Key Points
-
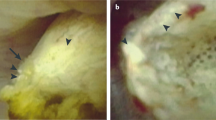
Idiopathic calcium stones are always accompanied by mineral deposits: interstitial deposits of apatite in patients with calcium oxalate (CaOx) stones or calcium phosphate (CaP) plugs in those with CaP stones
-
Overgrowth of CaOx stones on plaque depends on the formation of an initial CaP phase; urine saturations of CaP and CaOx might, therefore, be equally important
-
Microliths form on the open ends of tubule plugs but proof that these microliths can grow into clinically relevant stones is lacking
-
Patients with tubule plugs who form CaP stones show varying degrees of cortical fibrosis and nephron loss
-
Trial data support the use of high fluid intake, potassium citrate, thiazide diuretic agents and a reduced sodium diet for prevention of recurrent calcium renal stones
-
As idiopathic hypercalciuria arises from reduced renal tubule calcium reabsorption and is associated with negative calcium balance and bone disease, management with a low calcium diet is contraindicated
Abstract
The most common presentation of nephrolithiasis is idiopathic calcium stones in patients without systemic disease. Most stones are primarily composed of calcium oxalate and form on a base of interstitial apatite deposits, known as Randall's plaque. By contrast some stones are composed largely of calcium phosphate, as either hydroxyapatite or brushite (calcium monohydrogen phosphate), and are usually accompanied by deposits of calcium phosphate in the Bellini ducts. These deposits result in local tissue damage and might serve as a site of mineral overgrowth. Stone formation is driven by supersaturation of urine with calcium oxalate and brushite. The level of supersaturation is related to fluid intake as well as to the levels of urinary citrate and calcium. Risk of stone formation is increased when urine citrate excretion is <400 mg per day, and treatment with potassium citrate has been used to prevent stones. Urine calcium levels >200 mg per day also increase stone risk and often result in negative calcium balance. Reduced renal calcium reabsorption has a role in idiopathic hypercalciuria. Low sodium diets and thiazide-type diuretics lower urine calcium levels and potentially reduce the risk of stone recurrence and bone disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Scales, C. D. Jr., Smith, A. C., Hanley, J. M. & Saigal, C. S. Prevalence of kidney stones in the United States. Eur. Urol. 62, 160–165 (2012).
Kirkali, Z., Rasooly, R., Star, R. A. & Rodgers, G. P. Urinary stone disease: progress, status, and needs. Urology 86, 651–653 (2015).
Worcester, E. M. & Coe, F. L. Nephrolithiasis. Prim. Care 35, 369–391 (2008).
Worcester, E. M. & Coe, F. L. New insights into the pathogenesis of idiopathic hypercalciuria. Semin. Nephrol. 28, 120–132 (2008).
Parks, J. H., Worcester, E. M., Coe, F. L., Evan, A. P. & Lingeman, J. E. Clinical implications of abundant calcium phosphate in routinely analyzed kidney stones. Kidney Int. 66, 777–785 (2004).
Evan, A. P. et al. Mechanisms of human kidney stone formation. Urolithiasis. 43 (Suppl. 1), 19–32 (2015).
Miller, N. L. et al. A formal test of the hypothesis that idiopathic calcium oxalate stones grow on Randall's plaque. BJU Int. 103, 966–971 (2009). This paper provides evidence for the importance of Randall's plaque as the site of attachment of idiopathic calcium oxalate stones.
Miller, N. L. et al. In idiopathic calcium oxalate stone-formers, unattached stones show evidence of having originated as attached stones on Randall's plaque. BJU Int. 105, 242–245 (2010).
Linnes, M. P. et al. Phenotypic characterization of kidney stone formers by endoscopic and histological quantification of intrarenal calcification. Kidney Int. 84, 818–825 (2013).
Wang, X. et al. Distinguishing characteristics of idiopathic calcium oxalate kidney stone formers with low amounts of Randall's plaque. Clin. J. Am. Soc. Nephrol. 9, 1757–1763 (2014).
Viers, B. R. et al. Endoscopic and histologic findings in a cohort of uric acid and calcium oxalate stone formers. Urology 85, 771–776 (2015).
Letavernier, E. et al. Demographics and characterization of 10,282 Randall plaque-related kidney stones: a new epidemic? Medicine (Baltimore) 94, e566 (2015).
Evan, A. E. et al. Histopathology and surgical anatomy of patients with primary hyperparathyroidism and calcium phosphate stones. Kidney Int. 74, 223–229 (2008).
Evan, A. P. et al. Intra-tubular deposits, urine and stone composition are divergent in patients with ileostomy. Kidney Int. 76, 1081–1088 (2009).
Evan, A. P. et al. Renal histopathology and crystal deposits in patients with small bowel resection and calcium oxalate stone disease. Kidney Int. 78, 310–317 (2010).
Evan, A. P. et al. Contrasting histopathology and crystal deposits in kidneys of idiopathic stone formers who produce hydroxy apatite, brushite, or calcium oxalate stones. Anat. Rec. (Hoboken) 297, 731–748 (2014).
Evan, A. P. et al. Crystal-associated nephropathy in patients with brushite nephrolithiasis. Kidney Int. 67, 576–591 (2005).
Coe, F. L., Evan, A. P., Lingeman, J. E. & Worcester, E. M. Plaque and deposits in nine human stone diseases. Urol. Res. 38, 239–247 (2010).
Evan, A. P. et al. Randall's plaque of patients with nephrolithiasis begins in basement membranes of thin loops of Henle. J. Clin. Invest. 111, 607–616 (2003). Initial description of the papillary anatomy of calcium stone formers and the earliest site of appearance of Randall's plaque.
Evan, A. P. et al. Apatite plaque particles in inner medulla of kidneys of calcium oxalate stone formers: osteopontin localization. Kidney Int. 68, 145–154 (2005).
Evan, A. P. et al. Renal inter-α-trypsin inhibitor heavy chain 3 increases in calcium oxalate stone-forming patients. Kidney Int. 72, 1503–1511 (2007).
Williams, J. C. et al. Micro-CT imaging of Randall's plaques. Urolithiasis 43 (Suppl. 1), 13–17 (2015).
Khan, S. R., Rodriguez, D. E., Gower, L. B. & Monga, M. Association of Randall plaque with collagen fibers and membrane vesicles. J. Urol. 187, 1094–1100 (2012).
Evan, A. P. et al. Biopsy proven medullary sponge kidney: clinical findings, histopathology, and role of osteogenesis in stone and plaque formation. Anat. Rec. (Hoboken) 298, 865–877 (2015).
Kuo, R. L. et al. Urine calcium and volume predict coverage of renal papilla by Randall's plaque. Kidney Int. 64, 2150–2154 (2003).
Kriz, W. & Kaissling, B. in Structural Organization of the Mammalian Kidney in Seldin and Giebisch's The Kidney: Physiology and Pathophysiology (eds Alpern, R. J. et al.) 595–691 (Elsevier, 2013).
Bernardo, J. F. & Friedman, P. A. in Renal calcium metabolism in Seldin and Giebisch's The Kidney: Physiology and Pathophysiology (eds Alpern, R. J. et al.) 2225–2247 (Academic Press, 2013).
Coe, F. L., Evan, A. & Worcester, E. Pathophysiology-based treatment of idiopathic calcium kidney stones. Clin. J. Am. Soc. Nephrol. 6, 2083–2092 (2011).
Stoller, M. L., Shami, G. S., McCormick, V. D. & Kerschmann, R. L. High resolution radiography of cadaveric kidneys: unraveling the mystery of Randall's plaque formation. J. Urol. 156, 1263–1266 (1996).
Alexander, R. T. et al. Kidney stones and cardiovascular events: a cohort study. Clin. J. Am. Soc. Nephrol. 9, 506–512 (2014).
Ferraro, P. M. et al. History of kidney stones and the risk of coronary heart disease. JAMA 310, 408–415 (2013).
Evan, A. P. et al. Comparison of the pathology of interstitial plaque in human ICSF stone patients to NHERF-1 and THP-null mice. Urol. Res. 38, 439–452 (2010).
Evan, A. P. et al. Mechanism of formation of human calcium oxalate renal stones on Randall's plaque. Anat. Rec. (Hoboken.) 290, 1315–1323 (2007). A description of the ultrastructure of the interface between plaque and the earliest phase of calcium oxalate stone formation.
Evan, A. P. et al. Renal intratubular crystals and hyaluronan staining occur in stone formers with bypass surgery but not with idiopathic calcium oxalate stones. Anat. Rec. (Hoboken.) 291, 325–334 (2008).
Evan, A. P. et al. Renal histopathology of stone-forming patients with distal renal tubular acidosis. Kidney Int. 71, 795–801 (2007).
Evan, A. P. et al. Renal crystal deposits and histopathology in patients with cystine stones. Kidney Int. 69, 2227–2235 (2006).
Worcester, E. M. et al. A test of the hypothesis that oxalate secretion produces proximal tubule crystallization in primary hyperoxaluria type I. Am. J. Physiol. Renal Physiol. 305, F1574–F1584 (2013).
Worcester, E. M., Parks, J. H., Evan, A. P. & Coe, F. L. Renal function in patients with nephrolithiasis. J. Urol. 176, 600–603 (2006).
Coe, F. L., Evan, A. P., Worcester, E. M. & Lingeman, J. E. Three pathways for human kidney stone formation. Urol. Res. 38, 147–160 (2010).
Rule, A. D., Krambeck, A. E. & Lieske, J. C. Chronic kidney disease in kidney stone formers. Clin. J. Am. Soc. Nephrol. 6, 2069–2075 (2011).
Coe, F. L. & Parks, J. H. in Physical Chemistry of Calcium Stone Disease in Nephrolithiasis: Pathogenesis and Treatment (eds Coe, F. L. & Parks, J. H.) 38–58 (Year Book Medical Publishers, 1988).
Qiu, S. R. & Orme, C. A. Dynamics of biomineral formation at the near-molecular level. Chem. Rev. 108, 4784–4822 (2008).
Finlayson, B. in Calcium stones: some physical and clinical aspects in Calcium metabolism in renal failure and nephrolithiasis (eds David, D. S.) 337–382 (John Wiley & Sons, 1977). A description of the method for computation of urinary supersaturation in stone formers.
Parks, J. H., Coward, W. M. & Coe, F. L. Correspondence between stone composition and urine supersaturation in nephrolithiasis. Kidney Int. 51, 894–900 (1997).
Bergsland, K. J., Zisman, A. L., Asplin, J. R., Worcester, E. M. & Coe, F. L. Evidence for net renal tubule oxalate secretion in patients with calcium kidney stones. Am. J. Physiol. Renal Physiol. 300, F311–F318 (2011).
Santucci, L. et al. Urinary proteome in a snapshot: normal urine and glomerulonephritis. J. Nephrol. 26, 610–616 (2013).
Wright, C. A. et al. Label-free quantitative proteomics reveals differentially regulated proteins influencing urolithiasis. Mol. Cell. Proteomics 10, M110 (2011).
Kumar, V. & Lieske, J. C. Protein regulation of intrarenal crystallization. Curr. Opin. Nephrol. Hypertens. 15, 374–380 (2006). A review of the role of urinary crystallization inhibitors in preventing kidney stones.
Aggarwal, K. P., Narula, S., Kakkar, M. & Tandon, C. Nephrolithiasis: molecular mechanism of renal stone formation and the critical role played by modulators. Biomed. Res. Int. 2013, 292953 (2013).
Canales, B. K. et al. Proteome of human calcium kidney stones. Urology 76, 1017–1020 (2010).
Pak, C. Y. C. Physicochemical basis for formation of renal stones of calcium phosphate origin: calculation of the degree of supersaturation of urine with respect to brushite. J. Clin. Invest. 48, 1914–1922 (1969). A fundamental explanation of urinary supersaturation with respect to calcium phosphate.
Nancollas, G. H. & Henneman, Z. J. Calcium oxalate: calcium phosphate transformations. Urol. Res. 38, 277–280 (2010).
Costa-Bauza, A. et al. Type of renal calculi: variation with age and sex. World J. Urol. 25, 415–421 (2007).
Joseph, N. R. The dissociation constants of organic calcium complexes. J. Biol. Chem. 164, 529–541 (1946).
Rodgers, A. L., Allie-Hamdulay, S., Jackson, G. E. & Sutton, R. A. Enteric hyperoxaluria secondary to small bowel resection: use of computer simulation to characterize urinary risk factors for stone formation and assess potential treatment protocols. J. Endourol. 28, 985–994 (2014).
De Yoreo, J. J., Qiu, S. R. & Hoyer, J. R. Molecular modulation of calcium oxalate crystallization. Am. J. Physiol. Renal Physiol. 291, F1123–F1131 (2006).
Coe, F. L., Parks, J. H. & Moore, E. S. Familial idiopathic hypercalciuria. N. Engl. J. Med. 300, 337–340 (1979).
Albright, F., Henneman, P., Benedict, P. H. & Forbes, A. P. Idiopathic hypercalciuria: a preliminary report. Proc. R. Soc. Med. 46, 1077–1081 (1953).
Heilberg, I. P. & Weisinger, J. R. Bone disease in idiopathic hypercalciuria. Curr. Opin. Nephrol. Hypertens. 15, 394–402 (2006). An excellent review of the nature of the bone disease in patients with idiopathic hypercalciuria.
Curhan, G. C. & Taylor, E. N. 24-h uric acid excretion and the risk of kidney stones. Kidney Int. 73, 489–496 (2008). A presentation of data from a large prospective observational study that sheds light on urinary risk factors for stone formation.
Blaine, J., Chonchol, M. & Levi, M. Renal control of calcium, phosphate, and magnesium homeostasis. Clin. J. Am. Soc. Nephrol. 10, 1257–1272 (2015).
Liberman, U. A. et al. Metabolic and calcium kinetic studies in idiopathic hypercalciuria. J. Clin. Invest. 47, 2580–2590 (1968).
Heaney, R. P. & Skillman, T. G. Secretion and excretion of calcium by the human gastrointestinal tract. J. Lab. Clin. Med. 64, 29–41 (1964).
Nassim, J. R. & Higgins, B. A. Control of idiopathic hypercalciuria. Br. Med. J. 1, 675–681 (1965).
Edwards, N. A. & Hodgekinson, A. Metabolic studies in patients with idiopathic hypercalciuria. Clin. Sci. 29, 143–157 (1965).
Henneman, P. H., Benedict, P. H., Forbes, A. P. & Dudley, H. R. Idiopathic hypercalciuria. N. Engl. J. Med. 259, 802–807 (1958).
Jackson, W. P. U. & Dancaster, C. A consideration of the hypercalciuria in sarcoidosis, idiopathic hypercalciuria, and that produced by vitamin D. A new suggestion regarding calcium metabolism. J. Clin. Endocrinol. Metab. 19, 658 (1959).
Harrison, A. R. Some results of metabolic investigations in cases of renal stone. Br. J. Urol. 31, 398 (1959).
Dent, C. E., Harper, C. M. & Parfitt, A. M. The effect of cellulose phosphate on calcium metabolism in patients with hypercalciuria. Clin. Sci. 27, 417–425 (1964).
Parfitt, A. M., Higgins, B. A., Nassim, J. R., Collins, J. A. & Hilb, A. Metabolic studies in patients with hypercalciuria. Clin. Sci. 27, 463–482 (1964).
Yendt, E. R., Gagne, R. J. A. & Cohanim, M. The effects of thiazides in idiopathic hypercalciuria. Trans. Am. Clin. Climatol. Assoc. 77, 96–110 (1966).
Dent, C. E. & Watson, L. Metabolic studies in a patient with idiopathic hypercalciuria. Br. Med. J. 2, 449–452 (1965).
Anderson, J., Lee, H. A. & Tomlinson, R. W. Some metabolic aspects of idiopathic hypercalciuria. Nephron 4, 129–138 (1967).
Khanal, R. C. & Nemere, I. Regulation of intestinal calcium transport. Annu. Rev. Nutr. 28, 179–196 (2008).
Insogna, K. L., Broadus, A. E., Dreyer, B. E., Ellison, A. F. & Gertner, J. M. Elevated production rate of 1,25-dihydroxyvitamin D in patients with absorptive hypercalciuria. J. Clin. Endocrinol. Metab. 61, 490–495 (1985).
Bushinsky, D. A., Frick, K. K. & Nehrke, K. Genetic hypercalciuric stone-forming rats. Curr. Opin. Nephrol. Hypertens. 15, 403–418 (2006).
Worcester, E. M. et al. Evidence that postprandial reduction of renal calcium reabsorption mediates hypercalciuria of patients with calcium nephrolithiasis. Am. J. Physiol. Renal Physiol. 292, F66–F75 (2007).
Worcester, E. M., Bergsland, K. J., Gillen, D. L. & Coe, F. L. Evidence for increased renal tubule and parathyroid gland sensitivity to serum calcium in human idiopathic hypercalciuria. Am. J. Physiol. Renal Physiol. 305, F853–F860 (2013).
Worcester, E. M. et al. Evidence for increased postprandial distal nephron calcium delivery in hypercalciuric stone-forming patients. Am. J. Physiol. Renal Physiol. 295, F1286–F1294 (2008). This paper provides evidence that proximal tubule sodium and calcium reabsorption is lower in patients with idiopathic hypercalciuria than in normal individuals, and that this difference contributes to elevated urine calcium excretion.
Coe, F. L. et al. Effects of low-calcium diet on urine calcium excretion, parathyroid function and serum 1,25(OH)2D3 levels in patients with idiopathic hypercalciuria and in normal subjects. Am. J. Med. 72, 25–32 (1982). An important study showing that altered renal calcium reabsorption is a key feature of idiopathic hypercalciuria.
Qaseem, A., Dallas, P., Forciea, M. A., Starkey, M. & Denberg, T. D. Dietary and pharmacologic management to prevent recurrent nephrolithiasis in adults: a clinical practice guideline from the American College of Physicians. Ann. Intern. Med. 161, 659–667 (2014).
Bergsland, K. J., Coe, F. L., Gillen, D. L. & Worcester, E. M. A test of the hypothesis that the collecting duct calcium-sensing receptor limits rise of urine calcium molarity in hypercalciuric calcium kidney stone formers. Am. J. Physiol. Renal Physiol. 297, F1017–F1023 (2009).
Pak, C. Y. C., Sakhaee, K., Crowther, C. & Brinkley, L. Evidence justifying a high fluid intake in treatment of nephrolithiaisis. Ann. Intern. Med. 93, 36–39 (1980).
Borghi, L. et al. Urinary volume, water and recurrences of idiopathic calcium nephrolithiasis: a 5-year randomized prospective study. J. Urol. 155, 839–843 (1996). Evidence for the importance of fluid intake as a way to prevent recurrence of calcium stones.
Breslau, N. A., Mcguire, J. L., Zerwekh, J. E. & Pak, C. Y. C. The role of dietary sodium on renal excretion and intstinal absorption of calicum and on vitamin D metabolism. J. Clin. Endocrinol. Metab. 55, 369–373 (1982).
Sakhaee, K., Harvey, J. A., Padalino, P., Whitson, P. & Pak, C. Y. C. The potential role of salt abuse on the risk for kidney stone formation. J. Urol. 150, 310–312 (1993).
McCarron, D. A. et al. Urinary calcium excretion at extremes of sodium intake in normal man. Am. J. Nephrol. 1, 84–90 (1981).
Phillips, M. J. & Cooke, J. N. C. Relation between urinary calcium and sodium in patients with idiopathic hypercalciuria. Lancet 1, 1354–1357 (1967).
Teucher, B. et al. Sodium and bone health: impact of moderately high and low salt intakes on calcium metabolism in postmenopausal women. J. Bone Miner. Res. 23, 1477–1485 (2008).
McParland, B. E., Goulding, A. & Campbell, A. J. Dietary salt affects biochemical markers of resorption and formation of bone in elderly women. BMJ 299, 834–835 (1989).
Frings-Meuthen, P., Baecker, N. & Heer, M. Low-grade metabolic acidosis may be the cause of sodium chloride-induced exaggerated bone resorption. J. Bone Miner. Res. 23, 517–524 (2008).
Nascimento, L., Oliveros, F. H. & Cunningham, E. Renal handling of sodium and calcium in hypercalciuria. Clin. Pharmacol. Ther. 35, 342–347 (1984).
Pak, C. Y. et al. Effect of dietary modification on urinary stone risk factors. Kidney Int. 68, 2264–2273 (2005).
Muldowney, F. P., Freaney, R. & K.Moloney, M. F. Importance of dietary sodium in the hypercalciuria syndrome. Kidney Int. 22, 292–296 (1982).
Silver, J., Rubinger, D., Friedlaender, M. M. & Popovtzer, M. M. Sodium-dependent idiopathic hypercalciuria in renal-stone formers. Lancet 2, 484–486 (1983).
Nouvenne, A. et al. Diet to reduce mild hyperoxaluria in patients with idiopathic calcium oxalate stone formation: a pilot study. Urology 73, 725–730. e1 (2009).
Nouvenne, A. et al. Effects of a low-salt diet on idiopathic hypercalciuria in calcium-oxalate stone formers: a 3-mo randomized controlled trial. Am. J. Clin. Nutr. 91, 565–570 (2010).
Burtis, W. J., Gay, L., Insogna, K. L., Ellison, A. & Broadus, A. E. Dietary hypercalciuria in patients with calcium oxalate kidney stones. Am. J. Clin. Nutr. 60, 424–429 (1994).
Blackwood, A. M., Sagnella, G. A., Cook, D. G. & Cappuccio, F. P. Urinary calcium excretion, sodium intake and blood pressure in a multi-ethnic population: results of the Wandsworth Heart and Stroke Study. J. Hum. Hypertens. 15, 229–237 (2001).
Taylor, E. N. & Curhan, G. C. Demographic, dietary, and urinary factors and 24-h urinary calcium excretion. Clin. J. Am. Soc. Nephrol. 4, 1980–1987 (2009).
Damasio, P. C. et al. The role of salt abuse on risk for hypercalciuria. Nutr. J. 10, 3 (2011).
Borghi, L. et al. Comparison of two diets for the prevention of recurrent stones in idiopathic hypercalciuria. N. Engl. J. Med. 346, 77–84 (2002). This study documents the efficacy of a low sodium, normal calcium, moderately low protein diet to prevent recurrent calcium oxalate stones.
U.S. Department of Agriculture & U.S. Department of Health and Human Services. Dietary Guidelines for Americans (U.S. Government Printing Office, 2010).
Yendt, E. R., Gagne, R. J. A. & Cohanim, M. The effects of thiazides in idiopathic hypercalciuria. Am. J. Med. Sci. 261, 449–460 (1966).
Fink, H. A. et al. Medical management to prevent recurrent nephrolithiasis in adults: a systematic review for an American College of Physicians Clinical Guideline. Ann. Intern. Med. 158, 535–543 (2013).
Laerum, E. & Larsen, S. Thiazide prophylaxis of urolithiasis: a double-blind study in general practice. Acta Med. Scand. 215, 383–389 (1984).
Ettinger, B., Citron, J. T., Livermore, B. & Dolman, L. I. Chlorthalidone reduces calcium oxalate calculous recurrence but magnesium hydroxide does not. J. Urol. 139, 679–684 (1988).
Borghi, L., Meschi, T., Guerra, A. & Novarini, A. Randomized prospective study of a nonthiazide diuretic, indapamide, in preventing calcium stone recurrences. J. Cardiovasc. Pharmacol. 22, S78–S86 (1993).
Bergsland, K. J., Worcester, E. M. & Coe, F. L. Role of proximal tubule in the hypocalciuric response to thiazide of patients with idiopathic hypercalciuria. Am. J. Physiol. Renal Physiol. 305, F592–F599 (2013).
Coe, F. L., Parks, J. H., Bushinsky, D. A., Langman, C. B. & Favus, M. J. Chlorthalidone promotes mineral retention in patients with idiopathic hypercalciuria. Kidney Int. 33, 1140–1146 (1988).
Bolland, M. J. et al. The effect of treatment with a thiazide diuretic for 4 years on bone density in normal postmenopausal women. Osteoporos. Int. 18, 479–486 (2007).
Aung, K. & Htay, T. Thiazide diuretics and the risk of hip fracture. Cochrane Database Syst. Rev. 10, CD005185 (2011).
Caudarella, R., Vescini, F., Buffa, A. & Stefoni, S. Citrate and mineral metabolism: kidney stones and bone disease. Front. Biosci. 8, s1084–s1106 (2003).
Curthoys, N. P. & Moe, O. W. Proximal tubule function and response to acidosis. Clin. J. Am. Soc. Nephrol. 9, 1627–1638 (2014).
Halperin, M. L., Cheema, D. S. & Kamel, K. S. Physiology of acid-base balance: links with kidney stone prevention. Semin. Nephrol. 26, 441–446 (2006).
Pinheiro, V. B., Baxmann, A. C., Tiselius, H. G. & Heilberg, I. P. The effect of sodium bicarbonate upon urinary citrate excretion in calcium stone formers. Urology 82, 33–37 (2013).
Moseley, K. F., Weaver, C. M., Appel, L., Sebastian, A. & Sellmeyer, D. E. Potassium citrate supplementation results in sustained improvement in calcium balance in older men and women. J. Bone Miner. Res. 28, 497–504 (2013).
Menegon, L. F., Figueiredo, J. F. & Gontijo, J. A. Effect of metabolic acidosis on renal tubular sodium handling in rats as determined by lithium clearance. Braz. J. Med. Biol. Res. 31, 1269–1273 (1998).
Safirstein, R., Glassman, V. P. & DiScala, V. A. Effects of an NH4Cl-induced metabolic acidosis on salt and water reabsorption in dog kidney. Am. J. Physiol. 225, 805–809 (1973).
Wang, T., Egbert, A. L. Jr., Aronson, P. S. & Giebisch, G. Effect of metabolic acidosis on NaCl transport in the proximal tubule. Am. J. Physiol. 274, F1015–F1019 (1998).
Balkovetz, D. F., Chumley, P. & Amlal, H. Downregulation of claudin-2 expression in renal epithelial cells by metabolic acidosis. Am. J. Physiol. Renal Physiol. 297, F604–F611 (2009).
Barcelo, P., Wuhl, O., Servitge, E., Rousaud, A. & Pak, C. Y. C. Randomized double-blind study of potassium citrate in idiopathic hypocitraturic calcium nephrolithiasis. J. Urol. 150, 1761–1764 (1993).
Ettinger, B. et al. Potassium-magnesium citrate is an effective prophylaxis against recurrent calcium oxalate nephrolithiasis. J. Urol. 158, 2069–2073 (1997).
Hofbauer, J., Hobarth, K., Szabo, N. & Marberger, M. Alkali citrate prophylaxis in idiopathic recurrent calcium oxalate urolithiasis — a prospective randomized study. Br. J. Urol. 73, 362–365 (1994).
Soygur, T., Akbay, A. & Kupeli, S. Effect of potassium citrate therapy on stone recurrence and residual fragments after shockwave lithotripsy in lower caliceal calcium oxalate urolithiasis: a randomized controlled trial. J. Endourol. 16, 149–152 (2002).
Lojanapiwat, B. et al. Alkaline citrate reduces stone recurrence and regrowth after shockwave lithotripsy and percutaneous nephrolithotomy. Int. Braz. J. Urol. 37, 611–616 (2011).
Johnsson, M. S. & Nancollas, G. H. The role of brushite and octacalcium phosphate in apatite formation. Crit. Rev. Oral Biol. Med. 3, 61–82 (1992).
Acknowledgements
The authors' work is supported by the National Institute of Diabetes and Digestive and Kidney Diseases (PO1 DK56788).
Author information
Authors and Affiliations
Contributions
All authors researched the data, discussed the content, wrote the text and reviewed or edited the article before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Coe, F., Worcester, E. & Evan, A. Idiopathic hypercalciuria and formation of calcium renal stones. Nat Rev Nephrol 12, 519–533 (2016). https://doi.org/10.1038/nrneph.2016.101
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneph.2016.101
This article is cited by
-
Exosome-mediated crosstalk between epithelial cells amplifies the cell injury cascade in CaOx stone formation
Journal of Biological Engineering (2023)
-
Increased risk of chronic kidney disease in uric acid stone formers with high neutrophil-to-lymphocyte ratio
Scientific Reports (2023)
-
Association of acidic urine pH with impaired renal function in primary gout patients: a Chinese population-based cross-sectional study
Arthritis Research & Therapy (2022)
-
Association of functional genetic variants in TFF1 and nephrolithiasis risk in a Chinese population
BMC Urology (2022)
-
Numerical characterization of astronaut CaOx renal stone incidence rates to quantify in-flight and post-flight relative risk
npj Microgravity (2022)