Abstract
The role of thromboxane A2 (TxA2) in smoking-associated lung cancer is poorly understood. This study was conducted to study the role of TxA2 in smoking carcinogen 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK)-promoted cell survival and growth in human lung cancer cells. We found that NNK increased TxA2 synthase (TxAS) expression and thromboxane B2 (TxB2) generation in cultured lung cancer cells, the result of which was supported by the increased level of TxAS in lung cancer tissues of smokers. Both TxAS-specific inhibitor furegrelate and TxA2 receptor antagonist SQ29548 completely blocked NNK-mediated cell survival and growth via inducting apoptosis. TxA2 receptor agonist U46619 reconstituted a near-full survival and growth response to NNK when TxAS was inhibited, affirming the role of TxA2 receptor in NNK-mediated cell survival and growth. Suppression of cyclic adenosine monophosphate response element binding protein (CREB) activity by its small interference RNA blocked the effect of NNK. Phosphatidylinositol 3-kinase (PI3K)/Akt and extracellular signal-regulated kinase (ERK) also had a positive role. Altogether, our results have revealed that NNK stimulates TxA2 synthesis and activates its receptor in lung cancer cells. The increased TxA2 may then activate CREB through PI3K/Akt and extracellular ERK pathways, thereby contributing to the NNK-promoted survival and growth of lung cancer cells.
Similar content being viewed by others
Introduction
Cigarette smoking represents the leading risk factor for all lung cancer types. Generally, about 85–90% of lung cancer cases are attributable to cigarette smoking (Hecht, 2002). In addition, there is an approximate 20-fold increase in the risk of developing lung cancer for a lifetime smoker when compared with a lifetime non-smoker (Parsons et al., 2010). 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK), a nicotine-nitrosated derivative, is the major carcinogenic component in cigarette smoke. Since the polycyclic aromatic hydrocarbon of tobacco smoke was reported to cause an increase in cyclooxygenase-2 (COX-2) and its downstream product prostaglandin E2in normal and transformed oral epithelial cells in 1997 (Kelley et al., 1997), an interest in the role of COX-2 and its metabolites in tobacco carcinogen-related carcinoma has been increased.
Among the various downstream products of the COX pathway, thromboxane A2 (TxA2) participates in cancer development and metastasis (Nie et al., 2004; Sakai et al., 2006). TxA2 is converted from a COX-2 product, prostaglandin H2, by TxA2 synthase (TxAS). It exhibits diverse biological activities through its signature receptor, TxA2 receptor. TxA2 receptor can be activated by binding with its ligand TxA2, resulting in a broad range of cellular responses including signaling kinase activation, and the subsequent nuclear events involved in DNA synthesis, cell proliferation and cell survival (Huang et al., 2004). TxA2 can act on the TxA2-producing cells as a local hormone in autocrine or paracrine systems (Nie et al., 2000; Nakahata, 2008). TxA2 is extremely unstable in aqueous solution, being rapidly and non-enzymatically degraded into an inactive form of thromboxane B2 (TxB2). Therefore, TxAS and TxA2 receptor have been selected to be the indicators of TxA2 synthesis and action in ample studies. Overexpression of TxAS has been documented to have a potential role in promoting the progression of many types of cancers (Nie et al., 2004; Sakai et al., 2006; Moussa et al., 2008a; Leung et al., 2009; Cathcart et al., 2010). In addition to TxAS, the important role of TxA2 receptor in tumorigenesis and cancer progression has emerged (Sakai et al., 2006; Wei et al., 2007; Li and Tai, 2009; Cathcart et al., 2010). Particularly, we have previously demonstrated that inhibition of TxAS results in the p27-related induction of cell death or apoptosis in both human non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC) cells (Leung et al., 2009), and other authors have recently reported that the activation of TxA2 receptor induces cell proliferation in NSCLC cells (Li and Tai, 2009).
The role of TxA2 in tobacco smoke-related lung cancer remains largely unknown, although TxB2 has been shown to be significantly increased by smoking in lung tumor tissues (McLemore et al., 1988; Fahn et al., 1998; Chen et al., 2006). Herein, this study was designed to investigate the possible involvement of TxA2 in NNK-related lung tumor progression.
Results
High expression of TxAS in lung cancer tissues of smokers
Immunohistochemical staining was performed on lung cancer tissues. The scores of the immunohistochemical staining showed that TxAS expression was significantly increased in human lung cancer tumor tissues (∼90%, 30 of 37 cases) when compared with the paired corresponding non-tumor tissues (P<0.01; Table 1). The finding is in line with a previous study (Ermert et al., 2003). Strikingly, 100% samples of the smokers (tumor and non-tumor) exhibited positive staining for TxAS (Table 1). When we used the score 1 (<20%) of TxAS-positive staining as the cutoff value, smokers had higher expression of TxAS in tumor tissues (∼93%, 27 of 29 cases) when compared with non-smokers (50%, 4 of 8 cases; Table 1). The representative immunohistochemical staining (smokers and non-smokers) is shown in Figure 1a. In conjunction with our previous report showing that lung tumor tissues obtained from patients who smoked showed a higher level of TxB2 than lung tissues from patients who did not smoke (Chen et al., 2006), these results suggest that the increased TxAS may contribute to the high level of TxA2 in lung cancer tissues of smokers.
TxA2 synthesis in lung tissues and cell lines. (a) Immunohistochemical evaluation of TxAS expression in lung tissues. TxAS protein was found to be predominantly expressed in the cytoplasm of lung cells. Brown, TxAS staining; blue, nuclear staining. Original magnification × 200. The samples are representative of 37 cases. (b) NNK increased TxAS (60 kDa) expression in a dose-dependent (10 nM–20 μM, 12 h) and time-dependent (10 μM, 1–12 h) manner. Actin was used to ensure equal protein loading. The figure is the representative result selected from three independent experiments. (c) The effect of NNK on TxB2 generation in lung cancer cells. Cells were serum starved for 24 h, and then stimulated with NNK (10 μM) or furegrelate (1 mM) or both (10 μM NNK+1 mM furegrelate) for 24 h. Cells without treatment were set up as controls. The level of TxB2 in the medium was quantified using an enzyme immunoassay (EIA) kit as described under Materials and methods. Data are expressed as mean±s.d. of three independent experiments done in triplicate. **P<0.01. ctr, control; Fu, furegrelate; N, NNK. A full colour version of this figure is available at the Oncogene journal online.
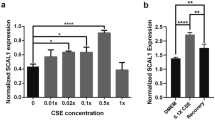
NNK stimulated TxA2 synthesis in lung cancer cells
Based on the above results obtained by immunohistochemical staining, we next sought to detect if NNK can stimulate TxA2 synthesis in lung cancer cells. Western blot analysis showed that NNK increased TxAS protein level in a time- and dose-dependent manner (Figure 1b). NNK at 100 nM clearly led to the increase of TxAS protein level and this stimulation reached to a maximum at 10 μM. NNK (10 μM) increased the level of TxAS as early as 1 h after the treatment and the increase continued up to at least 12 h. Using enzyme immunoassay kits, we next measured the effects of NNK on the level of TxB2, which is a stable and biologically inactive metabolite of TxA2. The result showed that NNK (10 μM) stimulated TxB2 production by 1.9-fold in NCI-H23 cells (P<0.01) and by 1.6-fold in CRL-2066 cells (P<0.01) when compared with control (Figure 1c). Moreover, preincubation with TxAS-specific inhibitor furegrelate significantly attenuated NNK-induced TxB2 production by nearly 75% (P<0.01) in NCI-H23 cells and 90% (P<0.01) in CRL-2066 cells. In light of the fact that the synthesis of TxA2 can be directly reflected by the TxAS expression and activity (TxB2 generation) (Nie et al., 2000, 2004; Sakai et al., 2006; Cailleteau et al., 2008), these results suggest that NNK is able to increase TxA2 output by stimulating TxAS in lung cancer cells. It should be noted that the elevated TxA2 level indicates that TxA2 receptor could be highly activated, which is generally attributed to the fact that TxA2 is a bioactive agonist that specifically interacts with its receptor on target cells to impart its biologic effects (Nie et al., 2000; Nakahata, 2008). It was reported that 7 μM of NNK corresponded to the approximate amount found in one pack of cigarettes (Proulx et al., 2005), and we have observed that the effects of NNK on lung cancer proliferation reach a plateau after its concentration reaches a level of >10 μM (Li et al., 2008, 2010). Considering these observations and the data obtained in this study, 10 μM NNK was used for conducting all further experiments.
TxAS inhibitor and TxA2 receptor antagonist prevented NNK-promoted cell proliferation/survival
Inhibition of TxA2 synthesis by TxAS inhibitors and blockade of TxA2 action by TxA2 receptor antagonists appear to be an effective method for evaluation of the role of TxA2 in tumor progression (Daniel et al., 1999; Nie et al., 2000, 2004; Nakahata, 2008). Accordingly, this pharmacological method was adopted in our study. The time course experiments of MTT (3-(4, 5-Dimethylthiazol-2-yl)-2, 5-diphenyltetrazolium bromide, a tetrazole) assay showed that the proliferation/survival of NCI-H23 cells treated with 10 μM NNK for 6, 12, 24, 48 and 72 h was 108.5±1.3, 121.4±1.7, 133.3±12.7, 143.9±8.7 and 156.1±12.6% of controls, respectively (Figure 2a). In CRL-2066 cells, it was 126.4±4.8, 141.8±2.7, 144.0±4.8, 159.4±3.3 and 171.0±2.9% of controls, respectively (Figure 2b). This finding is consistent with our previous studies (Li et al., 2008, 2010). The promoting effect of NNK on the cell proliferation/survival was fully and consistently blocked by the treatment with furegrelate (1 mM) and SQ29548 (5 μM) for 24, 48 or 72 h regardless of lung cancer cell types (Figures 2a and b). The cell proliferation/survival was below the control level at 24 h after treatment with NNK plus furegrelate or SQ29548 (Figures 2a and b). The result obtained by MTT assay was confirmed by another two methods for the cell proliferation/survival measurement: bromodeoxyuridine cell proliferation assay, which measures DNA synthesis by enzyme-linked immunosorbent assay (Figure 2c), and western blot analysis of the proliferating cell nuclear antigen (PCNA) protein (Figure 2d), which is a typical marker for cell proliferation (Stoimenov and Helleday, 2009). Collectively, pharmacological inhibition of either the synthesis of TxA2 or the activation of TxA2 receptor could totally overcome NNK-induced cell proliferation/survival, further confirming that TxA2 is critical for the proliferative effect of NNK in lung cancer cells.
Effects of blocking TxA2 synthesis or action on the proliferation/survival of NNK-treated cells. (a, b) MTT assay evaluation of cell proliferation/survival during treatment with NNK (10 μM) or co-treatment with NNK (10 μM) and furegrelate (1 mM) or SQ29548 (5 μM) for 6, 12, 24, 48 and 72 h. The results were presented as percentages of the 0 h control conditions. Data are expressed as mean±s.d. of three independent experiments done in quadruplicate. *P<0.05 and **P<0.01 compared with the control. #P<0.05 and ##P<0.01 compared with the corresponding group with NNK treatment in each time point. Bromodeoxyuridine (BrdU) cell proliferation assay (c) and western blotting evaluation of PCNA expression (d) were used to confirm the result of MTT assay. Cells were serum starved for 24 h and then treated with NNK (10 μM) or NNK (10 μM) plus furegrelate (1 mM) or SQ29548 (5 μM) for 24 h. Cells without treatment were set up as controls, and cells incubated with furegrelate (1 mM) or SQ29548 (5 μM) alone served as an additional control. (c) Cell proliferation was determined using the BrdU labeling and Detection Kit, and the results were presented as percentage of controls. Values are expressed as mean±s.d. of three independent experiments. *P<0.05 and **P<0.01. (d) The expression of PCNA (36 kDa) was evaluated by western blotting. Actin was used as an equal loading control. (e) The expression of TxA2 receptor (55 kDa) in NCI-H23 and CRL-2066 cells was examined by western blot analysis. (f) The effect of TxA2 mimetic U46619 on the proliferation of NNK-exposed cells during the inhibition of TxA2 synthesis. Cell proliferation/survival was determined by MTT assay. The results were presented as percentage of controls. Data are expressed as mean±s.d. of three independent experiments done in quadruplicate. *P<0.05 and **P<0.01. ctr, control; Fu, furegrelate; N, NNK; SQ, SQ29548; U, U46619.
TxA2 mimetic U46619 reconstituted NNK-induced cell proliferation/survival
We next sought to confirm if TxA2 receptor is concomitantly activated during the stimulation of TxA2 synthesis by NNK in lung cancer cells. Western blotting demonstrated that TxA2 receptor was readily detectable in both NCI-H23 and CRL-2066 cell lines (Figure 2e). U46619 is a stable analog of prostaglandin H2 and exhibits properties similar to TxA2 (Coleman et al., 1981). We utilized MTT assay to investigate the effect of TxA2 mimetic (TxA2 receptor agonist) U46619 on the cell proliferation/survival response to NNK when TxAS was inhibited. As shown in Figure 2f, blockade of TxA2 synthesis by furegrelate for 24 h totally overcame the NNK-induced cell proliferation, whereas the administration of TxA2 receptor agonist U46619 (1 μM) effectively reconstituted it. In addition, U46619 stimulated a similar proliferative rate of lung cancer cells as NNK. These results provided strong evidence that activation of TxA2 receptor is necessary for NNK-mediated lung cancer cell proliferation/survival.
Blockade of TxA2 synthesis or action induced the apoptosis of NNK-exposed cells
As MTT assay is a quantitative colorimetric assay for mammalian cell proliferation/survival (Mosmann, 1983), the data obtained by MTT assay implied that NNK may have pro-survival effect to promote tumor cell proliferation. The subsequent experiments were undertaken to examine if the blockage of TxA2 would affect apoptosis in NNK-exposed cells. TdT-mediated dUTP nick end labeling (TUNEL) method using flow cytometry for apoptosis analysis was performed. As illustrated in Figure 3a, co-treatment with NNK and furegrelate or SQ29548 resulted in a significant increase (4.9- or 3.7-fold) in the fraction of apoptotic cells in NCI-H23 (P=0.042 and P=0.031, respectively) when compared with the control. The percentage of TUNEL-positive cells were also significantly higher in CRL-2066 cells treated with furegrelate or SQ29548 in the presence of NNK than the control (5.5-fold, P=0.009 or 4.6-fold, P=0.044; Figure 3a). The trends of apoptosis induced by furegrelate or SQ29548 (in the presence of NNK) in both cell lines were similar. Moreover, protein levels of B-cell lymphoma 2 (Bcl-2), Bax and poly (ADP-ribose) polymerase (PARP) were measured (Figure 3b). An increase in antiapoptotic protein Bcl-2 accompanied by the slight decrease in apoptotic protein Bax was observed after 24 h of treatment with NNK. Both furegrelate and SQ29548 reversed the NNK-induced high ratio of Bcl-2/Bax by decreasing Bcl-2 expression and increasing Bax expression. Furthermore, the increase in cleaved PARP accompanied by the decrease in full-length PARP was detected in groups of NNK in combination with furegrelate or SQ29548. Collectively, these results suggested that blockade of TxA2 synthesis or its receptor prevented NNK-induced cell proliferation through induction of apoptosis.
Effects of blocking TxA2 synthesis or action on the survival of NNK-treated cells. Cells were serum starved for 24 h and then treated with NNK (10 μM) or NNK (10 μM) plus furegrelate (1 mM) or SQ29548 (5 μM) for another 24 h. Cells without treatment were set up as controls, and cells incubated with furegrelate (1 mM) or SQ29548 (5 μM) alone served as additional controls. (a) TUNEL apoptosis analysis. The number of TUNEL-positive cells was counted by flow cytometry. Data are expressed as mean±s.d. of three independent experiments. *P<0.05 and **P<0.01. (b) Western blotting evaluation of Bcl-2 (28 kDa), Bax (20 kDa) and PARP (full length: 116 kDa; cleavage: 89 kDa) protein expression. Actin was used as an equal loading control. The figure is the representative result selected from three independent experiments. ctr, control; Fu, furegrelate; N, NNK; SQ, SQ29548; U, U46619.
CREB is accountable for the key role of TxA2 in NNK-mediated cell proliferation/survival
CREB, a transcriptional factor, is thought to have a central role in tumor pathogenesis by continually driving the expression of concerned genes through the interaction with a DNA sequence called cyclic adenosine monophosphate response element (CRE: 5′-TGACGTCA-3′) (Sakamoto and Frank, 2009). To stimulate CRE-dependent transcription, CREB must be activated through phosphorylation at serine 133 (Sakamoto and Frank, 2009). In addition, CREB has been identified as a crucial survival factor in lung cancer with convincing evidence, showing the direct key role of phosphorylated CREB in promoting lung cancer cell proliferation (Laag et al., 2006; Aggarwal et al., 2008; Li and Tai, 2009). On the basis of these observations, we sought to determine if the involvement of TxA2 in NNK-induced proliferation is through the activation of CREB. As shown in Figure 4a, even though NNK did not affect CREB expression, it enhanced the phosphorylated CREB. Furegrelate or SQ29548 pre-treatment significantly blocked the NNK-induced increase of phosphorylated CREB. Subsequently, we suppressed the CREB activity in both cell lines by knockdown of CREB expression with small interference RNA (siRNA). Western blot analysis indicated that the expression and phosphorylation of CREB were significantly suppressed by transfection of CREB siRNA in both cell lines (Figure 4b). It is well known that both PCNA and Bcl-2 are CRE-containing genes (Ciani et al., 2002; Sakamoto and Frank, 2009). Western blot analysis also demonstrated that CREB siRNA notably attenuated the augmented PCNA and Bcl-2 expression induced by NNK (Figure 4c), the result of which is similar to that noted with furegrelate or SQ29548 pretreatment (Figures 2d and 3b). The results observed in U46619-exposed cells were similar to the effects seen in the cells exposed to NNK. Furthermore, MTT assay showed that the similar proliferative/survival rates of lung cancer cells by NNK and U46619 were substantially blocked by CREB siRNA (Figure 4d). These results suggest that CREB may function as a key effector of TxA2 in NNK-exposed cells.
The involvement of CREB in NNK-mediated regulation of TxA2 and cell proliferation/survival. (a) The effect of furegrelate or SQ2948 on NNK-induced CREB phosphorylation. The cells were serum starved for 24 h and then treated with NNK (10 μM) alone for 30 min. The cells were incubated with furegrelate (1 mM) or SQ29548 (5 μM) for 20 min before stimulation with NNK (10 μM) for 30 min. The cells without treatment served as controls, and the cells exposed to furegrelate (1 mM) or SQ29548 (5 μM) alone for entire duration of treatment were set up as additional controls. The phosphorylated CREB (pCREB, 43 kDa) and total CREB (43 kDa) levels were determined by western blot analysis. The figure is a representative result selected from three independent experiments. (b) CREB expression and phosphorylation were suppressed by CREB siRNA. Cells were transiently transfected with either non-target siRNA (control siRNA) or CREB siRNA for 24 h. Total protein was extracted and subjected to western blot analysis for detection of pCREB and CREB level. Actin was used as an equal loading control. The figure is the representative result selected from three independent experiments. (c, d) Cells were transiently transfected with either non-target siRNA or CREB siRNA for 24 h, in the absence or presence of NNK (10 μM) or U46619 (1 μM). The cells transfected with non-target siRNA without chemical treatment were set up as the control for all other groups. (c) The expression of PCNA (36 kDa) and Bcl-2 (28 kDa) was measured by western blot analysis. Actin was used as an equal loading control. The figure is the representative result selected from three independent experiments. (d) Cell proliferation/survival was assessed by MTT assay, and the results were presented as percentage of controls. Data are expressed as mean±s.d. of three independent experiments done in quadruplicate. *P<0.05, **P<0.01. ctr, control; Fu, furegrelate; N, NNK; NT siRNA, non-target siRNA; SQ, SQ29548; U, U46619.
PI3K/Akt and ERK rather than JNK and p38 pathways were mediated by TxA2 in the NNK-exposed cells
In order to further gain some insight into the signaling mechanism whereby TxA2 is involved in NNK-induced cell proliferation/survival, we employed western blot analysis to analyze Akt and extracellular signal-regulated kinase (ERK) in the cell survival pathway. We used the phosphatidylinositol 3-kinase (PI3K)-specific inhibitor wortmannin to block Akt pathway, as the specific inhibitors of Akt are not available yet and Akt is a pivotal downstream component of PI3K pathway (Sebolt-Leopold and Herrera, 2004). As indicated in Figure 5, either furegrelate or SQ29548 partially but markedly reduced the phosphorylation of Akt induced by NNK whereas wortmannin abrogated it. We observed similar changes in phosphorylated ERK (Figure 5). In these cells, additional control experiments were performed with TxA2 mimetic U46619, which yielded an almost identical stimulation of phosphorylated Akt and phosphorylated ERK as NNK.
Effects of blocking TxA2 synthesis and action on Akt, ERK, JNK and p38 in cells exposed to NNK. The cells were serum starved for 24 h and then treated with NNK (10 μM) alone or NNK (10 μM) plus U46619 (1 μM) for 30 min. The cells were treated with furegrelate (1 mM), SQ29548 (5 μM) or various kinase inhibitors for 20 min before stimulation with NNK for another 30 min. The cells without treatment served as controls, and the cells treated with furegrelate (1 mM), SQ29548 (5 μM) or each of the inhibitors alone for entire duration of treatment were set up as additional controls. The cells exposed to U46619 (1 μM) alone for 30 min were also set up as additional controls. The levels of phosphorylated Akt (pAkt, 60 kDa), total Akt (60 kDa), phosphorylated ERK (pERK, 42/44 kDa), total ERK (42/44 kDa), phosphorylated JNK (pJNK, 46/54 kDa), total JNK (46/54 kDa), phosphorylated p38 (pp38, 40 kDa) or total p38 (40 kDa) were detected by western blot analysis. The figure is the representative result selected from three independent experiments. Fu, furegrelate; N, NNK; SQ, SQ29548, U, U46619. KI is each of the kinase inhibitors (ERK, 5 μM CAY10561; JNK, 30 μM SP600125; p38, 10 μM SB203580; PI3K/Akt, 200 nM wortmannin).
It is well known that mitogen-activated protein kinase (MAPK) signaling pathways, which mainly include ERK, p38 and c-Jun NH(2)-terminal kinase (JNK) three members, are crucial for cell proliferation/survival in cancer (Li et al., 2007; Wei et al., 2007). Therefore, we also examined whether TxA2 affected their activation in the cells treated with NNK. As shown in Figure 5, phosphorylated JNK was mildly increased by NNK, but it was not obviously affected by furegrelate, SQ29548 and U46619. In contrast, phosphorylated p38 expression could be slightly reduced by furegrelate and SQ29548 and only increased by U46619 (Figure 5). The results obtained in both cell lines were similar, and the expression of total Akt, ERK, JNK or p38 protein was not changed by the above treatments.
CREB is located downstream of the PI3K/Akt and ERK pathways in NNK-treated cells
The final series of experiments employed kinase inhibitors to investigate the action of PI3K/Akt and ERK pathways on CREB phosphorylation in NNK-exposed cells. As shown in Figure 6, CAY10561 effectively attenuated NNK-induced CREB activation (phosphorylated CREB) in both cell lines, whereas wortmannin moderately prevented it. The attenuation of CREB activation by wortmannin was greater in CRL-2066 cells than in NCI-H23 cells. The results observed in U46619-exposed cells were similar to the effects seen in the cells exposed to NNK. No alteration was detectable regarding the expression of total CREB in both cell lines tested.
The action of PI3K/Akt or ERK pathways on CREB activation in NNK-exposed cells. The cells were serum starved for 24 h and then treated with NNK (10 μM) alone for 30 min. The cells were incubated with wortmannin (200 nM) or CAY10561 (5 μM) for 20 min before stimulation with NNK (10 μM) or U46619 (1 μM) for 30 min. The cells without treatment served as controls, and the cells exposed to each of the inhibitors alone for entire duration of treatment were set up as additional controls. The phosphorylated CREB (pCREB, 43 kDa) and total CREB (43 kDa) levels were determined by western blot analysis. The figure is a representative result selected from three independent experiments. CAY, CAY10561; N, NNK; U, U46619; Wort, wortmannin.
Discussion
There are an increasing number of publications describing the potential role of TxA2 and its related molecules in promoting progression of lung cancer (Ermert et al., 2003; Wei et al., 2007; Leung et al., 2009; Li and Tai, 2009). Unfortunately, the possible role of TxA2 in smoking-associated lung cancer has received limited attention. In this study, we have demonstrated that NNK could stimulate the synthesis and action of TxA2 in lung cancer cells. Such a response was directly correlated with the activation of PI3K/Akt and ERK pathways, leading to the activation of CREB.
We have shown that the synthesis of TxA2, reflected by TxAS expression and its activity (TxB2 formation), is elevated in lung cancer tissues of smokers and in lung cancer cells exposed to tobacco smoking carcinogen NNK. This finding is supported by other reports (McLemore et al., 1988; Fahn et al., 1998). NNK is the principal tobacco smoke carcinogen, and it can increase the expression and activity of COX-2, an upstream enzyme of TxA2, in lung cancer (El-Bayoumy et al., 1999; Grozio et al., 2007). The synthesis of TxA2 by TxAS is dependent on COX activities as COX-1 and COX-2 provide TxAS with the substrate, prostaglandin H2 (Nie et al., 2004). In addition, it has been recently demonstrated that nicotine plus its five major metabolites were significantly elevated in smokers when compared with non-smokers, with a significant high level of TxB2 (Calapai et al., 2009). Thus, it is reasonable to postulate that NNK stimulates TxA2 synthesis in lung cancer cells. This hypothesis was verified by the data that NNK increased TxAS expression and TxB2 generation in lung cancer cells. Blockade of TxA2 synthesis by TxAS-specific inhibitor furegrelate not only completely prevented NNK-induced high TxB2 level but also significantly inhibited NNK-promoted cell proliferation/survival, and TxA2 mimetic (TxA2 receptor agonist) U46619 induced a similar proliferative/survival rate as NNK. These results suggest that TxA2 has a functional role in mediating NNK-induced lung cancer cell proliferation/survival. Moreover, when TxAS was inhibited, U46619 could reconstitute a near-full proliferative/survival response to NNK, indicating that TxA2 receptor is necessary for the action of TxA2 in NNK-exposed lung cancer cells. Furthermore, TxA2 receptor antagonist SQ29548 that blocks TxA2 binding to its receptor as well as TxAS-specific inhibitor furegrelate significantly inhibited the pro-proliferative/survival effect of NNK and blocked NNK-induced PCNA and Bcl-2 elevation. These findings support that both activation of TxA2 receptor and synthesis of TxA2 have a critical role in NNK-promoted cell proliferation/survival. Our findings can be substantiated by several lines of evidence. For example, it has recently been demonstrated that the activation of TxA2 receptor by I-BOP (another TxA2 mimetic) promoted cell proliferation in lung A549 (NSCLC) cells (Li and Tai, 2009). In addition, the bladder cancer cells transfected with β-isoform of TxA2 receptor and stimulated with U46619 resulted in a significant increase in cellular growth rate and PCNA expression (Moussa et al., 2008b). A recent study has also reported that treatment of two NSCLC cell lines with another selective TxAS inhibitor ozagrel induced a significant reduction in cell proliferation (Cathcart et al., 2010). We have further demonstrated that the inhibitory effect of furegrelate or SQ29548 on NNK-promoted cell proliferation/survival is in part due to an increase in apoptosis regardless of cell type, which is supported by the previous reports showing that inhibition of TxAS resulted in apoptosis in bladder (Moussa et al., 2008a) and lung (Cathcart et al., 2010) cancer cells, and that treatment with TxA2 receptor antagonists also caused significant apoptosis in bladder cancer cells (Moussa et al., 2008b).
By modulating gene expression that are critically important in the tumor pathogenesis, transcription factors are believed to be the final regulators of the central processes of tumor progression such as proliferation and survival (Sakamoto and Frank, 2009). CREB is one such transcription factor (Sakamoto and Frank, 2009), and it is constitutively activated in both NSCLC and SCLC cells (Ma et al., 2007; Aggarwal et al., 2008). Additionally, CREB has been shown to be activated by NNK, TxA2 or TxA2 mimetic in lung cancer cells (Laag et al., 2006; Wei et al., 2007; Li and Tai, 2009). Therefore, CREB activation and its related proteins, PCNA and Bcl-2, were evaluated in this study. We demonstrated that either furegrelate or SQ29548 dramatically blocked NNK-induced CREB activation, which is consistent with the finding that either furegrelate or SQ29548 significantly inhibited the NNK-promoted cell proliferation/survival. Moreover, CREB siRNA prevented the NNK or U46619-induced PCNA and Bcl-2 elevation and abolished the enhanced cell proliferation/survival induced by NNK or U46619 in both types of lung cancer cells tested. In support of these results, it has been reported that the upregulation of PCNA and Bcl-2 could occur through the increase in their transcription factor CREB phosphorylation (Ciani et al., 2002), and that inhibition of CREB activity effectively suppressed the proliferation and survival of NSCLC cells (Aggarwal et al., 2008). These data are in line with our results showing that TxA2 is involved in NNK-promoted cell proliferation/survival by activating CREB. The conclusion supports the fact that CREB is an effector for a variety of receptors, including receptors for growth factors, hormones and prostaglandins (Aggarwal et al., 2008).
We have further examined the signaling mechanism whereby TxA2 is involved in NNK-promoted cell proliferation/survival. The PI3K/Akt and MAPK pathways are known to be the crucial pro-survival signaling and have critically important roles in cellular proliferation and growth (Merighi et al., 2006). It is noted that the PI3K/Akt and ERK pathways are two principal signalings associated with NNK (West et al., 2003; Hung and Hung, 2009). These two pathways can also be activated by TxA2 mimetic in cancer cells (Li et al., 2007; Wei et al., 2007). Although there are common signaling targets, no study has been previously done to correlate NNK with TxA2. In this study, we demonstrated that short-term NNK exposure led to high levels of phosphorylated Akt or ERK in lung cancer cells, which is in good agreement with a recent study (Nishioka et al., 2010). We further showed that TxA2 mimetic U46619 could yield similar stimulation of phosphorylated Akt or ERK as NNK, confirming the role of TxA2 in the upregulation of phosphorylated Akt or ERK. Importantly, either furegrelate or SQ29548 could inhibit the NNK-mediated activation of Akt and ERK, indicating that the effect of NNK depends on TxAS and TxA2 receptor. However, we could not find a strict correlation between NNK and TxA2 in the activation of both p38 MAPK and JNK pathways. As a matter of fact, the phosphorylation of these two kinases in response to TxA2 may be somewhat controversial. A linkage between the level of phosphorylated JNK and the sensitivity to TxA2 has been previously reported in cells of other tumor types (Miggin and Kinsella, 2001; Li et al., 2007), whereas studies in lung cancer cells have found no correlation (Wei et al., 2007). The data on the response of p38 phosphorylation to NNK in cancer studies are limited, whereas it has been well established that NNK can stimulate JNK activation in lung cancer of animal models (Kim et al., 2006; Lu et al., 2006). In this study, the phosphorylated p38 was shown to be influenced only by TxA2, whereas activation of JNK was demonstrated to be stimulated merely by NNK. The result indicated that the contribution of TxA2 to NNK-promoted cell proliferation/survival is likely because of the activation of ERK rather than p38 and JNK in MAPK family, and that NNK may have some effects that are independent of TxA2. We were unable to correlate the role of TxA2 with JNK phosphorylation, suggesting that the effect of NNK is independent of JNK activation.
CREB is known to be activated through phosphorylation by several kinases, including PI3K/Akt and ERK (Sakamoto and Frank, 2009). ERK has been well established to be a key upstream of CREB in NSCLC cells (Wei et al., 2007; Aggarwal et al., 2008; Li and Tai, 2009), whereas there is little information on the action of PI3K/Akt on CREB activity in lung cancer cells. Our study has confirmed that ERK is significantly involved in CREB phosphorylation in lung cancer cells. However, the activation of PI3K/Akt by NNK contributed to CREB phosphorylation to a lesser degree, as the PI3K/Akt pathway inhibitor wortmannin blocks either NNK- or U46619-induced CREB activation moderately. Moreover, the inhibition of CREB activation by wortmannin was greater in CRL-2066 (SCLC) cells than in NCI-H23 (NSCLC) cells stimulated with either NNK or U46619. Such diverse outcomes suggest that CREB activation may be one, but not the only, mechanism responsible for the involvement of TxA2 in NNK-induced lung cancer cell proliferation.
It is well known that besides NNK, cigarette smoking can also generate other chemical carcinogens such as NNAL (4-(methylnitrosamino)-1-(3-pyridyl)-1-butanol), NNN (N-nirosonornicotine) and NAB (N′-nitrosoanabasine) (Hoffmann et al., 1994). Based on the experiment of lung tumorigenesis in animal models, the ranking of potency of these carcinogens are as follows: NNK>NNAL>NNN>NAB (Amin et al., 1996). This study is thus focused on the most potent cigarette-smoking carcinogen, NNK. Whether other tobacco smoking-generated lung carcinogens can act in similar or same way as NNK to influence the TxA2 requires further investigation.
In summary, this study has delineated the involvement of TxA2 in NNK-promoted lung cancer cell proliferation/survival and its signaling mechanism (Figure 7), which advances our current knowledge of how NNK contributes to tumor growth of lung cancer. NNK may activate TxA2 receptor via stimulation of TxA2 synthesis. TxA2 activates the transcription factor CREB whose target genes include PCNA and Bcl-2, thereby contributing to NNK-induced lung cancer cell proliferation/survival. The PI3K/Akt and ERK pathways are involved in NNK-mediated tumor growth. ERK pathway is essential for the NNK-induced activation of CREB. To a lesser degree, PI3K/Akt pathway may also have a positive role. Thus, our study has highlighted the significance of TxA2-related pathway with respect to smoking-associated lung cancer progression. The findings may help to develop drugs affecting TxA2 synthesis or action to treat this deadly disease.
Materials and methods
Human lung tissue and immunohistochemical analysis
A total of 37 pairs of tumor and non-tumor lung tissues were obtained from lung cancer patients who underwent surgical resection at the Prince of Wales Hospital. Tumor tissue samples were taken from the central part of the tumors. Of the 37 patients, 29 were cigarette smokers with an average smoking history of >28 years and the other 8 patients were non-smokers. The samples included 11 pairs of squamous cell carcinoma tissues, 11 pairs of adenocarcinoma tissues, 5 pairs of large cell carcinoma tissues and 10 pairs of poorly differentiated carcinoma tissues. All types of tissue specimens were confirmed by histological examination. The tissue samples were stored in a liquid nitrogen tank until the experiments were performed. The tissues were sectioned and immunohistochemical staining was carried out using rabbit anti-TxAS antibody (Cayman Chemical, Ann Arbor, MI, USA).
Cell lines and cell culture
Two cell lines were selected in this study. NCI-H23 and CRL-2066 were obtained from American Type Culture Collection (Rockville, MD, USA). The former is a NSCLC cell line whereas the latter is a SCLC cell line. These two cell lines were grown in Dulbecco's modified Eagle's medium and Waymouth's MB 752/1 medium (Gibco, Grand Island, NY, USA), respectively.
Chemicals and drug treatment
Furegrelate (TxAS-specific inhibitor), SQ29548 (TxA2 receptor antagonist, also known as TxA2 functional antagonist; Nie et al., 2004), U46619 (TxA2 receptor agonist, also known as TxA2 mimetic; Li et al., 2007), CAY10561 (ERK-specific inhibitor; Aronov et al., 2007) and SP600125 (the JNK inhibitor) were purchased from Cayman Chemical. NNK and SB203580 (p38 MAPK-specific inhibitor) were obtained from Toronto Research Chemicals Inc. (Toronto, North York, Canada). The PI3K-specific inhibitor, wortmannin, was purchased from Sigma Chemical Co. (St Louis, MO, USA). The concentrations of all chemicals used were based on the product datasheets and previous publications (Daniel et al., 1999; de Leval et al., 2006; Aronov et al., 2007; Li et al., 2007; Wei et al., 2007; Cailleteau et al., 2008; Moussa et al., 2008a, 2008b), and they were proven to be optimal in the present study. Dimethylsulfoxide, an organic solvent, was used in the treatment with different drugs. In all experiments, the final concentration of dimethylsulfoxide did not exceed 0.005%, which did not induce differentiation or cell death in our model studied.
TxB2 enzyme immunoassay assay
TxB2 was detected by peroxidase-labeled TxB2 conjugates using an enzyme immunoassay kit according to a previous description (Chen et al., 2006).
MTT assay
Tumor cell proliferation and survival was determined by MTT assay, which was performed as previously described (Chen et al., 2006; Li et al., 2008, 2010).
Bromodeoxyuridine cell proliferation assay
Proliferation/survival of lung cancer cells was further studied using a bromodeoxyuridine labeling enzyme-linked immunosorbent assay kit (Roche Applied Science, Penzberg, Germany), which was performed as previously described (Chen et al., 2006; Li et al., 2008, 2010).
TUNEL
Apoptotic cells were measured by an APO-BRDU TUNEL kit (Phoenix Flow Systems, San Diego, CA, USA), which was performed as previously described (Chen et al., 2006; Li et al., 2008, 2010).
Transfection of cells with CREB siRNA
Lung cancer cells were seeded at the same density into a six-well culture plate, and then incubated overnight to allow cells to attach to the plate. CREB siRNA and non-target siRNA (control siRNA) were transfected into the cells with the aid of Lipofectamine 2000 reagents (Invitrogen, Carlsbad, CA, USA), according to the manufacturer's instruction (Santa Cruz Biotechnology, Santa Cruz, CA, USA). After 5-h transfection, the cells were recovered with the fresh culture medium. After 24-h recovery, the cells were exposed to the low-serum media (2% fetal bovine serum) with or without NNK or U46619 for MTT assay or other experiments.
Western blot analysis
Western blot was performed as previously described (Li et al., 2008, 2010). The following antibodies were used for western blotting: mouse monoclonal antibody against total p38 MAPK (1:200), rabbit polyclonal antibodies against TxAS (1:200), TxA2 receptor (1:200), phosphorylated p38 MAPK (1:1000) and phosphorylated ERK (1:1000) (Cayman Chemical), mouse monoclonal antibody against PCNA (1:5000), goat polyclonal antibody against β-actin (1:1000). The following antibodies were used for the western blotting. Mouse monoclonal antibody against total p38 MAPK (1:200), rabbit polyclonal antibodies against TxAS (1:200), TxA2 receptor (1:200), phosphorylated p38 MAPK (1:1000) and phosphorylated ERK (1:1000) were all purchased from Cayman chemical. Mouse monoclonal antibody against PCNA (1:5000), goat polyclonal antibody against β-actin (1:1000), rabbit polyclonal antibodies against phosphorylated Akt (Thr308) (1:1000), total Akt (1:1000), PARP (1:1000), Bax (1:1000) and Bcl-2 (1:1000) were from Santa Cruz Biotechnology (Santa Cruz, CA, USA). Rabbit monoclonal antibody against phosphorylated CREB (ser133) and total-CREB (1:1000), mouse monoclonal antibodies against total ERK (1:1000), phosphorylated JNK (1:1000) and total JNK (1:1000) were from Cell Signaling Technology (Beverly, MA, USA). Representative results reported were from three independent experiments.
Statistical analysis
SPSS 16.0 for windows software was used for statistical data analysis (SPSS, Chicago, IL, USA). The Wilcoxon signed-ranks test was used when appropriate to compare the difference in TxAS expression between tumor and non-tumor lung tissues. The Fisher's exact test was used to compare the difference in TxAS expression in tumor tissues between smokers and non-smokers. One-way ANOVA followed by Dunnett's test was used for comparing multiple groups against a single control, whereas Student's t-test was employed for comparison between two groups. The acceptable level of significance was P<0.05 or 0.01. All data are shown as mean±s.d. of at least three independent experiments.
References
Aggarwal S, Kim SW, Ryu SH, Chung WC, Koo JS . (2008). Growth suppression of lung cancer cells by targeting cyclic AMP response element-binding protein. Cancer Res 68: 981–988.
Amin S, Desai D, Hecht SS, Hoffmann D . (1996). Synthesis of tobacco-specific N-nitrosamines and their metabolites and results of related bioassays. Crit Rev Toxicol 26: 139–147.
Aronov AM, Baker C, Bemis GW, Cao J, Chen G, Ford PJ et al. (2007). Flipped out: structure-guided design of selective pyrazolylpyrrole ERK inhibitors. J Med Chem 50: 1280–1287.
Cailleteau C, Liagre B, Battu S, Jayat-Vignoles C, Beneytout JL . (2008). Increased cyclooxygenase-2 and thromboxane synthase expression is implicated in diosgenin-induced megakaryocytic differentiation in human erythroleukemia cells. Anal Biochem 380: 26–34.
Calapai G, Caputi AP, Mannucci C, Gregg EO, Pieratti A, Aurora Russo G et al. (2009). A cross-sectional investigation of biomarkers of risk after a decade of smoking. Inhal Toxicol 21: 1138–1143.
Cathcart MC, Reynolds JV, O′Byrne KJ, Pidgeon GP . (2010). The role of prostacyclin synthase and thromboxane synthase signaling in the development and progression of cancer. Biochim Biophys Acta 1805: 153–166.
Chen GG, Lee TW, Yip JH, Xu H, Lee IK, Mok TS et al. (2006). Increased thromboxane B(2) levels are associated with lipid peroxidation and Bcl-2 expression in human lung carcinoma. Cancer Lett 234: 193–198.
Ciani E, Guidi S, Bartesaghi R, Contestabile A . (2002). Nitric oxide regulates cGMP-dependent cAMP-responsive element binding protein phosphorylation and Bcl-2 expression in cerebellar neurons: implication for a survival role of nitric oxide. J Neurochem 82: 1282–1289.
Coleman RA, Humphrey PP, Kennedy I, Levy GP, Lumley P . (1981). Comparison of the actions of U-46619, a prostaglandin H2-analogue, with those of prostaglandin H2 and thromboxane A2 on some isolated smooth muscle preparations. Br J Pharmacol 73: 773–778.
Daniel TO, Liu H, Morrow JD, Crews BC, Marnett LJ . (1999). Thromboxane A2 is a mediator of cyclooxygenase-2-dependent endothelial migration and angiogenesis. Cancer Res 59: 4574–4577.
de Leval X, Dassesse T, Dogné JM, Waltregny D, Bellahcène A, Benoit V et al. (2006). Evaluation of original dual thromboxane A2 modulators as antiangiogenic agents. J Pharmacol Exp Ther 318: 1057–1067.
El-Bayoumy K, Iatropoulos M, Amin S, Hoffmann D, Wynder EL . (1999). Increased expression of cyclooxygenase-2 in rat lung tumors induced by the tobacco-specific nitrosamine 4-(methylnitrosamino)-4-(3-pyridyl)-1-butanone: the impact of a high-fat diet. Cancer Res 59: 1400–1403.
Ermert L, Dierkes C, Ermert M . (2003). Immunohistochemical expression of cyclooxygenase isoenzymes and downstream enzymes in human lung tumors. Clin Cancer Res 9: 1577–1578.
Fahn HJ, Wang LS, Kao SH, Chang SC, Huang MH, Wei YH . (1998). Smoking-associated mitochondrial DNA mutations and lipid peroxidation in human lung tissues. Am J Respir Cell Mol Biol 19: 901–909.
Grozio A, Catassi A, Cavalieri Z, Paleari L, Cesario A, Russo P . (2007). Nicotine, lung and cancer. Anticancer Agents Med Chem 7: 461–466.
Hecht SS . (2002). Cigarette smoking and lung cancer: chemical mechanisms and approaches to prevention. Lancet Oncol 3: 461–469.
Hoffmann D, Brunnemann KD, Prokopczyk B, Djordjevic MV . (1994). Tobacco-specific N-nitrosamines and Areca-derived N-nitrosamines: chemistry, biochemistry, carcinogenicity, and relevance to humans. J Toxicol Environ Health 41: 1–52.
Huang JS, Ramamurthy SK, Lin X, Le Breton GC . (2004). Cell signalling through thromboxane A2 receptors. Cell Signal 16: 521–533.
Hung YH, Hung WC . (2009). 4-(Methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK) enhances invasiveness of lung cancer cells by up-regulating contactin-1 via the alpha7 nicotinic acetylcholine receptor/ERK signaling pathway. Chem Biol Interact 179: 154–159.
Kelley DJ, Mestre JR, Subbaramaiah K, Sacks PG, Schantz SP, Tanabe T et al. (1997). Benzo[a]pyrene up-regulates cyclooxygenase-2 gene expression in oral epithelial cells. Carcinogenesis 18: 795–799.
Kim Y, Chongviriyaphan N, Liu C, Russell RM, Wang XD . (2006). Combined antioxidant (beta-carotene, alpha-tocopherol and ascorbic acid) supplementation increases the levels of lung retinoic acid and inhibits the activation of mitogen-activated protein kinase in the ferret lung cancer model. Carcinogenesis 27: 1410–1419.
Laag E, Majidi M, Cekanova M, Masi T, Takahashi T, Schuller HM . (2006). NNK activates ERK1/2 and CREB/ATF-1 via β-1-AR and EGFR signaling in human lung adenocarcinoma and small airway epithelial cells. Int J Cancer 119: 1547–1552.
Leung KC, Hsin MK, Chan JS, Yip JH, Li M, Leung BC et al. (2009). Inhibition of thromboxane synthase induces lung cancer cell death via increasing the nuclear p27. Exp Cell Res 315: 2974–2981.
Li MY, Hsin MK, Yip J, Mok TS, Underwood MJ, Chen GG . (2010). PPAR{gamma} activation extinguishes smoking carcinogen by inhibiting NNK-mediated proliferation. Am J Respir Cell Mol Biol 42: 113–122.
Li MY, Yip J, Hsin MK, Mok TS, Wu Y, Underwood MJ et al. (2008). Haem oxygenase-1 plays a central role in NNK-mediated lung carcinogenesis. Eur Respir J 32: 911–923.
Li X, Tai HH . (2009). Activation of thromboxane A (2) receptors induces orphan nuclear receptor Nurr1 expression and stimulates cell proliferation in human lung cancer cells. Carcinogenesis 30: 1606–1613.
Li X, Wei J, Tai HH . (2007). Activation of extracellular signal-regulated kinase by 12-hydroxy- heptadecatrienoic acid in prostate cancer PC3 cells. Arch Biochem Biophys 467: 20–30.
Lu G, Liao J, Yang G, Reuhl KR, Hao X, Yang CS . (2006). Inhibition of adenoma progression to adenocarcinoma in a 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone-induced lung tumorigenesis model in A/J mice by tea polyphenols and caffeine. Cancer Res 66: 11494–11501.
Ma PC, Tretiakova MS, Nallasura V, Jagadeeswaran R, Husain AN, Salgia R . (2007). Downstream signalling and specific inhibition of c-MET/HGF pathway in small cell lung cancer: implications for tumour invasion. Br J Cancer 97: 368–377.
McLemore TL, Hubbard WC, Litterst CL, Liu MC, Miller S, McMahon NA et al. (1988). Profiles of prostaglandin biosynthesis in normal lung and tumor tissue from lung cancer patients. Cancer Res 48: 3140–3147.
Merighi S, Benini A, Mirandola P, Gessi S, Varani K, Leung E et al. (2006). Modulation of the Akt/Ras/Raf/MEK/ERK pathway by A(3) adenosine receptor. Purinergic Signal 2: 627–632.
Miggin SM, Kinsella BT . (2001). Thromboxane A (2) receptor mediated activation of the mitogen activated protein kinase cascades in human uterine smooth muscle cells. Biochim Biophys Acta 1539: 147–162.
Mosmann T . (1983). Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J Immunol Methods 65: 55–63.
Moussa O, Ashton AW, Fraig M, Garrett-Mayer E, Ghoneim MA, Halushka PV et al. (2008b). Novel role of thromboxane receptors beta isoform in bladder cancer pathogenesis. Cancer Res 68: 4097–4104.
Moussa O, Riker JM, Klein J, Fraig M, Halushka PV, Watson DK . (2008a). Inhibition of thromboxane synthase activity modulates bladder cancer cell responses to chemotherapeutic agents. Oncogene 27: 55–62.
Nakahata N . (2008). Thromboxane A2: physiology/pathophysiology, cellular signal transduction and pharmacology. Pharmacol Ther 118: 18–35.
Nie D, Che M, Zacharek A, Qiao Y, Li L, Li X et al. (2004). Differential expression of thromboxane synthase in prostate carcinoma: role in tumor cell motility. Am J Pathol 164: 429–439.
Nie D, Lamberti M, Zacharek A, Li L, Szekeres K, Tang K et al. (2000). Thromboxane A(2) regulation of endothelial cell migration, angiogenesis, and tumor metastasis. Biochem Biophys Res Commun 267: 245–251.
Nishioka T, Guo J, Yamamoto D, Chen L, Huppi P, Chen CY . (2010). Nicotine, through upregulating pro-survival signaling, cooperates with NNK to promote transformation. J Cell Biochem 109: 152–161.
Parsons A, Daley A, Begh R, Aveyard P . (2010). Influence of smoking cessation after diagnosis of early stage lung cancer on prognosis: systematic review of observational studies with meta-analysis. Br Med J 340: b5569.
Proulx LI, Gaudreault M, Turmel V, Augusto LA, Castonguay A, Bissonnette EY . (2005). 4-(Methylnitrosamino)-1-(3-pyridyl)-1-butanone, a component of tobacco smoke, modulates mediator release from human bronchial and alveolar epithelial cells. Clin Exp Immunol 140: 46–53.
Sakai H, Suzuki T, Takahashi Y, Ukai M, Tauchi K, Fujii T et al. (2006). Upregulation of thromboxane synthase in human colorectal carcinoma and the cancer cell proliferation by thromboxane A2. FEBS Lett 580: 3368–3374.
Sakamoto KM, Frank DA . (2009). CREB in the pathophysiology of cancer: implications for targeting transcription factors for cancer therapy. Clin Cancer Res 15: 2583–2587.
Sebolt-Leopold JS, Herrera R . (2004). Targeting the mitogen-activated protein kinase cascade to treat cancer. Nat Rev Cancer 4: 937–947.
Stoimenov I, Helleday T . (2009). PCNA on the crossroad of cancer. Biochem Soc Trans 37: 605–613.
Wei J, Yan W, Li X, Chang WC, Tai HH . (2007). Activation of thromboxane receptor alpha induces expression of cyclooxygenase-2 through multiple signaling pathways in A549 human lung adenocarcinoma cells. Biochem Pharmacol 74: 787–800.
West KA, Brognard J, Clark AS, Linnoila IR, Yang X, Swain SM et al. (2003). Rapid Akt activation by nicotine and a tobacco carcinogen modulates the phenotype of normal human airway epithelial cells. J Clin Invest 111: 81–90.
Acknowledgements
We thank Suk Ying Chun, Ernest Chi Wai Chak and Billy Cheuk Sing Leung for their technical assistance. This study was supported by the CUHK direct grants (2007.2.045 and 2008.2.038).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Huang, RY., Li, MY., Hsin, M. et al. 4-Methylnitrosamino-1-3-pyridyl-1-butanone (NNK) promotes lung cancer cell survival by stimulating thromboxane A2 and its receptor. Oncogene 30, 106–116 (2011). https://doi.org/10.1038/onc.2010.390
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/onc.2010.390
Keywords
This article is cited by
-
Human tumor necrosis factor alpha-induced protein eight-like 1 exhibited potent anti-tumor effect through modulation of proliferation, survival, migration and invasion of lung cancer cells
Molecular and Cellular Biochemistry (2021)
-
Targeting lipid mediators in cancer biology
Cancer and Metastasis Reviews (2018)
-
SUMOylation and SENP3 regulate STAT3 activation in head and neck cancer
Oncogene (2016)
-
Single-molecule force spectroscopy study of the effect of cigarette carcinogens on thrombomodulin–thrombin interaction
Science Bulletin (2016)
-
Differential involvement of gp130 signalling pathways in modulating tobacco carcinogen-induced lung tumourigenesis
Oncogene (2015)