Key Points
-
Hepatitis E virus (HEV) is the commonest cause of acute viral hepatitis worldwide
-
HEV is hyperendemic in many developing countries, where it is spread predominantly by contaminated water, and endemic in developed countries, where it is mostly a porcine zoonosis
-
HEV is associated with a range of subacute monophasic neurological injuries, in particular, Guillain–Barré syndrome, neuralgic amyotrophy and encephalitis/myelitis
-
In patients with HEV-associated neurological injury, the neurological features dominate the clinical picture, and hepatitis is either mild or absent
-
The incidence, clinical phenotype, pathophysiology and treatment of HEV-associated neurological injury remain to be determined
Abstract
Hepatitis E is hyperendemic in many developing countries in Asia and Africa, and is caused by hepatitis E virus (HEV) genotypes 1 and 2, which are spread via the faecal–oral route by contaminated water. Recent data show that HEV infection is also endemic in developed countries. In such geographical settings, hepatitis E is caused by HEV genotypes 3 and 4, and is mainly a porcine zoonosis. In a minority of cases, HEV causes acute and chronic hepatitis, but infection is commonly asymptomatic or unrecognized. HEV infection is associated with a number of extrahepatic manifestations, including a range of neurological injuries. To date, 91 cases of HEV-associated neurological injury — most commonly, Guillain–Barré syndrome, neuralgic amyotrophy, and encephalitis/myelitis — have been reported. Here, we review the reported cases, discuss possible pathogenic mechanisms, and present our perspectives on future directions and research questions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Kamar, N. et al. Hepatitis E. Lancet 379, 2477–2488 (2012).
Dalton, H. R., Bendall, R., Ijaz, S. & Banks, M. Hepatitis E: an emerging infection in developed countries. Lancet Infect. Dis. 8, 698–709 (2008).
Kamar, N., Dalton, H. R., Abravanel, F. & Izopet, J. Hepatitis E virus infection. Clin. Microbiol. Rev. 27, 116–138 (2014).
Woolson, K. L. et al. Extra-hepatic manifestations of autochthonous hepatitis E infection. Aliment. Pharmacol. Ther. 40, 1282–1291 (2014).
Dalton, H. R. et al. Autochthonous hepatitis E in Southwest England: natural history, complications and seasonal variation, and hepatitis E virus IgG seroprevalence in blood donors, the elderly and patients with chronic liver disease. Eur. J. Gastroenterol. Hepatol. 20, 784–790 (2008).
Dalton, H. R. et al. Autochthonous hepatitis E in southwest England. J. Viral Hepat. 14, 304–309 (2007).
Ijaz, S. et al. Non-travel-associated hepatitis E in England and Wales: demographic, clinical, and molecular epidemiological characteristics. J. Infect. Dis. 192, 1166–1172 (2005).
Mansuy, J. M. et al. Hepatitis E in the south west of France in individuals who have never visited an endemic area. J. Med. Virol. 74, 419–424 (2004).
Tsang, T. H. et al. Acute hepatitis E infection acquired in California. Clin. Infect. Dis. 30, 618–619 (2000).
Pina, S., Buti, M., Cotrina, M., Piella, J. & Girones, R. HEV identified in serum from humans with acute hepatitis and in sewage of animal origin in Spain. J. Hepatol. 33, 826–833 (2000).
Sainokami, S. et al. Epidemiological and clinical study of sporadic acute hepatitis E caused by indigenous strains of hepatitis E virus in Japan compared with acute hepatitis A. J. Gastroenterol. 39, 640–648 (2004).
Widdowson, M. A. et al. Cluster of cases of acute hepatitis associated with hepatitis E virus infection acquired in the Netherlands. Clin. Infect. Dis. 36, 29–33 (2003).
Kamar, N. et al. Hepatitis E virus and chronic hepatitis in organ-transplant recipients. N. Engl. J. Med. 358, 811–817 (2008).
Gerolami, R., Moal, V. & Colson, P. Chronic hepatitis E with cirrhosis in a kidney-transplant recipient. N. Engl. J. Med. 358, 859–860 (2008).
Kamar, N. et al. Factors associated with chronic hepatitis in patients with hepatitis E virus infection who have received solid organ transplants. Gastroenterology 140, 1481–1489 (2011).
Dalton, H. R., Bendall, R., Keane, F., Tedder, R. & Ijaz, S. Persistent carriage of hepatitis E virus in patients with HIV infection. N. Engl. J. Med. 361, 1025–1027 (2009).
Zaaijer, H. L. No artifact, hepatitis E is emerging. Hepatology 62, 654 (2014).
Slot, E. et al. Silent hepatitis E virus infection in Dutch blood donors, 2011 to 2012. Euro Surveill. 18, 20550 (2013).
Gallian, P. et al. Hepatitis E virus infections in blood donors, France. Emerg. Infect. Dis. 20, 1914–1917 (2014).
Mansuy, J. M. et al. Hepatitis E virus antibody in blood donors, France. Emerg. Infect. Dis. 17, 2309–2312 (2011).
Vollmer, T. et al. Novel approach for detection of hepatitis E virus infection in German blood donors. J. Clin. Microbiol. 50, 2708–2713 (2012).
Baylis, S. A., Gartner, T., Nick, S., Ovemyr, J. & Blumel, J. Occurrence of hepatitis E virus RNA in plasma donations from Sweden, Germany and the United States. Vox Sang. 103, 89–90 (2012).
Wenzel, J. J., Preiss, J., Schemmerer, M., Huber, B. & Jilg, W. Test performance characteristics of anti-HEV IgG assays strongly influence hepatitis E seroprevalence estimates. J. Infect. Dis. 207, 497–500 (2013).
Fukuda, S. et al. Prevalence of antibodies to hepatitis E virus among Japanese blood donors: identification of three blood donors infected with a genotype 3 hepatitis E virus. J. Med. Virol. 73, 554–561 (2004).
Guo, Q. S. et al. Prevalence of hepatitis E virus in Chinese blood donors. J. Clin. Microbiol. 48, 317–318 (2010).
Hewitt, P. E. et al. Hepatitis E virus in blood components: a prevalence and transmission study in southeast England. Lancet 384, 1766–1773 (2014).
Ijaz, S., Szypulska, R., Tettmar, K. I., Kitchen, A. & Tedder, R. S. Detection of hepatitis E virus RNA in plasma mini-pools from blood donors in England. Vox Sang. 102, 272 (2012).
Beale, M. A., Tettmar, K., Szypulska, R., Tedder, R. S. & Ijaz, S. Is there evidence of recent hepatitis E virus infection in English and North Welsh blood donors? Vox Sang. 100, 340–342 (2011).
Fischer, C. et al. Seroprevalence and incidence of hepatitis E in blood donors in Upper Austria. PLoS ONE 10, e0119576 (2015).
Xu, C. et al. An assessment of hepatitis E virus (HEV) in US blood donors and recipients: no detectable HEV RNA in 1939 donors tested and no evidence for HEV transmission to 362 prospectively followed recipients. Transfusion 53, 2505–2511 (2013).
Cleland, A. et al. Hepatitis E virus in Scottish blood donors. Vox Sang. 105, 283–289 (2013).
Shrestha, A. C. et al. Hepatitis E virus and implications for blood supply safety, Australia. Emerg. Infect. Dis. 20, 1940–1942 (2014).
Dalton, H. R. et al. Hepatitis E in New Zealand. J. Gastroenterol. Hepatol. 22, 1236–1240 (2007).
Halliday, J. S. et al. Hepatitis E virus infection, Papua New Guinea, Fiji, and Kiribati, 2003–2005. Emerg. Infect. Dis. 20, 1057–1058 (2014).
Faramawi, M. F., Johnson, E., Chen, S. & Pannala, P. R. The incidence of hepatitis E virus infection in the general population of the USA. Epidemiol. Infect. 139, 1145–1150 (2011).
Legrand-Abravanel, F. et al. Characteristics of autochthonous hepatitis E virus infection in solid-organ transplant recipients in France. J. Infect. Dis. 202, 835–844 (2010).
Sood, A., Midha, V. & Sood, N. Guillain–Barré syndrome with acute hepatitis E. Am. J. Gastroenterol. 95, 3667–3668 (2000).
Kejariwal, D., Roy, S. & Sarkar, N. Seizure associated with acute hepatitis E. Neurology 57, 1935 (2001).
Kamani, P. et al. Guillain–Barré syndrome associated with acute hepatitis E. Indian J. Gastroenterol. 24, 216 (2005).
Dixit, V. K., Abhilash, V. B., Kate, M. P. & Jain, A. K. Hepatitis E infection with Bell's palsy. J. Assoc. Physicians India 54, 418 (2006).
Mandal, K. & Chopra, N. Acute transverse myelitis following hepatitis E virus infection. Indian Pediatr. 43, 365–366 (2006).
Joshi, G. G. et al. Acute viral hepatitis E and Japanese encephalitis: an unusual co-occurrence. Indian J. Gastroenterol. 26, 102–103 (2007).
Fong, F. & Illahi, M. Neuralgic amyotrophy associated with hepatitis E virus. Clin. Neurol. Neurosurg. 111, 193–195 (2009).
Loly, J. P. et al. Guillain–Barré syndrome following hepatitis E. World J. Gastroenterol. 15, 1645–1647 (2009).
Rianthavorn, P. et al. The entire genome sequence of hepatitis E virus genotype 3 isolated from a patient with neuralgic amyotrophy. Scand. J. Infect. Dis. 42, 395–400 (2010).
Kamar, N. et al. Hepatitis E virus and neurologic disorders. Emerg. Infect. Dis. 17, 173–179 (2011).
Kamar, N. et al. Hepatitis E virus-induced neurological symptoms in a kidney-transplant patient with chronic hepatitis. Am. J. Transplant. 10, 1321–1324 (2010).
Dalton, H., Keane, F., Bendall, R., Mathew, J. & Ijaz, S. Treatment of chronic hepatitis E in a HIV positive patient. Ann. Intern. Med. 155, 479–480 (2011).
Cronin, S., McNicholas, R., Kavanagh, E., Reid, V. & O'Rourke, K. Anti-glycolipid GM2-positive Guillain–Barré syndrome due to hepatitis E infection. Ir. J. Med. Sci. 180, 255–257 (2011).
Maurissen, I., Jeurissen, A., Strauven, T., Sprengers, D. & De Schepper, B. First case of anti-ganglioside GM1-positive Guillain–Barré syndrome due to hepatitis E virus infection. Infection 40, 323–326 (2012).
Despierres, L. A. et al. Neurologic disorders and hepatitis E, France, 2010. Emerg. Infect. Dis. 17, 1510–1512 (2011).
Del Bello, A., Arne-Bes, M. C., Lavayssiere, L. & Kamar, N. Hepatitis E virus-induced severe myositis. J. Hepatol. 57, 1152–1153 (2012).
Tse, A. C., Cheung, R. T., Ho, S. L. & Chan, K. H. Guillain–Barré syndrome associated with acute hepatitis E infection. J. Clin. Neurosci. 19, 607–608 (2012).
Inghilleri, M. L., Grini Mazouzi, M. & Juntas Morales, R. Neuralgic amyotrophy as a manifestation of hepatitis E infection. Rev. Neurol. (Paris) 168, 383–384 (in French) (2012).
Sharma, B., Nagpal, K., Bakki Sannegowda, R. & Prakash, S. Hepatitis E with Gullain–Barré syndrome: still a rare association. J. Neurovirol. 19, 186–187 (2013).
Santos, L. et al. Acute hepatitis E complicated by Guillain–Barré syndrome in Portugal, December 2012 — a case report. Euro Surveill. 18, 20563 (2013).
Motte, A., Franques, J., Weitten, T. & Colson, P. Hepatitis E-associated Parsonage–Turner syndrome, France. Clin. Res. Hepatol. Gastroenterol. 38, e11–e14 (2014).
Moisset, X. et al. Severe bilateral amyotrophic neuralgia associated with major dysphagia secondary to acute hepatitis E. F1000Res. 2, 259 (2013).
Maddukuri, V. C. et al. Chronic hepatitis E with neurologic manifestations and rapid progression of liver fibrosis in a liver transplant recipient. Dig. Dis. Sci. 58, 2413–2416 (2013).
Geurtsvankessel, C. H. et al. Hepatitis E and Guillain–Barré syndrome. Clin. Infect. Dis. 57, 1369–1370 (2013).
de Vries, M. A., Samijn, J. P., de Man, R. & Boots, J. M. Hepatitis E-associated encephalopathy in a renal transplant recipient. BMJ Case Rep. http://dx.doi.org/10.1136/bcr-2014-204244 (2014).
Comont, T. et al. Acute hepatitis E infection associated with Guillain–Barré syndrome in an immunocompetent patient. Rev. Med. Interne 35, 333–336 (in French) (2014).
Scharn, N. et al. Guillain–Barré syndrome associated with autochthonous infection by hepatitis E virus subgenotype 3c. Infection 42, 171–173 (2014).
Deroux, A. et al. Association between hepatitis E and neurological disorders: two case studies and literature review. J. Clin. Virol. 60, 60–62 (2014).
Belbezier, A., Deroux, A., Sarrot-Reynauld, F., Larrat, S. & Bouillet, L. Myasthenia gravis associated with acute hepatitis E infection in immunocompetent woman. Emerg. Infect. Dis. 20, 908–910 (2014).
Chen, X. D., Zhou, Y. T., Zhou, J. J., Wang, Y. W. & Tong, D. M. Guillain–Barré syndrome and encephalitis/encephalopathy of a rare case of Northern China acute severe hepatitis E infection. Neurol. Sci. 35, 1461–1463 (2014).
van den Berg, B. et al. Guillain–Barré syndrome associated with preceding hepatitis E virus infection. Neurology 82, 491–497 (2014).
van Eijk, J. J. et al. Neuralgic amyotrophy and hepatitis E virus infection. Neurology 82, 498–503 (2014).
Bennett, S., Gunson, R. N. & Li, K. Hepatitis E virus infection presenting with paraesthesia. Scott. Med. J. 60, e27–e29 (2015).
Blasco Perrin, H. et al. Neurologic disorders in non-immunocompromized patients with auotchtonous acute hepatitis E. Emerg. Infect. Dis. 21, 1928–1934 (2015).
Décard, B. F. et al. Hepatitis-E virus associated neuralgic amyotrophy with sustained plexus brachialis swelling visualized by high-resolution ultrasound. J. Neurol. Sci. 351, 208–210 (2015).
Theochari, E., Vincent-Smith, L. & Ellis, C. Neuralgic amyotrophy complicating acute hepatitis E infection: a rare association. BMJ Case Rep. http://dx.doi.org/10.1136/bcr-2014-207669 (2015).
Jha, A. K., Nijhawan, S., Nepalia, S. & Suchismita, A. Association of Bell's palsy with hepatitis E virus infection: a rare entity. J. Clin. Exp. Hepatol. 2, 88–90 (2012).
Carli, P. et al. Shoulder pain in a 30-year-old man. Rev. Med. Interne 33, 111–114 (in French) (2012).
Cheung, M. C., Maguire, J., Carey, I., Wendon, J. & Agarwal, K. Hepatitis E — an unexpected problem at home. Scand. J. Gastroenterol. 47, 253 (2012).
Peri, A. M., Milazzo, L., Meroni, L. & Antinori, S. Radiculoneuropathy associated with acute hepatitis E. Dig. Liver Dis. 45, 963–964 (2013).
Martínez Rodríguez, L., Carvajal, P. & Morís, G. Neuralgic amyotrophy associated to hepatitis E virus infection. Med. Clin. (Barc.) 145, 462–463 (in Spanish) (2015).
Dartevel, A. et al. Hepatitis E and neuralgic amyotrophy: five cases and review of literature. J. Clin. Virol. 69, 156–164 (2015).
Fokke, C. et al. Diagnosis of Guillain–Barré syndrome and validation of Brighton criteria. Brain 137, 33–43 (2014).
Jacobs, B. C. et al. The spectrum of antecedent infections in Guillain–Barré syndrome: a case–control study. Neurology 51, 1110–1115 (1998).
Oomes, P. G., van der Meche, F. G. & Kleyweg, R. P. Liver function disturbances in Guillain–Barré syndrome: a prospective longitudinal study in 100 patients. Dutch Guillain–Barré Study Group. Neurology 46, 96–100 (1996).
van Alfen, N. Clinical and pathophysiological concepts of neuralgic amyotrophy. Nat. Rev. Neurol. 7, 315–322 (2011).
van Alfen, N. & van Engelen, B. G. The clinical spectrum of neuralgic amyotrophy in 246 cases. Brain 129, 438–450 (2006).
Yazaki, Y. et al. Characteristics of 20 patients with autochthonous acute hepatitis E in Hokkaido, Japan: first report of bilateral facial palsy following the infection with genotype 4 hepatitis E virus. Tohoku J. Exp. Med. 236, 263–271 (2015).
Legrand-Abravanel, F. et al. Hepatitis E virus genotype 3 diversity, France. Emerg. Infect. Dis. 15, 110–114 (2009).
Nemni, R. et al. Peripheral neuropathy in hepatitis C virus infection with and without cryoglobulinaemia. J. Neurol. Neurosurg. Psychiatry 74, 1267–1271 (2003).
Authier, F. J. et al. Detection of genomic viral RNA in nerve and muscle of patients with HCV neuropathy. Neurology 60, 808–812 (2003).
Cacoub, P., Saadoun, D., Limal, N., Leger, J. M. & Maisonobe, T. Hepatitis C virus infection and mixed cryoglobulinaemia vasculitis: a review of neurological complications. AIDS 19, S128–S134 (2005).
Shukla, P. et al. Adaptation of a genotype 3 hepatitis E virus to efficient growth in cell culture depends on an inserted human gene segment acquired by recombination. J. Virol. 86, 5697–5707 (2012).
Yuki, N. et al. Carbohydrate mimicry between human ganglioside GM1 and Campylobacter jejuni lipooligosaccharide causes Guillain–Barré syndrome. Proc. Natl Acad. Sci. USA 101, 11404–11409 (2004).
Plomp, J. J. & Willison, H. J. Pathophysiological actions of neuropathy-related anti-ganglioside antibodies at the neuromuscular junction. J. Physiol. 587, 3979–3999 (2009).
van Alfen, N. et al. Incidence of neuralgic amyotrophy (Parsonage Turner syndrome) in a primary care seting — a prospective cohort study. PLoS ONE 10, e0128361 (2015).
Bendall, R., Ellis, V., Ijaz, S., Ali, R. & Dalton, H. A comparison of two commercially available anti-HEV IgG kits and a re-evaluation of anti-HEV IgG seroprevalence data in developed countries. J. Med. Virol. 82, 799–805 (2010).
French Cooperative Group on Plasma Exchange in Guillain–Barré syndrome. Efficiency of plasma exchange in Guillain–Barré syndrome: role of replacement fluids. Ann. Neurol. 22, 753–761 (1987).
Hughes, R. A. & Cornblath, D. R. Guillain–Barré syndrome. Lancet 366, 1653–1666 (2005).
van Eijk, J. J. et al. Evaluation of prednisolone treatment in the acute phase of neuralgic amyotrophy: an observational study. J. Neurol. Neurosurg. Psychiatry 80, 1120–1124 (2009).
van Alfen, N., van Engelen, B. G. & Hughes, R. A. Treatment for idiopathic and hereditary neuralgic amyotrophy (brachial neuritis). Cochrane Database Syst. Rev. 3, CD006976 (2009).
Fourquet, E. et al. Severe thrombocytopenia associated with acute autochthonous hepatitis E. J. Clin. Virol. 48, 73–74 (2010).
Pischke, S., Behrendt, P., Manns, M. P. & Wedemeyer, H. HEV-associated cryoglobulinaemia and extrahepatic manifestations of hepatitis E. Lancet Infect. Dis. 14, 678–679 (2014).
Kamar, N. et al. Hepatitis E virus and the kidney in solid-organ-transplant patients. Transplantation 93, 617–623 (2012).
Deniel, C. et al. Acute pancreatitis: a rare complication of acute hepatitis E. J. Clin. Virol. 51, 202–204 (2011).
Serratrice, J. et al. Acute polyarthritis revealing hepatitis E. Clin. Rheumatol. 26, 1973–1975 (2007).
Dumoulin, F. L. & Liese, H. Acute hepatitis E virus infection and autoimmune thyroiditis: yet another trigger? BMJ Case Rep. http://dx.doi.org/10.1136/bcr.12.2011.5441 (2012).
Hoofnagle, J. H., Nelson, K. & Purcell, R. H. Hepatitis E. N. Engl. J. Med. 367, 1237–1244 (2012).
Rein, D. B., Stevens, G. A., Theaker, J., Wittenborn, J. S. & Wiersma, S. T. The global burden of hepatitis E virus genotypes 1 and 2 in 2005. Hepatology 55, 988–997 (2012).
Stramer, S. L. et al. Hepatitis E virus: seroprevalence and frequency of viral RNA detection among US blood donors. Transfusion http://dx.doi.org/10.1111/trf.13355 (2015).
Acknowledgements
H.R.D. and N.K. have received support from the Gates Foundation. B.C.J. has received support from the Netherlands Organization for Health Research and Development, Erasmus MC and GBS-CIDP Foundation International.
Author information
Authors and Affiliations
Contributions
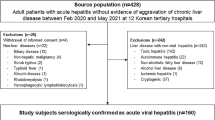
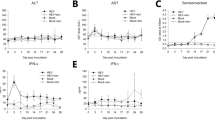
H.R.D., N.K., J.J.J.v.E., R.P.B., P.C., B.N.M., and B.C.J. researched data for the article, made substantial contributions to discussion of the content, wrote the article, and reviewed and/or edited the manuscript before submission. H.R.D. drafted the tables. N.K. drafted the supplementary table, and J.J.J.v.E. drafted the figures.
Corresponding author
Ethics declarations
Competing interests
H.R.D. has received travel and accommodation costs and consultancy fees from GlaxoSmithKline, Wantai and Roche; travel, accommodation and lecture fees from Merck, Gilead and GFE Blut; and travel and accommodation fees from the Falk Foundation. N.K. has received travel and accommodation costs and consultancy fees from Novartis and Merck; travel, accommodation and lecture fees from Gilead, Novartis, Astellas, BMS, Amgen and Fresenius. J.J.J.v.E. has received travel and accommodation costs or consultancy or lecture fees from Merck, Biogen Idec, Novartis and Teva Pharmaceutical Industries. B.C.J. has received research support from Prinses Beatrix Spierfonds, CSL-Behring and Grifols, and travel support from Baxter Biopharmaceutics. The other authors declare no competing interests.
Supplementary information
Supplementary Table 1
Review – neurological manifestations associated with HEV (DOCX 71 kb)
Rights and permissions
About this article
Cite this article
Dalton, H., Kamar, N., van Eijk, J. et al. Hepatitis E virus and neurological injury. Nat Rev Neurol 12, 77–85 (2016). https://doi.org/10.1038/nrneurol.2015.234
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneurol.2015.234
This article is cited by
-
Hepatitis E virus and Klebsiella pneumoniae co-infection detected by metagenomics next-generation sequencing in a patient with central nervous system and bloodstream Infection: a case report
BMC Infectious Diseases (2024)
-
Massivste epigastrische Schmerzen bei einem 59-jährigen Patienten
Der Internist (2021)
-
Why all blood donations should be tested for hepatitis E virus (HEV)
BMC Infectious Diseases (2019)
-
Human Schwann cells are susceptible to infection with Zika and yellow fever viruses, but not dengue virus
Scientific Reports (2019)
-
Pathogenic mechanisms and current epidemiological status of HEV infection in asymptomatic blood donors and patients with chronic diseases
European Journal of Clinical Microbiology & Infectious Diseases (2019)