Key Points
-
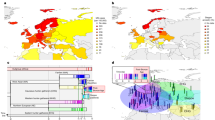
Epstein–Barr virus (EBV) infection, smoking, low vitamin D and lack of sun exposure are well established factors associated with risk of multiple sclerosis (MS); recently, adolescent obesity has been added to this list
-
Less established factors include exposure to organic solvents and night shift work, which associate with increased risk, whereas oral tobacco use, cytomegalovirus infection, alcohol use and coffee consumption associate with decreased risk
-
Some of these factors should be considered in primary prevention
-
Most lifestyle and environmental factors seem to have the greatest effect during a particular time window — adolescence
-
Certain factors, such as EBV infection, smoking and adolescent obesity interact with human leukocyte antigen MS risk genes, with substantial risk increases in individuals who carry genes that predispose them to MS
-
The interaction with these immune response genes provides strong evidence that these lifestyle and environmental factors act on adaptive immunity, leading to autoimmune attack on the nervous system
Abstract
Genetic predisposition to multiple sclerosis (MS) only explains a fraction of the disease risk; lifestyle and environmental factors are key contributors to the risk of MS. Importantly, these nongenetic factors can influence pathogenetic pathways, and some of them can be modified. Besides established MS-associated risk factors — high latitude, female sex, smoking, low vitamin D levels caused by insufficient sun exposure and/or dietary intake, and Epstein–Barr virus (EBV) infection — strong evidence now supports obesity during adolescence as a factor increasing MS risk. Organic solvents and shift work have also been reported to confer increased risk of the disease, whereas factors such as use of nicotine or alcohol, cytomegalovirus infection and a high coffee consumption are associated with a reduced risk. Certain factors — smoking, EBV infection and obesity — interact with HLA risk genes, pointing at a pathogenetic pathway involving adaptive immunity. All of the described risk factors for MS can influence adaptive and/or innate immunity, which is thought to be the main pathway modulated by MS risk alleles. Unlike genetic risk factors, many environmental and lifestyle factors can be modified, with potential for prevention, particularly for people at the greatest risk, such as relatives of individuals with MS. Here, we review recent data on environmental and lifestyle factors, with a focus on gene–environment interactions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Marrie, R. A., Yu, N., Wei, Y., Elliott, L. & Blanchard, J. High rates of physician services utilization at least five years before multiple sclerosis diagnosis. Mult. Scler. 19, 1113–1119 (2013).
Hughes, A. M. et al. Early-life hygiene-related factors affect risk of central nervous system demyelination and asthma differentially. Clin. Exp. Immunol. 172, 466–474 (2013).
Hedstrom, A. K., Hillert, J., Olsson, T. & Alfredsson, L. Reverse causality behind the association between reproductive history and MS. Mult. Scler. 20, 406–411 (2014).
Nielsen, N. M. et al. Reproductive history and risk of multiple sclerosis. Epidemiology 22, 546–552 (2011).
Ascherio, A., Munger, K. L. & Lunemann, J. D. The initiation and prevention of multiple sclerosis. Nat. Rev. Neurol. 8, 602–612 (2012).
Lucas, R. M., Byrne, S. N., Correale, J., Ilschner, S. & Hart, P. H. Ultraviolet radiation, vitamin D and multiple sclerosis. Neurodegener. Dis. Manag. 5, 413–424 (2015).
Sawcer, S. The complex genetics of multiple sclerosis: pitfalls and prospects. Brain 131, 3118–3131 (2008).
van der Mei, I. et al. Population attributable fractions and joint effects of key risk factors for multiple sclerosis. Mult. Scler. 22, 461–469 (2016).
O'Gorman, C., Lin, R., Stankovich, J. & Broadley, S. A. Modelling genetic susceptibility to multiple sclerosis with family data. Neuroepidemiology 40, 1–12 (2013).
Westerlind, H. et al. Modest familial risks for multiple sclerosis: a registry-based study of the population of Sweden. Brain 137, 770–778 (2014).
Westerlind, H. et al. Identity-by-descent mapping in a Scandinavian multiple sclerosis cohort. Eur. J. Hum. Genet. 23, 688–692 (2015).
Simpson, S. et al. Latitude is significantly associated with the prevalence of multiple sclerosis: a meta-analysis. J. Neurol. Neurosurg. Psychiatry 82, 1132–1141 (2011).
Gale, C. R. & Martyn, C. N. Migrant studies in multiple sclerosis. Prog. Neurobiol. 47, 425–448 (1995).
Berg-Hansen, P. et al. Prevalence of multiple sclerosis among immigrants in Norway. Mult. Scler. 21, 695–702 (2015).
Ahlgren, C., Oden, A. & Lycke, J. A nationwide survey of the prevalence of multiple sclerosis in immigrant populations of Sweden. Mult. Scler. 18, 1099–1107 (2012).
Ahlgren, C., Lycke, J., Oden, A. & Andersen, O. High risk of MS in Iranian immigrants in Gothenburg, Sweden. Mult. Scler. 16, 1079–1082 (2010).
Montgomery, S. M., Lambe, M., Olsson, T. & Ekbom, A. Parental age, family size, and risk of multiple sclerosis. Epidemiology 15, 717–723 (2004).
van der Mei, I. A. et al. Human leukocyte antigen-DR15, low infant sibling exposure and multiple sclerosis: gene-environment interaction. Ann. Neurol. 67, 261–265 (2010).
Barnett, M. H., McLeod, J. G., Hammond, S. R. & Kurtzke, J. F. Migration and multiple sclerosis in immigrants from United Kingdom and Ireland to Australia: a reassessment. III: risk of multiple sclerosis in UKI immigrants and Australian-born in Hobart, Tasmania. J. Neurol. 263, 792–798 (2016).
Koch-Henriksen, N. & Sorensen, P. S. The changing demographic pattern of multiple sclerosis epidemiology. Lancet Neurol. 9, 520–532 (2010).
Westerlind, H. et al. New data identify an increasing sex ratio of multiple sclerosis in Sweden. Mult. Scler. 20, 1578–1583 (2014).
Ponsonby, A. L. et al. Offspring number, pregnancy, and risk of a first clinical demyelinating event: the AusImmune Study. Neurology 78, 867–874 (2012).
Magyari, M., Koch-Henriksen, N., Pfleger, C. C. & Sorensen, P. S. Reproduction and the risk of multiple sclerosis. Mult. Scler. 19, 1604–1609 (2013).
Brodin, P. et al. Variation in the human immune system is largely driven by non-heritable influences. Cell 160, 37–47 (2015).
Roshanisefat, H., Bahmanyar, S., Hillert, J., Olsson, T. & Montgomery, S. Shared genetic factors may not explain the raised risk of comorbid inflammatory diseases in multiple sclerosis. Mult. Scler. 18, 1430–1436 (2012).
Sawcer, S. et al. Genetic risk and a primary role for cell-mediated immune mechanisms in multiple sclerosis. Nature 476, 214–219 (2011).
Brynedal, B. et al. HLA-A confers an HLA-DRB1 independent influence on the risk of multiple sclerosis. PLoS ONE 2, e664 (2007).
Beecham, A. H. et al. Analysis of immune-related loci identifies 48 new susceptibility variants for multiple sclerosis. Nat. Genet. 45, 1353–1360 (2013).
Moutsianas, L. et al. Class II HLA interactions modulate genetic risk for multiple sclerosis. Nat. Genet. 47, 1107–1113 (2015).
Rothman, K. J., Greenland, S. & Walker, A. M. Concepts of interaction. Am. J. Epidemiol. 112, 467–470 (1980).
Rothman, K. J., Greenland, S. & Lash, T. L. (eds) in Modern Epidemiology. 3rd edn Ch. 3 pp. 71–83 (Lippincott Williams & Wilkins, 2008).
Hawkes, C. H. Smoking is a risk factor for multiple sclerosis: a metanalysis. Mult. Scler. 13, 610–615 (2007).
Handel, A. E. et al. Smoking and multiple sclerosis: an updated meta-analysis. PLoS ONE 6, e16149 (2011).
Hedstrom, A. K., Baarnhielm, M., Olsson, T. & Alfredsson, L. Tobacco smoking, but not Swedish snuff use, increases the risk of multiple sclerosis. Neurology 73, 696–701 (2009).
Ghadirian, P., Dadgostar, B., Azani, R. & Maisonneuve, P. A case-control study of the association between socio-demographic, lifestyle and medical history factors and multiple sclerosis. Can. J. Public Health 92, 281–285 (2001).
Salzer, J. et al. Smoking as a risk factor for multiple sclerosis. Mult. Scler. 19, 1022–1027 (2013).
Hedstrom, A. K., Baarnhielm, M., Olsson, T. & Alfredsson, L. Exposure to environmental tobacco smoke is associated with increased risk for multiple sclerosis. Mult. Scler. 17, 788–793 (2011).
Heydarpour, P. et al. Potential impact of air pollution on multiple sclerosis in Tehran, Iran. Neuroepidemiology 43, 233–238 (2014).
Barragan-Martinez, C. et al. Organic solvents as risk factor for autoimmune diseases: a systematic review and meta-analysis. PLoS ONE 7, e51506 (2012).
Hedstrom, A. et al. Smokers run increased risk of developing anti-natalizumab antibodies. Mult. Scler. 20, 1081–1085 (2013).
Hedstrom, A. K. et al. Smoking and risk of treatment-induced neutralizing antibodies to interferon β-1a. Mult. Scler. 20, 445–450 (2014).
Chinoy, H. et al. Interaction of HLA-DRB1*03 and smoking for the development of anti-Jo-1 antibodies in adult idiopathic inflammatory myopathies: a European-wide case study. Ann. Rheum. Dis. 71, 961–965 (2012).
Klareskog, L., Catrina, A. I. & Paget, S. Rheumatoid arthritis. Lancet 373, 659–672 (2009).
Hedstrom, A. K., Hillert, J., Olsson, T. & Alfredsson, L. Nicotine might have a protective effect in the etiology of multiple sclerosis. Mult. Scler. 19, 1009–1013 (2013).
Nizri, E. et al. Activation of the cholinergic anti-inflammatory system by nicotine attenuates neuroinflammation via suppression of TH1 and TH17 responses. J. Immunol. 183, 6681–6688 (2009).
Shan, M. et al. Lung myeloid dendritic cells coordinately induce TH1 and TH17 responses in human emphysema. Sci. Transl. Med. 1, 4ra10 (2009).
Odoardi, F. et al. T cells become licensed in the lung to enter the central nervous system. Nature 488, 675–679 (2012).
Hedstrom, A. K. et al. Smoking and two human leukocyte antigen genes interact to increase the risk for multiple sclerosis. Brain 134, 653–664 (2011).
Hedstrom, A. K. et al. Interaction between passive smoking and two HLA genes with regard to multiple sclerosis risk. Int. J. Epidemiol. 43, 1791–1798 (2014).
Briggs, F. B. et al. Smoking and risk of multiple sclerosis: evidence of modification by NAT1 variants. Epidemiology 25, 605–614 (2014).
Friese, M. A. & Fugger, L. Autoreactive CD8+ T cells in multiple sclerosis: a new target for therapy? Brain 128, 1747–1763 (2005).
Friese, M. A. et al. Opposing effects of HLA class I molecules in tuning autoreactive CD8+ T cells in multiple sclerosis. Nat. Med. 14, 1227–1235 (2008).
Dendrou, C. A., Fugger, L. & Friese, M. A. Immunopathology of multiple sclerosis. Nat. Rev. Immunol. 15, 545–558 (2015).
Mustafa, M. et al. The major histocompatibility complex influences myelin basic protein 63-88-induced T cell cytokine profile and experimental autoimmune encephalomyelitis. Eur. J. Immunol. 23, 3089–3095 (1993).
Mustafa, M. et al. Protective influences on experimental autoimmune encephalomyelitis by MHC class I and class II alleles. J. Immunol. 153, 3337–3344 (1994).
Issazadeh, S., Kjellen, P., Olsson, T., Mustafa, M. & Holmdahl, R. Major histocompatibility complex-controlled protective influences on experimental autoimmune encephalomyelitis are peptide specific. Eur. J. Immunol. 27, 1584–1587 (1997).
Hedstrom, A. K., Olsson, T. & Alfredsson, L. Smoking is a major preventable risk factor for multiple sclerosis. Mult. Scler. 22, 1021–1026 (2016).
Sundstrom, P. & Nystrom, L. Smoking worsens the prognosis in multiple sclerosis. Mult. Scler. 14, 1031–1035 (2008).
Correale, J. & Farez, M. F. Smoking worsens multiple sclerosis prognosis: two different pathways are involved. J. Neuroimmunol. 281, 23–34 (2015).
Di Pauli, F. et al. Smoking is a risk factor for early conversion to clinically definite multiple sclerosis. Mult. Scler. 14, 1026–1030 (2008).
Healy, B. C. et al. Smoking and disease progression in multiple sclerosis. Arch. Neurol. 66, 858–864 (2009).
Hernan, M. A. et al. Cigarette smoking and the progression of multiple sclerosis. Brain 128, 1461–1465 (2005).
Pittas, F. et al. Smoking is associated with progressive disease course and increased progression in clinical disability in a prospective cohort of people with multiple sclerosis. J. Neurol. 256, 577–585 (2009).
Manouchehrinia, A. et al. Tobacco smoking and disability progression in multiple sclerosis: United Kingdom cohort study. Brain 136, 2298–2304 (2013).
Zivadinov, R. et al. Smoking is associated with increased lesion volumes and brain atrophy in multiple sclerosis. Neurology 73, 504–510 (2009).
Manouchehrinia, A., Weston, M., Tench, C. R., Britton, J. & Constantinescu, C. S. Tobacco smoking and excess mortality in multiple sclerosis: a cohort study. J. Neurol. Neurosurg. Psychiatry 85, 1091–1095 (2014).
Ramanujam, R. et al. Effect of smoking cessation on multiple sclerosis prognosis. JAMA Neurol. 72, 1117–1123 (2015).
Handel, A. E. et al. An updated meta-analysis of risk of multiple sclerosis following infectious mononucleosis. PLoS ONE 5, e12496 (2010).
Sundstrom, P., Nystrom, M., Ruuth, K. & Lundgren, E. Antibodies to specific EBNA-1 domains and HLA DRB1*1501 interact as risk factors for multiple sclerosis. J. Neuroimmunol. 215, 102–107 (2009).
Sundqvist, E. et al. Epstein-Barr virus and multiple sclerosis: interaction with HLA. Genes Immun. 13, 14–20 (2012).
Levin, L. I., Munger, K. L., O'Reilly, E. J., Falk, K. I. & Ascherio, A. Primary infection with the Epstein-Barr virus and risk of multiple sclerosis. Ann. Neurol. 67, 824–830 (2010).
Ascherio, A. & Munger, K. L. EBV and autoimmunity. Curr. Top. Microbiol. Immunol. 390, 365–385 (2015).
Makhani, N. et al. Viral exposures and MS outcome in a prospective cohort of children with acquired demyelination. Mult. Scler. 22, 385–388 (2016).
Zhou, Y. et al. Genetic loci for Epstein-Barr virus nuclear antigen-1 are associated with risk of multiple sclerosis. Mult. Scler. (2016).
Nielsen, T. R. et al. Effects of infectious mononucleosis and HLA-DRB1*15 in multiple sclerosis. Mult. Scler. 15, 431–436 (2009).
Hedstrom, A. K., Lima Bomfim, I., Hillert, J., Olsson, T. & Alfredsson, L. Obesity interacts with infectious mononucleosis in risk of multiple sclerosis. Eur. J. Neurol. 22, 578–e538 (2015).
Serafini, B. et al. Dysregulated Epstein-Barr virus infection in the multiple sclerosis brain. J. Exp. Med. 204, 2899–2912 (2007).
Lassmann, H., Niedobitek, G., Aloisi, F. & Middeldorp, J. M. Epstein–Barr virus in the multiple sclerosis brain: a controversial issue—report on a focused workshop held in the Centre for Brain Research of the Medical University of Vienna, Austria. Brain 134, 2772–2786 (2011).
Hauser, S. L. et al. B-Cell depletion with rituximab in relapsing-remitting multiple sclerosis. N. Engl. J. Med. 358, 676–688 (2008).
Sundqvist, E. et al. JC polyomavirus infection is strongly controlled by human leucocyte antigen class II variants. PLoS Pathog. 10, e1004084 (2014).
Staras, S. A. et al. Seroprevalence of cytomegalovirus infection in the United States, 1988–1994. Clin. Infect. Dis. 43, 1143–1151 (2006).
Waubant, E. et al. Common viruses associated with lower pediatric multiple sclerosis risk. Neurology 76, 1989–1995 (2011).
Waubant, E. et al. Antibody response to common viruses and human leukocyte antigen-DRB1 in pediatric multiple sclerosis. Mult. Scler. 19, 891–895 (2013).
Sundqvist, E. et al. Cytomegalovirus seropositivity is negatively associated with multiple sclerosis. Mult. Scler. 20, 165–173 (2014).
Ascherio, A. et al. Epstein–Barr virus antibodies and risk of multiple sclerosis: a prospective study. JAMA 286, 3083–3088 (2001).
Levin, L. I. et al. Temporal relationship between elevation of Epstein–Barr virus antibody titers and initial onset of neurological symptoms in multiple sclerosis. JAMA 293, 2496–2500 (2005).
DeLorenze, G. N. et al. Epstein–Barr virus and multiple sclerosis: evidence of association from a prospective study with long-term follow-up. Arch. Neurol. 63, 839–844 (2006).
Chidrawar, S. et al. Cytomegalovirus-seropositivity has a profound influence on the magnitude of major lymphoid subsets within healthy individuals. Clin. Exp. Immunol. 155, 423–432 (2009).
Munger, K. L. et al. Molecular mechanism underlying the impact of vitamin D on disease activity of MS. Ann. Clin. Transl. Neurol. 1, 605–617 (2014).
Kampman, M. T., Wilsgaard, T. & Mellgren, S. I. Outdoor activities and diet in childhood and adolescence relate to MS risk above the Arctic Circle. J. Neurol. 254, 471–477 (2007).
Baarnhielm, M. et al. Sunlight is associated with decreased multiple sclerosis risk: no interaction with human leukocyte antigen-DRB1*15. Eur. J. Neurol. 19, 955–962 (2012).
Becklund, B. R., Severson, K. S., Vang, S. V. & DeLuca, H. F. UV radiation suppresses experimental autoimmune encephalomyelitis independent of vitamin D production. Proc. Natl. Acad. Sci. U. S. A. 107, 6418–6423 (2010).
Rana, S., Rogers, L. J. & Halliday, G. M. Systemic low-dose UVB inhibits CD8 T cells and skin inflammation by alternative and novel mechanisms. Am. J. Pathol. 178, 2783–2791 (2011).
Breuer, J. et al. Ultraviolet B light attenuates the systemic immune response in central nervous system autoimmunity. Ann. Neurol. 75, 739–758 (2014).
Navid, F. et al. The aryl hydrocarbon receptor is involved in UVR-induced immunosuppression. J. Invest. Dermatol. 133, 2763–2770 (2013).
Correale, J. & Farez, M. F. Modulation of multiple sclerosis by sunlight exposure: role of cis-urocanic acid. J. Neuroimmunol. 261, 134–140 (2013).
Munger, K. L., Levin, L. I., Hollis, B. W., Howard, N. S. & Ascherio, A. Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis. JAMA 296, 2832–2838 (2006).
Cortese, M. et al. Timing of use of cod liver oil, a vitamin D source, and multiple sclerosis risk: the EnvIMS study. Mult. Scler. 21, 1856–1864 (2015).
Bjornevik, K. et al. Sun exposure and multiple sclerosis risk in Norway and Italy: the EnvIMS study. Mult. Scler. 20, 1042–1049 (2014).
Baarnhielm, M., Olsson, T. & Alfredsson, L. Fatty fish intake is associated with decreased occurrence of multiple sclerosis. Mult. Scler. 20, 726–732 (2014).
Sandberg, L. et al. Vitamin D and axonal injury in multiple sclerosis. Mult. Scler. 22, 1027–1031 (2015).
Ueda, P. et al. Neonatal vitamin D status and risk of multiple sclerosis. Ann. Neurol. 76, 338–346 (2014).
Adzemovic, M. Z., Zeitelhofer, M., Hochmeister, S., Gustafsson, S. A. & Jagodic, M. Efficacy of vitamin D in treating multiple sclerosis-like neuroinflammation depends on developmental stage. Exp. Neurol. 249, 39–48 (2013).
Munger, K. L. et al. Vitamin D status during pregnancy and risk of multiple sclerosis in offspring of women in the Finnish maternity cohort. JAMA Neurol. 73, 515–519 (2016).
Staples, J., Ponsonby, A. L. & Lim, L. Low maternal exposure to ultraviolet radiation in pregnancy, month of birth, and risk of multiple sclerosis in offspring: longitudinal analysis. BMJ 340, c1640 (2010).
Sundqvist, E. et al. Confirmation of association between multiple sclerosis and CYP27B1. Eur. J. Hum. Genet. 18, 1349–1352 (2010).
Rhead, B. et al. Mendelian randomization shows a causal effect of low vitamin D on multiple sclerosis risk. Neurol. Genet. 2, e97 (2016).
Mokry, L. E. et al. Vitamin D and risk of multiple sclerosis: a Mendelian randomization study. PLoS Med. 12, e1001866 (2015).
Handunnetthi, L., Ramagopalan, S. V. & Ebers, G. C. Multiple sclerosis, vitamin D, and HLA-DRB1*15. Neurology 74, 1905–1910 (2010).
Ascherio, A. et al. Vitamin D as an early predictor of multiple sclerosis activity and progression. JAMA Neurol. 71, 306–314 (2014).
Fitzgerald, K. C. et al. Association of vitamin D levels with multiple sclerosis activity and progression in patients receiving interferon Beta-1b. JAMA Neurol. 72, 1458–1465 (2015).
Munger, K. L., Chitnis, T. & Ascherio, A. Body size and risk of MS in two cohorts of US women. Neurology 73, 1543–1550 (2009).
Munger, K. L. et al. Childhood body mass index and multiple sclerosis risk: a long-term cohort study. Mult. Scler. 19, 1323–1329 (2013).
Hedstrom, A. K. et al. Interaction between adolescent obesity and HLA risk genes in the etiology of multiple sclerosis. Neurology 82, 865–872 (2014).
Gianfrancesco, M. A. et al. Obesity during childhood and adolescence increases susceptibility to multiple sclerosis after accounting for established genetic and environmental risk factors. Obes. Res. Clin. Pract. 8, e435–447 (2014).
Langer-Gould, A., Brara, S. M., Beaber, B. E. & Koebnick, C. Childhood obesity and risk of pediatric multiple sclerosis and clinically isolated syndrome. Neurology 80, 548–552 (2013).
Hedstrom, A. K., Olsson, T. & Alfredsson, L. Body mass index during adolescence, rather than childhood, is critical in determining MS risk. Mult. Scler. 22, 878–883 (2016).
Wesnes, K. et al. Body size and the risk of multiple sclerosis in Norway and Italy: the EnvIMS study. Mult. Scler. 21, 388–395 (2015).
Mokry, L. E. et al. Obesity and multiple sclerosis: a Mendelian randomization study. PLoS Med. 13, e1002053 (2016).
Gianfrancesco, M. A. et al. Genetic variants associated with body mass index demonstrate a causal effect on multiple sclerosis susceptibility. Am. J. Epidemiol. In press http://dx.doi.org/10.1093/aje/kww120 (2016).
Lumeng, C. N., Bodzin, J. L. & Saltiel, A. R. Obesity induces a phenotypic switch in adipose tissue macrophage polarization. J. Clin. Invest. 117, 175–184 (2007).
Procaccini, C., Pucino, V., Mantzoros, C. S. & Matarese, G. Leptin in autoimmune diseases. Metabolism 64, 92–104 (2015).
Matarese, G. et al. Leptin increase in multiple sclerosis associates with reduced number of CD4+CD25+ regulatory T cells. Proc. Natl Acad. Sci. USA. 102, 5150–5155 (2005).
Matarese, G., Carrieri, P. B., Montella, S., De Rosa, V. & La Cava, A. Leptin as a metabolic link to multiple sclerosis. Nat. Rev. Neurol. 6, 455–461 (2010).
Wortsman, J., Matsuoka, L. Y., Chen, T. C., Lu, Z. & Holick, M. F. Decreased bioavailability of vitamin D in obesity. Am. J. Clin. Nutr. 72, 690–693 (2000).
Karlsson, E. A. & Beck, M. A. The burden of obesity on infectious disease. Exp. Biol. Med. (Maywood) 235, 1412–1424 (2010).
Paich, H. A. et al. Overweight and obese adult humans have a defective cellular immune response to pandemic H1N1 influenza A virus. Obesity (Silver Spring) 21, 2377–2386 (2013).
Magrini, A. et al. Shift work and autoimmune thyroid disorders. Int. J. Immunopathol. Pharmacol. 19, 31–36 (2006).
Hedstrom, A. K., Akerstedt, T., Hillert, J., Olsson, T. & Alfredsson, L. Shift work at young age is associated with increased risk for multiple sclerosis. Ann. Neurol. 70, 733–741 (2011).
Hedstrom, A., Akerstedt, T., Olsson, T. & Alfredsson, L. Shift work influences multiple sclerosis risk. Mult. Scler. 21, 1195–1199 (2015).
Hansson, I., Holmdahl, R. & Mattsson, R. Constant darkness enhances autoimmunity to type II collagen and exaggerates development of collagen-induced arthritis in DBA/1 mice. J. Neuroimmunol. 27, 79–84 (1990).
Farez, M. F. et al. Melatonin contributes to the seasonality of multiple sclerosis relapses. Cell 162, 1338–1352 (2015).
Hansson, I., Holmdahl, R. & Mattsson, R. Pinealectomy ameliorates collagen II-induced arthritis in mice. Clin. Exp. Immunol. 92, 432–436 (1993).
Massa, J., O'Reilly, E. J., Munger, K. L. & Ascherio, A. Caffeine and alcohol intakes have no association with risk of multiple sclerosis. Mult. Scler. 19, 53–58 (2013).
Hedstrom, A. K., Hillert, J., Olsson, T. & Alfredsson, L. Alcohol as a modifiable lifestyle factor affecting multiple sclerosis risk. JAMA Neurol. 71, 300–305 (2014).
Kallberg, H. et al. Alcohol consumption is associated with decreased risk of rheumatoid arthritis: results from two Scandinavian case-control studies. Ann. Rheum. Dis. 68, 222–227 (2009).
Hedstrom, A. K. et al. High consumption of coffee is associated with decreased multiple sclerosis risk; results from two independent studies. J. Neurol. Neurosurg. Psychiatry 87, 454–460 (2016).
Chen, G. Q. et al. Chronic caffeine treatment attenuates experimental autoimmune encephalomyelitis induced by guinea pig spinal cord homogenates in Wistar rats. Brain Res. 1309, 116–125 (2010).
Horrigan, L. A., Kelly, J. P. & Connor, T. J. Immunomodulatory effects of caffeine: friend or foe? Pharmacol. Ther. 111, 877–892 (2006).
Kleinewietfeld, M. et al. Sodium chloride drives autoimmune disease by the induction of pathogenic TH17 cells. Nature 496, 518–522 (2013).
Wu, C. et al. Induction of pathogenic TH17 cells by inducible salt-sensing kinase SGK1. Nature 496, 513–517 (2013).
Farez, M. F., Fiol, M. P., Gaitan, M. I., Quintana, F. J. & Correale, J. Sodium intake is associated with increased disease activity in multiple sclerosis. J. Neurol. Neurosurg. Psychiatry 86, 26–31 (2015).
Berer, K. et al. Commensal microbiota and myelin autoantigen cooperate to trigger autoimmune demyelination. Nature 479, 538–541 (2011).
Correale, J. & Farez, M. F. The impact of environmental infections (parasites) on MS activity. Mult. Scler. 17, 1162–1169 (2011).
Zhang, D. et al. Genetic control of individual differences in gene-specific methylation in human brain. Am. J. Hum. Genet. 86, 411–419 (2010).
Liu, Y. et al. GeMes, clusters of DNA methylation under genetic control, can inform genetic and epigenetic analysis of disease. Am. J. Hum. Genet. 94, 485–495 (2014).
Gao, X., Jia, M., Zhang, Y., Breitling, L. P. & Brenner, H. DNA methylation changes of whole blood cells in response to active smoking exposure in adults: a systematic review of DNA methylation studies. Clin. Epigenetics 7, 113 (2015).
Mastronardi, F. G. et al. Increased citrullination of histone H3 in multiple sclerosis brain and animal models of demyelination: a role for tumor necrosis factor-induced peptidylarginine deiminase 4 translocation. J. Neurosci. 26, 11387–11396 (2006).
Baranzini, S. E. et al. Genome, epigenome and RNA sequences of monozygotic twins discordant for multiple sclerosis. Nature 464, 1351–1356 (2010).
Pedre, X. et al. Changed histone acetylation patterns in normal-appearing white matter and early multiple sclerosis lesions. J. Neurosci. 31, 3435–3445 (2011).
Graves, M. C. et al. Methylation differences at the HLA-DRB1 locus in CD4+ T-Cells are associated with multiple sclerosis. Mult. Scler. 20, 1033–1041 (2014).
Huynh, J. L. et al. Epigenome-wide differences in pathology-free regions of multiple sclerosis-affected brains. Nat. Neurosci. 17, 121–130 (2014).
Bos, S. D. et al. Genome-wide DNA methylation profiles indicate CD8+ T cell hypermethylation in multiple sclerosis. PLoS ONE 10, e0117403 (2015).
Maltby, V. E. et al. Genome-wide DNA methylation profiling of CD8+ T cells shows a distinct epigenetic signature to CD4+ T cells in multiple sclerosis patients. Clin. Epigenetics 7, 118 (2015).
Acknowledgements
We thank Mohsen Khademi for preparing the schematic figures and Maja Jagodic for input on the epigenetics section. The original studies by T.O. cited in the text have been supported by the Swedish Research Council, the Knut and Alice Wallenberg foundation, the AFA foundation, the Swedish Brain Foundation, Margareta af Ugglas Foundation and the EUfp7 Neurinox 2012–278611. L.A. has received grants for multiple sclerosis research from the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare and the Swedish Brain Foundation.
Author information
Authors and Affiliations
Contributions
All authors researched data for article, and provided substantial contribution to discussion of content, writing, reviewing and editing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
T.O. has received honoraria for lectures and/or advisory boards as well as unrestricted multiple sclerosis research grants from Allmiral, Astrazeneca, Biogen, Genzyme, Merck and Novartis. L.A. has received lecture honoraria from Biogen and Teva.
Glossary
- Latitude gradient
-
A gradual decrease in incidence and prevalence of MS from north to south in the northern hemisphere, and in the opposite direction in the southern hemisphere.
- HLA complex
-
A region on human chromosome 6 containing ∼ 200 genes, most of which have functions in the immune system; of these, class II genes encode molecules that bind and present peptide antigens to CD4+ TH cells, and class I genes encode molecules that present peptide antigens to CD8+ cytotoxic T cells.
- Genome-wide association studies (GWAS)
-
Single-nucleotide polymorphisms (SNPs) are identified throughout the genome, usually several hundreds of thousands of SNPs, in very large case–control cohorts, allowing identification of associations between diseases and discrete genome loci.
- Experimental autoimmune encephalomyelitis
-
A model disease induced in experimental animals, commonly mice or rats, by immunizing the animal with CNS components that induce an autoimmune attack against the CNS that mimics many aspects of MS; can also be induced by transfer of CNS autoreactive T cells.
- Molecular mimicry
-
A phenomenon in which parts of a microbial agent have a molecular structure similar to a host molecule, thereby eliciting an immune response that is autoreactive against the host.
- Mendelian randomization
-
A method to determine causal effects of modifiable factors that takes advantage of the fact that gene variants for certain traits are independently segregated and randomly assigned at meiosis, thereby minimizing bias such as confounding.
- Epiphysioectomy
-
Surgical removal of the epiphysis (also known as the pineal gland), the main source of melatonin.
Rights and permissions
About this article
Cite this article
Olsson, T., Barcellos, L. & Alfredsson, L. Interactions between genetic, lifestyle and environmental risk factors for multiple sclerosis. Nat Rev Neurol 13, 25–36 (2017). https://doi.org/10.1038/nrneurol.2016.187
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneurol.2016.187
This article is cited by
-
Time trends in herpesvirus seroepidemiology among Swedish adults
BMC Infectious Diseases (2024)
-
Ancient DNA reveals evolutionary origins of autoimmune diseases
Nature Reviews Immunology (2024)
-
Childhood and adolescence factors and multiple sclerosis: results from the German National Cohort (NAKO)
BMC Neurology (2024)
-
Modifiable risk factors for multiple sclerosis have consistent directions of effect across diverse ethnic backgrounds: a nested case–control study in an English population-based cohort
Journal of Neurology (2024)
-
Demyelinating plaque-associated uveitis
Graefe's Archive for Clinical and Experimental Ophthalmology (2024)