Abstract
Background:
There has been a recent proposal to change the grading system of prostate cancer into a five-tier grade grouping system. The prognostic impact of this has been demonstrated in regards only to biochemical recurrence-free survival (bRFS) with short follow-up (3 years).
Methods:
Between 1990 and 2013, 847 consecutive men were treated with definitive external beam radiation therapy at a single academic center. To validate the new grade grouping system, bRFS, distant metastases-free survival (DMFS) and prostate cancer-specific survival (PCSS) were calculated. Adjusted Kaplan–Meier and multivariable Cox regression analyses were performed to assess the independent impact of the new grade grouping system. Discriminatory analyses were performed to compare the commonly used three-tier Gleason score system (6, 7 and 8–10) to the new system.
Results:
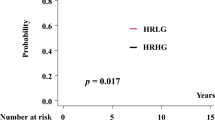
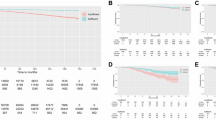
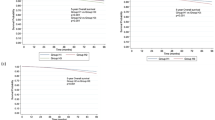
The median follow-up of our cohort was 88 months. The 5-grade groups independently validated differing risks of bRFS (group 1 as reference; adjusted hazard ratio (aHR) 1.35, 2.16, 1.79 and 3.84 for groups 2–5, respectively). Furthermore, a clear stratification was demonstrated for DMFS (aHR 2.03, 3.18, 3.62 and 13.77 for groups 2–5, respectively) and PCSS (aHR 3.00, 5.32, 6.02 and 39.02 for groups 2–5, respectively). The 5-grade group system had improved prognostic discrimination for all end points compared with the commonly used three-tiered system (that is, Gleason score 6, 7 and 8–10).
Conclusions:
In a large independent radiotherapy cohort with long-term follow-up, we have validated the bRFS benefit of the proposed five-tier grade grouping system. Furthermore, we have demonstrated that the system is highly prognostic for DMFS and PCSS. Grade group 5 had markedly worse outcomes for all end points, and future work is necessary to improve outcomes in these patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
NCCN Clinical Practice Guidelines in Oncology: Prostate Cancer 2016. Available at http://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf (date last accessed 1 February 2016).
Chan TY, Partin AW, Walsh PC, Epstein JI . Prognostic significance of Gleason score 3+4 versus Gleason score 4+3 tumor at radical prostatectomy. Urology 2000; 56: 823–827.
Khoddami SM, Shariat SF, Lotan Y, Saboorian H, McConnell JD, Sagalowsky AI et al. Predictive value of primary Gleason pattern 4 in patients with Gleason score 7 tumours treated with radical prostatectomy. BJU Int 2004; 94: 42–46.
Stark JR, Perner S, Stampfer MJ, Sinnott JA, Finn S, Eisenstein AS et al. Gleason score and lethal prostate cancer: does 3+4=4+3? J Clin Oncol 2009; 27: 3459–3464.
Zumsteg ZS, Spratt DE, Pei I, Zhang Z, Yamada Y, Kollmeier M et al. A new risk classification system for therapeutic decision making with intermediate-risk prostate cancer patients undergoing dose-escalated external-beam radiation therapy. Eur Urol 2013; 64: 895–902.
Tollefson MK, Leibovich BC, Slezak JM, Zincke H, Blute ML . Long-term prognostic significance of primary Gleason pattern in patients with Gleason score 7 prostate cancer: impact on prostate cancer specific survival. J Urol 2006; 175: 547–551.
Spratt DE, Zumsteg Z, Ghadjar P, Pangasa M, Pei X, Fine SW et al. Prognostic importance of Gleason 7 disease among patients treated with external beam radiation therapy for prostate cancer: results of a detailed biopsy core analysis. Int J Radiat Oncol Biol Phys 2013; 85: 1254–1261.
Cheng L, Koch MO, Juliar BE, Daggy JK, Foster RS, Bihrle R et al. The combined percentage of Gleason patterns 4 and 5 is the best predictor of cancer progression after radical prostatectomy. J Clin Oncol 2005; 23: 2911–2917.
Jackson W, Hamstra DA, Johnson S, Zhou J, Foster B, Foster C et al. Gleason pattern 5 is the strongest pathologic predictor of recurrence, metastasis, and prostate cancer-specific death in patients receiving salvage radiation therapy following radical prostatectomy. Cancer 2013; 119: 3287–3294.
Pierorazio PM, Guzzo TJ, Han M, Bivalacqua TJ, Epstein JI, Schaeffer EM et al. Long-term survival after radical prostatectomy for men with high Gleason sum in pathologic specimen. Urology 2010; 76: 715–721.
Sabolch A, Feng FY, Daignault-Newton S, Halverson S, Blas K, Phelps L et al. Gleason pattern 5 is the greatest risk factor for clinical failure and death from prostate cancer after dose-escalated radiation therapy and hormonal ablation. Int J Radiat Oncol Biol Phys 2011; 81: e351–e360.
Tsao CK, Gray KP, Nakabayashi M, Evan C, Kantoff PW, Huang J et al. Patients with biopsy Gleason 9 and 10 prostate cancer have significantly worse outcomes compared to patients with Gleason 8 disease. J Urol 2015; 194: 91–97.
Pierorazio PM, Walsh PC, Partin AW, Epstein JI . Prognostic Gleason grade grouping: data based on the modified Gleason scoring system. BJU Int 2013; 111: 753–760.
Epstein JI, Zelefsky MJ, Sjoberg DD, Nelson JB, Egevad L, Magi-Galluzzi C et al. A Contemporary prostate cancer grading system: a validated alternative to the Gleason score. Eur Urol 2015; 69: 428–435.
Roach M 3rd, Hanks G, Thames H Jr., Schellhammer P, Shipley WU, Sokol GH et al. Defining biochemical failure following radiotherapy with or without hormonal therapy in men with clinically localized prostate cancer: recommendations of the RTOG-ASTRO Phoenix Consensus Conference. Int J Radiat Oncol Biol Phys 2006; 65: 965–974.
Nieto FJ, Coresh J . Adjusting survival curves for confounders: a review and a new method. Am J Epidemiol 1996; 143: 1059–1068.
Epstein JI, Allsbrook WC Jr., Amin MB, Egevad LL, Committee IG . The 2005 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma. Am J Surg Pathol 2005; 29: 1228–1242.
Gleason DF . Histologic grading of prostate cancer: a perspective. Hum Pathol 1992; 23: 273–279.
Eggener SE, Scardino PT, Walsh PC, Han M, Partin AW, Trock BJ et al. Predicting 15-year prostate cancer specific mortality after radical prostatectomy. J Urol 2011; 185: 869–875.
Stephenson AJ, Kattan MW, Eastham JA, Bianco FJ Jr., Yossepowitch O, Vickers AJ et al. Prostate cancer-specific mortality after radical prostatectomy for patients treated in the prostate-specific antigen era. J Clin Oncol 2009; 27: 4300–4305.
D'Amico AV, Chen MH, Renshaw AA, Loffredo B, Kantoff PW . Risk of prostate cancer recurrence in men treated with radiation alone or in conjunction with combined or less than combined androgen suppression therapy. J Clin Oncol 2008; 26: 2979–2983.
Stephenson AJ, Scardino PT, Kattan MW, Pisansky TM, Slawin KM, Klein EA et al. Predicting the outcome of salvage radiation therapy for recurrent prostate cancer after radical prostatectomy. J Clin Oncol 2007; 25: 2035–2041.
Zhou P, Chen MH, McLeod D, Carroll PR, Moul JW, D'Amico AV . Predictors of prostate cancer-specific mortality after radical prostatectomy or radiation therapy. J Clin Oncol 2005; 23: 6992–6998.
Pound CR, Partin AW, Eisenberger MA, Chan DW, Pearson JD, Walsh PC . Natural history of progression after PSA elevation following radical prostatectomy. JAMA 1999; 281: 1591–1597.
Huynh MA, Chen MH, Wu J, Braccioforte MH, Moran BJ, D'Amico AV . Gleason score 3+5 or 5+3 versus 4+4 prostate cancer: the risk of death. Eur Urol 2015; 69: 976–979.
Mahal BA, Muralidhar V, Chen YW, Choueiri TK, Hoffman KE, Hu JC et al. Gleason score 5+3=8 prostate cancer: much more like Gleason score 9? BJU Int, e-pub ahead of print 24 July 2015; doi: 10.1111/bju.13239.
Epstein JI, Egevad L, Amin MB, Delahunt B, Srigley JR, Humphrey PA et al The 2014 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason grading of prostatic carcinoma: definition of grading patterns and proposal for a new grading system. Am J Surg Pathol 2016; 40: 244–252.
Hanks GE, Pajak TF, Porter A, Grignon D, Brereton H, Venkatesan V et al. Phase III trial of long-term adjuvant androgen deprivation after neoadjuvant hormonal cytoreduction and radiotherapy in locally advanced carcinoma of the prostate: the Radiation Therapy Oncology Group Protocol 92-02. J Clin Oncol 2003; 21: 3972–3978.
Spratt DE, Evans MJ, Davis BJ, Doran MG, Lee MX, Shah N et al. Androgen receptor upregulation mediates radioresistance after ionizing radiation. Cancer Res 2015; 75: 4688–4696.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
DES was supported by the Prostate Cancer Foundation Young Investigator Award. RM was supported by the Prostate Cancer Foundation Young Investigator Award. SAT served on the advisory boards of: Medivation/Astellas and Janssen; and received grant funding from: A. Alfred Taubman Medical Research Institute. FYF served on the advisory boards of: Medivation/Astellas, GenomeDx, Nanostring and Celgene; and received grant funding from: Varian, Medivation/Astellas and Celgene. TMM served on the advisory boards of: MDxHealth and Myriad Genetics; received research funding from: MDxHealth and Myriad Genetics; and was supported by the Prostate Cancer Foundation Young Investigator Award and by the A. Alfred Taubman Medical Research Institute. HMS consulted for: Janssen, Medivation/Astellas, Sanofi, Ferring, Clovis Oncology and Varian. The remaining authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Spratt, D., Jackson, W., Abugharib, A. et al. Independent validation of the prognostic capacity of the ISUP prostate cancer grade grouping system for radiation treated patients with long-term follow-up. Prostate Cancer Prostatic Dis 19, 292–297 (2016). https://doi.org/10.1038/pcan.2016.18
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2016.18
This article is cited by
-
The 2014 ISUP grade group system: the Holy Grail or yet another hype?
World Journal of Urology (2021)
-
Quantification of the individual risk of each Gleason pattern, including tertiary Gleason pattern 5, after radical prostatectomy: development of the modified Gleason grade grouping (mGGG) model
BMC Cancer (2020)
-
The new ISUP 2014/WHO 2016 prostate cancer grade group system: first résumé 5 years after introduction and systemic review of the literature
World Journal of Urology (2020)
-
Treatment outcomes of prostate cancer patients with Gleason score 8–10 treated with definitive radiotherapy
Strahlentherapie und Onkologie (2019)
-
Prostate cancer grading: a decade after the 2005 modified system
Modern Pathology (2018)