fluorescence was observed when the same sample was incubated with 30 mg/dL bilirubin/BSA, as shown on the right. Dashed arrow, note the lower initial reading of fluorescence in the presence of bilirubin/BSA. B, dose-dependent effect of increasing concentration of bilirubin/BSA (solid bars) or bilirubin/HSA (empty bars) on rate of loss of cis-PnA fluorescence in erythrocyte ghosts. Values represent the mean ± SE of determinations in cord blood derived from 9-10 different deliveries. * p < 0.05 vs no bilirubin/BSA or bilirubin/HAS. † p < 0.05 vs 5 mg/dL bilirubin/BSA or bilirubin/HAS.
Samples incubated without bilirubin/BSA had a significantly higher fluorescence reading than samples incubated with bilirubin/BSA, indicating that there was a significant absorption of fluorescence or quenching of cis-PnA by bilirubin (see example in Fig. 1A). However, this did not cause a change in the rate of cis-PnA decay over the course of the 10-min experiment. Thus, we still observed a dose-dependent significant reduction of the rate of decay of cis-PnA fluorescence compared with controls in the presence of bilirubin/BSA (Fig. 1B). Incubation of samples with commercially available bilirubin/BSA did not alter the rate of fluorescence decay of cis-PnA compared with incubation with purified bilirubin/BSA (for example, slope with 30 mg/dL bilirubin/BSA = 0.13 ± 0.02 versus 0.09 ± 0.01 CF/min for commercial bilirubin/BSA and pure bilirubin/BSA, respectively, p = 0.19). Because human and bovine albumin have differing binding properties(31), we incubated the samples with 3 g/dL HSA and bilirubin at all concentrations to obviate any effect of the albumin itself. Although incubation with bilirubin/BSA was associated with a lower rate of fluorescence decay than bilirubin mixed with 3 g/dL HSA, the decrease in fluorescence decay was similar at all bilirubin/HSA concentrations and therefore did not confound the data analysis (Fig. 1B).
Protein oxidation. Protein carbonyl groups detected by Western analysis using anti-DNP antibodies were significantly increased in the control samples incubated with BSA alone and subjected to oxidative injury compared with oxidized samples incubated with 5-30 mg/dL bilirubin/BSA (Fig. 2). In contrast, at the highest concentrations of bilirubin/BSA (45-60 mg/dL), the previously observed decreases in protein carbonyl content observed with bilirubin/BSA incubation were no longer seen (Fig. 2).
A, protein carbonyl content in erythrocyte ghosts subjected to oxidative stress. Samples were incubated with DNPH for 30 min and then subjected to Western analysis (see "Methods"). Representative example of three analyses. Control were as follows: U (negative control), unoxidized cells treated with DNPH as described; O (positive control), cells incubated overnight with 100 µM ferric chloride and 25 mM ascorbic acid to induce oxidation then subjected to DNPH incubation as described. The samples represent erythrocytes incubated for 15 min with bilirubin/BSA, then subjected to oxidative injury with 0.6 mM H2O2 and 0.15 M CuSO4. All samples on the representative blot are derived from the blood of one cord to allow for comparison. Lane 0, no bilirubin; lane 5, 5 mg/dL bilirubin/BSA; lane 15, 15 mg/dL bilirubin/BSA; lane 30, 30 mg/dL bilirubin/BSA; lane 45, 45 mg/dL bilirubin/BSA; lane 60, 60 mg/dL bilirubin/BSA. B, relative signal intensity of carbonyl content in neonatal erythrocyte ghosts incubated for 15 min with 0-60 mg/dL bilirubin/BSA, then subjected to oxidative injury with 0.6 mM H2O2 and 0.15 M CuSO4. Samples were assayed for protein carbonyl content as described in A and under "Methods," and densitometric evaluation of Western blots for each cord blood sample was obtained. Signal intensity of each sample was normalized to the densitometric value of the sample, which did not contain BSA from each blot to allow for comparison. Values represent mean ± SE of four samples for each group. * p < 0.05 vs no bilirubin.
Effect of bilirubin/BSA on cell membrane integrity. The number of erythrocyte ghosts was determined in the samples incubated with or without bilirubin/BSA (but not subjected to lipid peroxidation) to determine whether incubation with bilirubin/BSA alone would result in lysis of the neonatal erythrocytes. Although the cell counts were higher before incubation than after (3.42 ± 0.3 × 1010 cells/mL versus 1.89 ± 0.2 × 1010 cells/mL, n = 10; p < 0.05), we did not observe further cell loss after incubation with bilirubin/BSA at any concentration (cell counts ranging from 1.77 ± 0.1 to 1.99 ± 0.1 × 1010 cells/mL, n = 12 in each group).
Additionally, intact erythrocytes incubated for 30-120 min with 45 and 60 mg/dL bilirubin/BSA showed a visible increase in the number of damaged cells compared with cells incubated with other concentrations of bilirubin/BSA (Fig. 3). When the cells were exposed to 45 mg/dL bilirubin/BSA, there was an increase in numbers of deformed and shrunken erythrocytes (crenated cells), whereas the cells exposed to 60 mg/dL bilirubin/BSA for 30-120 min lost their normal biconcavity and assumed a spheroidal shape (spherocytes) (Fig. 3).
Effect of various concentrations of bilirubin/BSA on erythrocyte membrane integrity. Intact eerythrocytes were incubated with 0-60 mg/dL bilirubin/BSA for 0, 30, 60, or 120 min. An aliquot of the sample was examined under phase contrast microscope and photographed (see "Methods"). Shown here is a representative example of the erythrocytes incubated with 0-60 mg/dL bilirubin/BSA for 60 min. Panel 1, no bilirubin; panel 2, 5 mg/dL bilirubin/BSA; panel 3, 15 mg/dL bilirubin/BSA; panel 4, 30 mg/dL bilirubin/BSA; panel 5, 45 mg/dL bilirubin/BSA; panel 6, 60 mg/dL bilirubin/BSA. The samples incubated with 45 mg/dL bilirubin/BSA demonstrated increased numbers of echinocytes (arrowhead and left bottom inset), whereas the samples incubated with 60 mg/dL bilirubin/BSA were shown to have increased numbers of spherocytes (arrow and right bottom inset). Samples incubated for 30 and 120 min showed similar changes in erythrocytes morphology at all concentrations of bilirubin/BSA.
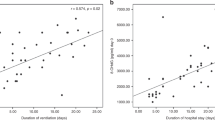
Hb release from intact erythrocytes. Incubation of the intact erythrocytes with bilirubin/BSA at concentrations of 0-30 mg/dL did not result in a significant release of Hb over the course of 1 h. However, Hb release was significantly elevated in the erythrocytes incubated with 45 and 60 mg/dL bilirubin/BSA BSA compared with all other groups (Fig. 4).
Effect of various concentrations of bilirubin/BSA on release of Hb from erythrocytes. Intact erythrocytes were incubated with 0-60 mg/dL bilirubin/BSA for 60 min. The cells were centrifuged, and the supernatant was assayed for released Hb (see "Methods"). Values represent the mean ± SE of determinations in four samples for each group. * p < 0.05 vs no bilirubin.
Glucose-6-phosphate dehydrogenase activity in erythrocytes. G-6-PD activity did not change significantly in PRE-LP compared with POST-LP cells. Incubation with 45 mg/dL and 60 mg/dL bilirubin/BSA was associated with a 25% reduction in G-6-PD activity (p = 0.0538 and 0.01, respectively). Incubation with 45 mg/dL and 60 mg/dL bilirubin/BSA coupled with lipid peroxidation further decreased G-6-PD activity of the samples to 50% of control values (Fig. 5).
G-6-PD activity in intact neonatal erythrocytes incubated with various concentrations of bilirubin/BSA. PRE-LP, incubation of erythrocytes with 0-60 mg/dL bilirubin/BSA for 30 min; POST-LP, incubation with 0-60 mg/dL for 30 min followed by oxidative injury with 0.6 mM H2O2 and 0.15 M CuSO4. The values are expressed as units of activity per 1012 erythrocytes/min ± SE of three cord blood samples. * p < 0.05 vs the PRE-LP value for samples incubated without bilirubin. † p < 0.05 vs the POST-LP value for samples incubated without bilirubin.
Adenosine triphosphatase activity and inorganic phosphorous content in erythrocytes. Lipid peroxidation for 30 min had no effect on ATPase activity. This was demonstrated by a lack of a significant change in ATPase activity in PRE-LP versus POST-LP samples. As with G-6-PD, increasing concentrations with a more than 50% decrease in ATPase activity (p = 0.02, 0.02, and 0.03, respectively). Incubation of erythrocytes with high bilirubin/BSA concentrations followed by lipid peroxidation did not further decrease ATPase activity (Fig. 6).
ATPase activity in erythrocytes incubated with various concentrations of bilirubin/BSA. PRE-LP, incubation of erythrocytes with 0-60 mg/dL bilirubin/BSA for 30 min; POST-LP, incubation with 0-60 mg/dL bilirubin/BSA for 30 min followed by oxidative injury with 0.6 mM H2O2 and 0.15 M CuSO4. Values are expressed as mg/dL Pi released per 1010 erythrocytes/min ± SE of three cord blood samples. * p < 0.05 vs the PRE-LP value for samples incubated without bilirubin. † p < 0.05 vs the POST-LP value for samples incubated without bilirubin.
DISCUSSION
We have shown that bilirubin in the presence of BSA at physiologic concentrations protects neonatal erythrocytes against oxidative stress in a dose-dependent fashion. However, with bilirubin/BSA concentrations of 30 mg/dL or higher, we observed significant erythrocyte cytotoxicity despite physiologic concentrations of albumin (3 g/dL). Therefore, injury to erythrocytes was noted when the bilirubin:BSA ratio exceeded a value of one in this model.
To determine the level of oxidative stress in cells, we measured the decay of a fluorescent probe, cis-PnA, intercalated into the erythrocyte ghost membranes. This measurement is known to be a reliable and sensitive index of oxidative injury(21,22). Nonetheless, bilirubin is also a fluorescent compound that could quench the fluorescent of cis-PnA, as it absorbs maximally at 452 nm(32) and cis-PnA emits at 413 nm(21). We therefore ensured that the wavelengths and bandpasses used in our measurements allowed for the least interference of the two compounds. Because bilirubin had significant absorption in the region of cis-PnA emission, we compared the rate of fluorescence decay rather than the intensity of fluorescence for each sample. Using this technique, we saw a dose-dependent decrease in the rate of loss of cis-PnA fluorescence associated with incubation of neonatal erythrocyte ghosts with bilirubin/BSA and bilirubin/HSA. This suggests that bilirubin can serve as an antioxidant in erythrocytes membranes and corroborates the work of others in various model systems(3,33–35).
To further expand on the role of bilirubin in antioxidant defense, we evaluated protein oxidation as measured by the protein carbonyl content of erythrocyte ghosts incubated with varying concentrations of bilirubin/BSA and subjected to oxidative stress. We demonstrated that protein oxidation was decreased by incubation of the erythrocyte ghosts with 5-30 mg/dL bilirubin/BSA. This result is in accord with previous work showing that bilirubin is protective against oxygen radical-mediated protein carbonyl formation in vitro(36,37). However, at higher concentrations of bilirubin/BSA (greater than 30 mg/dL, thereby exceeding a bilirubin:albumin ratio of one), protection against protein oxidation was lost, suggesting a threshold of cytoprotective effects of bilirubin.
We wanted to further define whether the cytoprotective effects of bilirubin would be offset by its toxic actions, especially at higher bilirubin concentrations. Because neonatal hyperbilirubinemia has been associated with red cell damage and possible hemolysis(38,39), we examined the effect of bilirubin/BSA on cell membrane integrity by determining whether incubation with bilirubin/BSA decreased intact neonatal erythrocyte cell counts and increased Hb release from intact erythrocytes. Because the Coulter counter can discriminate cell size, we assumed that lysed cells and fragments would be smaller; thus, we could exclude intact cells from the analysis by setting a higher detection threshold. We did not see any changes in cell numbers after incubation with all concentrations of bilirubin/BSA for 15 min. To investigate this further, we looked at cells under phase contrast microscope after incubation with 0-60 mg/dL bilirubin/BSA for 0-2 h to determine whether a longer exposure to bilirubin/BSA was necessary to see an effect on erythrocyte membrane integrity. Incubations with 45-60 mg/dL bilirubin/BSA for 30 min or more led to increased cell membrane damage, as evidenced by the formation of relatively large cells with membrane protrusions (echinocytes) with 45 mg/dL bilirubin/BSA and large spherical cells (spherocytes) with 60 mg/dL bilirubin/BSA. Incubations with bilirubin/BSA at the lower concentrations did not result in visible membrane damage, even with the longer exposures. We can retrospectively explain the lack of change in cell counts by the fact that damaged erythrocytes were relatively large and were likely to be counted by Coulter. Cheung et al.(38) observed that 22 mg/dL bilirubin in the presence of 1.5 g/dL human serum albumin resulted in echinocyte formation within 1 h and spherocytes within 2 h, whereas incubation with 22 mg/dL bilirubin alone immediately led to echinocyte formation and subsequent cell lysis. Furthermore, they also demonstrated that bilirubin concentrations lower than 15 mg/dL did not result in erythrocyte membrane damage. These and our findings imply that high concentrations of free bilirubin lead to alterations of the erythrocyte membrane and eventual swelling and lysis.
To further corroborate the above observations, we evaluated the release of Hb from erythrocytes incubated with bilirubin/BSA. At the lower concentrations tested (5-30 mg/dL), incubation of intact erythrocytes with bilirubin/BSA was not associated with a significant release of Hb from the cells (less than 0.25 g/dL). However, incubation with the highest concentrations of bilirubin/BSA (45-60 mg/dL, bilirubin:BSA ratio > 1) was associated with a clinically significant (close to 1 g/dL) release of Hb from erythrocytes in the absence of other injurious stimuli, further corroborating that erythrocyte membrane damage results from high concentrations of bilirubin/BSA and particularly from increased free bilirubin. Others have also evaluated the effect of bilirubin on cytotoxicity. In astrocytes and fibroblasts in culture treated with bilirubin with albumin, cell lysis as measured by lactate dehydrogenase release and mitochondrial activity was exacerbated when the bilirubin:albumin ratio exceeded 0.7, suggesting that the cytotoxic effects see in these cell types were linked to the free bilirubin concentrations(40).
We further investigated the potential cytotoxicity of bilirubin by evaluating whether incubation of intact neonatal erythrocytes with 0-60 mg/dL bilirubin/BSA would alter erythrocyte membrane enzyme activity. G-6-PD activity is found in abundance in the red cell membrane and serves to prevent oxidative injury and the resultant cell lysis(41). Clinical studies have demonstrated that certain forms of G-6-PD deficiency can exacerbate the extent of neonatal jaundice and bilirubin toxicity(42,43). In our study, incubation of intact erythrocytes with the highest concentrations of bilirubin/BSA, namely 45 and 60 mg/dL, was associated with a 25% decrease in G-6-PD activity, suggesting that high levels of bilirubin may depress G-6-PD activity. This observation also implies that measurement of G-6-PD activity in the presence of high concentrations of bilirubin could lead to falsely lowered determinations of enzyme activity. Incubation with 45 and 60 mg/dL bilirubin/BSA followed by lipid peroxidation further decreased G-6-PD activity in our samples to 50% of control values, suggesting that high levels of bilirubin may in fact exacerbate oxidative stress, although the mechanism by which this occurs is not yet clear.
Another red cell enzyme that is sensitive to oxidative damage, Na+/K+ ATPase, is important in the transport of electrolytes into cells(16). Bilirubin at a bilirubin:albumin ratio of greater than one has been shown to inhibit Na+/K+ ATPase in a neuroblastoma cell line(6), but the effects of varying doses of bilirubin on ATPase function have not been investigated in neonatal erythrocytes. We therefore measured total ATPase enzyme activity in the samples incubated with increasing concentrations of bilirubin/BSA. Higher concentrations of bilirubin/BSA (i.e. greater than 30 mg/dL bilirubin/BSA, bilirubin:BSA ratio >1) were associated with a greater than 50% decrease in ATPase activity in the neonatal erythrocytes, in agreement with findings in neuroblastoma cells(6). This decreased ATPase activity, in particular if Na+/K+ ATPase was affected, could theoretically lead to alterations in ion efflux from the erythrocytes and result in subsequent hyperkalemia in a clinical setting(16).
Although our data cannot be completely extrapolated to humans because not all experiments were performed using HSA, it is likely that qualitatively similar effects would be seen with HSA. We conclude that bilirubin, at physiologic concentrations and at a bilirubin:albumin ratio of less than one, is cytoprotective against oxidative injury in neonatal erythrocytes. However, toxic effects may outweigh beneficial effects of bilirubin at pathologic concentrations when the bilirubin:albumin ratio exceeds one.
Abbreviations
- cis-PnA :
-
cis-parinaric acid
- bilirubin/BSA :
-
bilirubin at varying concentrations in the presence of 3 g/dL BSA
- HAS :
-
human serum albumin
- G-6-PD :
-
glucose-6-phosphate dehydrogenase
- NA + /K + ATPase :
-
sodium/potassium ATPase
- DNPH :
-
dinitrophenylhydrazine
- PRE-LP :
-
before initiation of lipid peroxidation
- POST-LP :
-
after initiation of lipid peroxidation
References
Abraham NG, Lin JH, Schwartzman ML, Levere RD, Shibahara S 1988 The physiological significance of heme oxygenase. Int J Biochem 20: 543–558.
Stocker R, McDonagh AF, Glazer AN, Ames BN 1990 Antioxidant activities of bile pigments: biliverdin and bilirubin. Methods Enzymol 186: 301–309.
Stocker R, Yamamoto Y, McDonagh AF, Glazer AN, Ames BN 1987 Bilirubin is an antioxidant of possible physiologic importance. Science 235: 1043–1046.
Dennery PA, McDonagh AF, Spitz DR, Rodgers PA, Stevenson DK 1995 Hyperbilirubinemia results in reduced oxidative injury in neonatal Gunn rats exposed to hyperoxia. Free Rad Biol Med 19: 395–404.
Corchs JL, Corchs MJ, Serrani RE 1994 Unconjugated bilirubin effect on 3H-ouabain binding to human fetal red cells. Rev Esp Fisiol 50: 5–9.
Amit Y, Chan G, Fedunec S, Poznansky MJ, Schiff D 1989 Bilirubin toxicity in a neuroblastoma cell line N-115:I. effects on Na+K+ ATPase. [3H]-thymidine uptake, L-[35S]-methionine incorporation, and mitochondrial function. Pediatr Res 25: 364–368.
Johnson L 1991 Hyperbilirubinemia in the term infant: when to worry, when to treat. N Y State J Med 91: 483–489.
Penn AA, Enzmann DR, Hahn JS, Stevenson DK 1994 Kernicterus in a full term infant. Pediatrics 93: 1003–1006.
Turkel SB 1990 Autopsy findings associated with neonatal hyperbilirubinemia. Clin Perinatol 17: 381–396.
Deliac P, Demarquez JL, Barberot JP, Sandler B, Paty J 1990 Brainstem auditory evoked potentials in icteric fullterm newborns: alterations after exchange transfusion. Neuropediatrics 21: 115–118.
Vohr BR 1990 New approaches to assessing the risks of hyperbilirubinemia. Clin Perinatol 17: 293–306.
Miyake M, Miki M, Yasuda H, Ogihara T, Mino M 1991 Vitamin E and the peroxidizability of erythrocyte membranes in neonates. Free Radic Res Commun 15: 41–50.
Ripalda MJ, Rudolph N, Wong SL 1989 Developmental patterns of antioxidant defense mechanisms in human erythrocytes. Pediatr Res 26: 366–369.
Shahal Y, Zmora E, Katz M, Mazor D, Meyerstein N 1991 Effect of vitamin K on neonatal erythrocytes. Pediatr Res 29: 373–378.
Mohamed AO, Ronquist G, al Bayoumi R 1992 Increased membrane activity of glyceraldehyde 3-phosphate dehydrogenase in erythrocytes of patients with homozygous sickle cell anaemia. Clin Chim Acta 209: 189–195.
Stefano JL, Norman ME, Morales MC, Goplerud JM, Mishra OP, Delivoria-Papadopoulos M 1993 Decreased erythrocyte Na+,K(+)-ATPase activity associated with cellular potassium loss in extremely low birth infants with nonoliguric hyperkalemia. J Pediatr 122: 276–284.
Jain SK 1989 The neonatal erythrocyte and its oxidative susceptibility. Semin Hematol 26: 286–300.
Jain SK 1986 Membrane lipid peroxidation in erythrocytes of the newborn. Clin Chim Acta 161: 301–306.
Shahal Y, Bauminger ER, Zmora E, Katz M, Mazor D, Horn S, Meyerstein N 1991 Oxidative stress in newborn erythrocytes. Pediatr Res 29: 119–122.
Ogihara T, Kitagawa M, Miki M, Tamai H, Yasuda H, Okamoto R, Mino M 1991 Susceptibility of neonatal lipoproteins to oxidative stress. Pediatr Res 29: 39–45.
Kuypers FA, van den Berg JJ, Schalkwijk C, Roelofsen B, Op den Kamp JA 1987 Parinaric acid as a sensitive fluorescent probe for the determination of lipid peroxidation. Biochim Biophys Acta 921: 266–274.
Van den Berg JJ, Kuypers FA, Qju JH, Chiu D, Lubin B, Roelofsen B, Op den Kamp JA 1988 The use of cis-parinaric acid to determine lipid peroxidation in human erythrocyte membranes: comparison of normal and sickle erythrocyte membranes. Biochim Biophys Acta 944: 29–39.
Anderton JG, Thomas TH, Wilkinson R 1996 Increased susceptibility to membrane lipid peroxidation in renal failure. Nephron 74: 373–377.
Papadopoulos MC, Koumenis IL, Dugan LL, Giffard RG 1997 Vulnerability to glucose deprivation injury correlates with glutathione levels in astrocytes. Brain Res 748: 151–156.
Fotino M, Merson EJ, Allen FH 1971 Micromethod for rapid separation of lymphocytes from peripheral blood. Ann Clin Lab Sci 1: 131–133.
Steck TL, Kant JA 1974 Preparation of impermeable ghosts and inside-out vesicles from human erythrocyte membranes. Methods Enzymol 31: 172–180.
Lightner DA, Holmes DL, McDonagh AF 1996 On the acid dissociation constants of bilirubin and biliverdin: pKa values from 13C NMR spectroscopy. J Biol Chem 271: 2397–2405.
Bradford MM 1976 A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 72: 248–254.
Shacter E, Williams JA, Lim M, Levine RL 1994 Differential suspectibility of plasma proteins to oxidative modification: examination by western blot immunoassay. Free Radic Biol Med 17: 429–437.
Schoen I, Solomon M 1962 Control of blood haemoglobin determination by a simple effective method. J Clin Pathol 15: 44–48.
Blauer G, Lavie E, Silfen J 1977 Relative affinities of bilirubin for serum albumins from different species. Biochim Biophys Acta 492: 64–69.
Heirwegh KP, Brown SB 1982 Bilirubin, Vol I. CRC Press, Boca Raton, FL, 47–74.
Llesuy SF, Tomaro ML 1994 Heme oxygenase and oxidative stress: evidence of involvement of bilirubin as physiological protector against oxidative damage. Biochim Biophys Acta 1223: 9–14.
Gopinathan V, Miller NJ, Milner AD, Rice-Evans CA 1994 Bilirubin and ascorbate antioxidant activity in neonatal plasma. FEBS Lett 349: 197–200.
Wu TW, Carey D, Wu J, Sugiyama H 1991 The cytoprotective effects of bilirubin and biliverdin on rat hepatocytes and human erythrocytes and the impact of albumin. Biochem Cell Biol 69: 828–834.
Neuzil J, Stocker R 1994 Free and albumin-bound bilirubin are efficient co-antioxidants for alpha-tocopherol, inhibiting plasma and low density lipoprotein lipid peroxidation. J Biol Chem 269: 16712–16719.
Neuzil J, Stocker R 1993 Bilirubin attenuates radical-mediated damage to serum albumin. FEBS Lett 331: 281–284.
Cheung WH, Sawitsky A, Isenberg HD 1966 The effect of bilirubin on the mammalian erythrocyte. Transfusion 6: 475–486.
Olah VA, Csathy L, Karmazsin L 1991 Erythrocyte damage in newborn babies caused by hyperbilirubinaemia and hypoxia. Acta Paediatr Hung 31: 357–364.
Chuniaud L, Dessante M, Chantoux F, Blondeau JP, Francon J, Trivin F 1996 Cytotoxicity of bilirubin for human fibroblasts and rat astrocytes in culture: effect of the ratio of bilirubin to serum albumin. Clin Chim Acta 256: 103–114.
Liu TZ, Lin TF, Hung IJ, Wei JS, Chiu DT 1994 Enhanced susceptibility of erythrocytes deficient in glucose-6-phosphate dehydrogenase to alloxan/glutathione-induced decrease in red cell deformability. Life Sci 55:L55–L60.
Slusher TM, Vreman HJ, McLaren DW, Lewison LJ, Brown AK, Stevenson DK 1995 Glucose-6-phosphate dehydrogenase deficiency and carboxyhemoglobin concentrations associated with bilirubin-related morbidity and death in Nigerian infants. J Pediatr 126: 102–108.
Valaes T 1994 Severe neonatal jaundice associated with glucose-6-phosphate dehydrogenase deficiency: pathogenesis and global epidemiology. Acta Paediatr Suppl 394: 58–76.
Acknowledgements
The authors are indebted to Dr. Antony McDonagh for his thoughtful review of the manuscript and for his generous gift of purified bilirubin and to Dr. David K. Stevenson for his helpful editorial comments. We also thank Drs. Franz Kuypers and Jeroen Van den Berg for their technical assistance with the measurement of cis-parinaric acid, Drs. Karen Becker and David Bieber for their invaluable assistance with phase contrast microscopy, and Ronald J. Wong for his assistance in collecting the cord blood samples.
Author information
Authors and Affiliations
Additional information
This work was supported in part by grant HL52701 from the National Institutes of Health (Heart Lung Blood Institute) (P. Dennery).
Rights and permissions
About this article
Cite this article
Mireles, L., Lum, M. & Dennery, P. Antioxidant and Cytotoxic Effects of Bilirubin on Neonatal Erythrocytes. Pediatr Res 45, 355–362 (1999). https://doi.org/10.1203/00006450-199903000-00011
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199903000-00011
This article is cited by
-
Unconjugated bilirubin is correlated with the severeness and neurodevelopmental outcomes in neonatal hypoxic-ischemic encephalopathy
Scientific Reports (2023)
-
Changes in bilirubin in infants with hypoxic–ischemic encephalopathy
European Journal of Pediatrics (2018)
-
Effect of long-term intake of aspartame on serum biochemical parameters and erythrocyte oxidative stress biomarkers in rats
Comparative Clinical Pathology (2015)
-
Lipid peroxidation, DNA damage and total antioxidant status in neonatal hyperbilirubinemia
Journal of Perinatology (2014)
-
Total serum bilirubin levels during the first 2 days of life and subsequent neonatal morbidity in very low birth weight infants: a retrospective review
European Journal of Pediatrics (2012)