Abstract
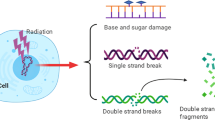
Recent reports implicate poly(ADP-ribose) polymerase-1 (PARP-1) in the activation of nuclear factor kappaB (NF-κB). We investigated the role of PARP-1 in the NF-κB signalling cascade induced by ionizing radiation (IR). AG14361, a potent PARP-1 inhibitor, was used in two breast cancer cell lines expressing different levels of constitutively activated NF-κB, as well as mouse embryonic fibroblasts (MEFs) proficient or deficient for PARP-1 or NF-κB p65. In the breast cancer cell lines, AG14361 had no effect on IR-induced degradation of IκBα or nuclear translocation of p50 or p65. However, AG14361 inhibited IR-induced NF-κB-dependent transcription of a luciferase reporter gene. Similarly, in PARP-1−/− MEFs, IR-induced nuclear translocation of p50 and p65 was normal, but κB binding and transcriptional activation did not occur. AG14361 sensitized both breast cancer cell lines to IR-induced cell killing, inhibited IR-induced XIAP expression and increased caspase-3 activity. However, AG14361 failed to increase IR-induced caspase activity when p65 was knocked down by siRNA. Consistent with this, AG14361 sensitized p65+/+ but not p65−/− MEFs to IR. We conclude that PARP-1 activity is essential in the upstream regulation of IR-induced NF-κB activation. These data indicate that potentiation of IR-induced cytotoxicity by AG14361 is mediated solely by inhibition of NF-κB activation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 50 print issues and online access
$259.00 per year
only $5.18 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Change history
26 January 2023
A Correction to this paper has been published: https://doi.org/10.1038/s41388-023-02605-w
References
Althaus FR, Hofferer L, Kleczkowska HE, Malanga M, Naegeli H, Panzeter PL et al. (1994). Histone shuttling by poly ADP-ribosylation. Mol Cell Biochem 138: 53–59.
Andela VB, Schwarz EM, Puzas JE, O’Keefe RJ, Rosier RN . (2000). Tumor metastasis and the reciprocal regulation of prometastatic and antimetastatic factors by nuclear factor kappaB. Cancer Res 60: 6557–6562.
Barkett M, Gilmore TD . (1999). Control of apoptosis by Rel/NF-kappaB transcription factors. Oncogene 18: 6910–6924.
Bassères DS, Baldwin AS . (2006). Nuclear factor-kappaB and inhibitor of kappaB kinase pathways in oncogenic initiation and progression. Oncogene 25: 6817–6830.
Beg AA, Baltimore D . (1996). An essential role for NF-kappaB in preventing TNF-alpha-induced cell death. Science 274: 782–784.
Biswas DK, Dai SC, Cruz A, Weiser B, Graner E, Pardee AB . (2001). The nuclear factor kappa B (NF-kappa B): a potential therapeutic target for estrogen receptor negative breast cancers. Proc Natl Acad Sci USA 98: 10386–10391.
Biswas DK, Shi Q, Baily S, Strickland I, Ghosh S, Pardee AB et al. (2004). NF-kappa B activation in human breast cancer specimens and its role in cell proliferation and apoptosis. Proc Natl Acad Sci USA 101: 10137–10142.
Brach M, Hass R, Sherman M, Gunji H, Weichselbaum R, Kufe D . (1991). Ionizing radiation induces expression and binding activity of the nuclear factor kB. J Clin Invest 88: 691–695.
Calabrese CR, Almassy R, Barton S, Batey MA, Calvert AH, Canan-Koch S et al. (2004). Anticancer chemosensitization and radiosensitization by the novel poly(ADP-ribose) polymerase-1 inhibitor AG14361. J Natl Cancer Inst 96: 56–67.
Cao Y, Karin M . (2003). NF-kappaB in mammary gland development and breast cancer. J Mammary Gland Biol Neoplasia 8: 215–223.
Cardoso SM, Oliveira CR . (2003). Inhibition of NF-kB renders cells more vulnerable to apoptosis induced by amyloid beta peptides. Free Radic Res 37: 967–973.
Carrillo A, Monreal Y, Ramirez P, Marin L, Parrilla P, Oliver FJ et al. (2004). Transcription regulation of TNF-alpha-early response genes by poly(ADP-ribose) polymerase-1 in murine heart endothelial cells. Nucleic Acids Res 32: 757–766.
Chalmers A, Johnston P, Woodcock M, Joiner M, Marples B . (2004). PARP-1, PARP-2, and the cellular response to low doses of ionizing radiation. Int J Radiat Oncol Biol Phys 58: 410–419.
Chang WJ, Alvarez-Gonzalez R . (2001). The sequence-specific DNA binding of NF-kappa B is reversibly regulated by the automodification reaction of poly (ADP-ribose) polymerase 1. J Biol Chem 276: 47664–47670.
Chiarugi A, Moskowitz MA . (2003). Poly(ADP-ribose) polymerase-1 activity promotes NF-kappaB-driven transcription and microglial activation: implication for neurodegenerative disorders. J Neurochem 85: 306–317.
Concin N, Zeillinger C, Tong D, Stimpfl M, Konig M, Printz D et al. (2003). Comparison of p53 mutational status with mRNA and protein expression in a panel of 24 human breast carcinoma cell lines. Breast Cancer Res Treat 79: 37–46.
Criswell T, Leskov K, Miyamoto S, Luo G, Boothman DA . (2003). Transcription factors activated in mammalian cells after clinically relevant doses of ionizing radiation. Oncogene 22: 5813–5827.
Dan HC, Sun M, Kaneko S, Feldman RI, Nicosia SV, Wang HG et al. (2004). Akt phosphorylation and stabilization of X-linked inhibitor of apoptosis protein (XIAP). J Biol Chem 279: 5405–5412.
Deveraux QL, Leo E, Stennicke HR, Welsh K, Salvesen GS, Read GC . (1999). Cleavage of human inhibitor of apoptosis protein XIAP results in fragments with distinct specificities for caspases. EMBO J 18: 5242–5251.
Ferreira C, van der Valk P, Span S, Jonker J, Postmus P, Kruyt F et al. (2001). Assessment of IAP (inhibitor of apoptosis) proteins as predictors of response to chemotherapy in advanced non-small-cell lung cancer patients. Ann Oncol 12: 799–805.
Ghosh S, Karin M . (2002). Missing pieces in the NF-kappaB puzzle. Cell 109 (Suppl): S81–S96.
Grube K, Kupper JH, Burkle A . (1991). Direct stimulation of poly(ADP ribose) polymerase in permeabilized cells by double-stranded DNA oligomers. Anal Biochem 193: 236–239.
Hassa PO, Covic M, Hasan S, Imhof R, Hottiger MO . (2001). The enzymatic and DNA binding activity of PARP-1 are not required for NF-kappa B coactivator function. J Biol Chem 276: 45588–45597.
Hassa PO, Haenni SS, Buerki C, Meier NI, Lane WS, Owen H et al. (2005). Acetylation of PARP-1 by p300/CBP regulates coactivation of NF-kappa B-dependent transcription. J Biol Chem 280: 40450–40464.
Hassa PO, Hottiger MO . (1999). A role of poly (ADP-ribose) polymerase in NF-kappaB transcriptional activation. J Biol Chem 380: 953–959.
Holcik N, Gibson H, Korneluk RG . (2001). XIAP: apoptotic brake and promising therapeutic target. Apoptosis 6: 253.
Jung M, Dritschilo A . (2001). NF-kappa B signaling pathway as a target for human tumor radiosensitization. Semin Radiat Oncol 11: 346–351.
Kraus W, Lis J . (2003). PARP goes transcription. Cell 113: 677–683.
Martin-Oliva D, Aguilar-Quesada R, O’valle F, Munoz-Gamez JA, Martinez-Romero R, Garcia Del Moral R et al. (2006). Inhibition of poly(ADP-ribose) polymerase modulates tumor-related gene expression, including hypoxia-inducible factor-1 activation, during skin carcinogenesis. Cancer Res 66: 5744–5756.
Nakajima H, Nagaso H, Kakui N, Ishikawa M, Hiranuma T, Hoshiko S . (2004). Critical role of the automodification of poly(ADP-ribose) polymerase-1 in nuclear factor-kappaB-dependent gene expression in primary cultured mouse glial cells. J Biol Chem 279: 42774–42786.
Nakshatri H, Bhat-Nakshatri P, Martin DA, Goulet Jr RJ, Sledge Jr GW . (1997). Constitutive activation of NF-kappaB during progression of breast cancer to hormone-independent growth. Mol Cell Biol 17: 3629–3639.
Oliver FJ, Menissier-de Murcia J, Nacci C, Decker P, Andriantsitohaina R, Muller S et al. (1999). Resistance to endotoxic shock as a consequence of defective NF-kappaB activation in poly (ADP-ribose) polymerase-1 deficient mice. EMBO J 18: 4446–4454.
Pande V, Ramos MJ . (2005). NF-kappaB in human disease: current inhibitors and prospects for de novo structure based design of inhibitors. Curr Med Chem 12: 357–374.
Patel NM, Nozaki S, Shortle NH, Bhat-Nakshatri P, Newton TR, Rice S et al. (2000). Paclitaxel sensitivity of breast cancer cells with constitutively active NF-kappaB is enhanced by IkappaBalpha super-repressor and parthenolide. Oncogene 19: 4159–4169.
Penolazzi L, Lambertini E, Borgatti M . (2003). Decoy oligodeoxynucleotides targeting NFkB transcription factors: induction of apoptosis in human primary osteoclasts. Biochem Pharmacol 66: 1189–1198.
Perkins ND . (2006). Good cop, bad cop: the different faces of NF-kappaB. Oncogene 25: 6717–6730.
Pratt MA, Bishop TE, White D, Yasvinski G, Menard M, Niu MY et al. (2003). Estrogen withdrawal-induced NF-kappaB activity and bcl-3 expression in breast cancer cells: roles in growth and hormone independence. Mol Cell Biol 23: 6887–6900.
Raju U, Gumin GJ, Noel F, Tofilon PJ . (1998). IkappaBalpha degradation is not a requirement for the X-ray-induced activation of nuclear factor kappaB in normal rat astrocytes and human brain tumour cells. Int J Radiat Biol 74: 617–624.
Rayet B, Gelinas C . (1999). Aberrant rel/nfkb genes and activity in human cancer. Oncogene 18: 6938–6947.
Russo SM, Tepper JE, Baldwin Jr AS, Liu R, Adams J, Elliott P et al. (2001). Enhancement of radiosensitivity by proteasome inhibition: implications for a role of NF-kappaB. Int J Radiat Oncol Biol Phys 50: 183–193.
Scott FL, Denault JB, Riedl SJ, Shin H, Renatus M, Salvesen GS . (2005). XIAP inhibits caspase-3 and -7 using two binding sites: evolutionarily conserved mechanism of IAPs. EMBO J 24: 645–655.
Skalitzky DJ, Marakovits JT, Maegley KA, Ekker A, Yu XH, Hostomsky Z et al. (2003). Tricyclic benzimidazoles as potent poly(ADP-ribose) polymerase-1 inhibitors. J Med Chem 46: 210–213.
Smith S . (2001). The world according to PARP. Trends Biochem Sci 26: 174–179.
Sovak MA, Bellas RE, Kim DW, Zanieski GJ, Rogers AE, Traish AM et al. (1997). Aberrant nuclear factor-kappaB/Rel expression and the pathogenesis of breast cancer. J Clin Invest 100: 2952–2960.
Veuger SJ, Curtin NJ, Richardson CJ, Smith GC, Durkacz BW . (2003). Radiosensitization and DNA repair inhibition by the combined use of novel inhibitors of DNA-dependent protein kinase and poly(ADP-ribose) polymerase-1. Cancer Res 63: 6008–6015.
Wang CY, Mayo MW, Baldwin Jr AS . (1996). TNF- and cancer therapy-induced apoptosis: potentiation by inhibition of NF-kappaB. Science 274: 784–787.
Wang CY, Mayo MW, Korneluk RG, Goeddel DV, Baldwin Jr AS . (1998). NF-kappaB antiapoptosis: induction of TRAF1 and TRAF2 and c-IAP1 and c-IAP2 to suppress caspase-8 activation. Science 281: 1680–1683.
Webster GA, Perkins ND . (1999). Transcriptional cross talk between NF-kappaB and p53. Mol Cell Biol 19: 3485–3495.
Wu JT, Kral JG . (2005). The NF-kappaB/IkappaB signaling system: a molecular target in breast cancer therapy. J Surg Res 123: 158–169.
Xiao CW, Ash K, Tsang BK . (2001). Nuclear factor-kappaB-mediated X-linked inhibitor of apoptosis protein expression prevents rat granulosa cells from tumor necrosis factor alpha-induced apoptosis. Endocrinology 142: 557–563.
Yang L, Cao Z, Yan H, Wood W . (2003). Coexistence of high levels of apoptotic signalling and inhibitor of apoptosis proteins in human tumour cells: Implications for cancer specific therapy. Cancer Research 63: 6815–6824.
Zhou Y, Eppenberger-Castori S, Marx C, Yau C, Scott GK, Eppenberger U et al. (2005). Activation of nuclear factor-kappaB (NFkappaB) identifies a high-risk subset of hormone-dependent breast cancers. Int J Biochem Cell Biol 37: 1130–1144.
Acknowledgements
This work was supported by the Breast Cancer Campaign, UK and Cancer Research UK.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on the Oncogene website (http://www.nature.com/onc)
Supplementary information
Rights and permissions
About this article
Cite this article
Veuger, S., Hunter, J. & Durkacz, B. Ionizing radiation-induced NF-κB activation requires PARP-1 function to confer radioresistance. Oncogene 28, 832–842 (2009). https://doi.org/10.1038/onc.2008.439
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/onc.2008.439
Keywords
This article is cited by
-
Mitochondrial metabolism: a predictive biomarker of radiotherapy efficacy and toxicity
Journal of Cancer Research and Clinical Oncology (2023)
-
SPINDOC binds PARP1 to facilitate PARylation
Nature Communications (2021)
-
Reduction of metastatic potential by inhibiting EGFR/Akt/p38/ERK signaling pathway and epithelial-mesenchymal transition after carbon ion exposure is potentiated by PARP-1 inhibition in non-small-cell lung cancer
BMC Cancer (2019)
-
The convergent roles of NF-κB and ER stress in sunitinib-mediated expression of pro-tumorigenic cytokines and refractory phenotype in renal cell carcinoma
Cell Death & Disease (2018)
-
mGluR5 mediates post-radiotherapy fatigue development in cancer patients
Translational Psychiatry (2018)