Abstract
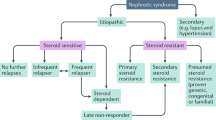
Until recently, membranoproliferative glomerulonephritis (MPGN) was clinically classified as either primary, idiopathic MPGN or as secondary MPGN when an underlying aetiology was identifiable. Primary MPGN was further classified into three types—type I, type II, and type III—based principally on the ultrastructural appearance and location of electron-dense deposits. Both the clinical and histopathologic schemes presented problems, however, as neither was based on disease pathogenesis. An improved understanding of the role of complement in the pathogenesis of MPGN has led to a proposed reclassification into immunoglobulin-mediated disease (driven by the classical complement pathway) and non-immunoglobulin-mediated disease (driven by the alternative complement pathway). This reclassification has led to improved diagnostic clinical algorithms and the emergence of a new grouping of diseases known as the C3 glomerulopathies, best represented by dense deposit disease and C3 glomerulonephritis. In this Review, we re-examine the previous and current classification schemes of MPGN, focusing on the role of complement. We survey current data about the pathogenesis of the C3 glomerulopathies, including familial studies and patient cohorts from the USA and Europe. In addition, we discuss the diagnosis, treatment, and prognosis of the C3 glomerulopathies.
Key Points
-
A new classification scheme for MPGN, centred on whether or not immunoglobulin accompanies complement on immunofluorescence, aims to capture the pathogenesis behind the MPGN lesion
-
A C3 glomerulopathy is a proliferative glomerulonephritis, usually (but not exclusively) with a MPGN pattern on light microscopy, with C3 staining alone on immunofluorescence, implicating hyperactivity of the alternative complement pathway
-
Mutations in and/or autoantibodies directed at factors that activate or regulate the C3 convertase of the alternative complement pathway can lead to dysregulation of this pathway and subsequent glomerular injury
-
Atypical hemolytic uremic syndrome is distinct from the C3 glomerulopathies in both the pattern of glomerular injury (a thrombotic microangiopathy) and phase of complement dysregulation (solid versus fluid phase)
-
Targeted and effective treatment of the C3 glomerulopathies will likely require an a priori, individualized understanding of the defect in the alternative complement pathway for each affected individual
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Tarshish, P., Bernstein, J., Tobin, J. N. & Edelmann, C. M. Jr. Treatment of mesangiocapillary glomerulonephritis with alternate-day prednisone—a report of the International Study of Kidney Disease in Children. Pediatr. Nephrol. 6, 123–130 (1992).
Fakhouri, F., Fremeaux-Bacchi, V., Noel, L. H., Cook, H. T. & Pickering, M. C. C3 glomerulopathy: a new classification. Nat. Rev. Nephrol. 6, 494–499 (2010).
Sethi, S., Nester, C. M. & Smith, R. J. Membranoproliferative glomerulonephritis and C3 glomerulopathy: resolving the confusion. Kidney Int. 81, 434–441 (2012).
Levy, M., Gubler, M. C., Sich, M., Beziau, A. & Habib, R. Immunopathology of membranoproliferative glomerulonephritis with subendothelial deposits (type I MPGN). Clin. Immunol. Immunopathol. 10, 477–492 (1978).
Habib, R., Gubler, M. C., Loirat, C., Maiz, H. B. & Levy, M. Dense deposit disease: a variant of membranoproliferative glomerulonephritis. Kidney Int. 7, 204–215 (1975).
Strife, C. F., McEnery, P. T., McAdams, A. J. & West, C. D. Membranoproliferative glomerulonephritis with disruption of the glomerular basement membrane. Clin. Nephrol. 7, 65–72 (1977).
Sethi, S. et al. Glomeruli of dense deposit disease contain components of the alternative and terminal complement pathway. Kidney Int. 75, 952–960 (2009).
Sethi, S. & Fervenza, F. C. Membranoproliferative glomerulonephritis—a new look at an old entity. N. Engl. J. Med. 366, 1119–1131 (2012).
Sethi, S. & Fervenza, F. C. Membranoproliferative glomerulonephritis: pathogenetic heterogeneity and proposal for a new classification. Semin. Nephrol. 31, 341–348 (2011).
Walker, P. D., Ferrario, F., Joh, K. & Bonsib, S. M. Dense deposit disease is not a membranoproliferative glomerulonephritis. Mod. Pathol. 20, 605–616 (2007).
D'Agati, V. D. & Bomback, A. S. C3 glomerulopathy: What's in a name? Kidney Int. 82, 379–381 (2012).
Zuber, J. et al. Use of eculizumab for atypical haemolytic uraemic syndrome and C3 glomerulopathies. Nat. Rev. Nephrol. http://dx.doi.org/10.1038/nrneph.2012.214.
Roumenina, L. T. et al. Alternative complement pathway assessment in patients with atypical HUS. J. Immunol. Methods 365, 8–26 (2011).
Zhang, Y. et al. Causes of alternative pathway dysregulation in dense deposit disease. Clin. J. Am. Soc. Nephrol. 7, 265–274 (2012).
Licht, C. & Fremeaux-Bacchi, V. Hereditary and acquired complement dysregulation in membranoproliferative glomerulonephritis. Thromb. Haemost. 101, 271–278 (2009).
Herlitz, L. C. et al. Pathology after eculizumab in dense deposit disease and C3 GN. J. Am. Soc. Nephrol. 23, 1229–1237 (2012).
Servais, A. et al. Primary glomerulonephritis with isolated C3 deposits: a new entity which shares common genetic risk factors with haemolytic uraemic syndrome. J. Med. Genet. 44, 193–199 (2007).
Licht, C. et al. Deletion of Lys224 in regulatory domain 4 of factor H reveals a novel pathomechanism for dense deposit disease (MPGN II). Kidney Int. 70, 42–50 (2006).
Habbig, S. et al. C3 deposition glomerulopathy due to a functional factor H defect. Kidney Int. 75, 1230–1234 (2009).
Gale, D. P. et al. Identification of a mutation in complement factor H-related protein 5 in patients of Cypriot origin with glomerulonephritis. Lancet 376, 794–801 (2010).
Athanasiou, Y. et al. Familial C3 glomerulopathy associated with CFHR5 mutations: clinical characteristics of 91 patients in 16 pedigrees. Clin. J. Am. Soc. Nephrol. 6, 1436–1446 (2011).
Martinez-Barricarte, R. et al. Human C3 mutation reveals a mechanism of dense deposit disease pathogenesis and provides insights into complement activation and regulation. J. Clin. Invest. 120, 3702–3712 (2010).
Ruley, E. J., Forristal, J., Davis, N. C., Andres, C. & West, C. D. Hypocomplementemia of membranoproliferative nephritis. Dependence of the nephritic factor reaction on properdin factor B. J. Clin. Invest. 52, 896–904 (1973).
Vallota, E. H. et al. A serum factor in chronic hypocomplementemic hephritis distinct from immunoglobulins and activating the alternate pathway of complement. J. Exp. Med. 139, 1249–1261 (1974).
West, C. D. Nephritic factors predispose to chronic glomerulonephritis. Am. J. Kidney Dis. 24, 956–963 (1994).
West, C. D., Witte, D. P. & McAdams, A. J. Composition of nephritic factor-generated glomerular deposits in membranoproliferative glomerulonephritis type 2. Am. J. Kidney Dis. 37, 1120–1130 (2001).
Gewurz, A. T., Imherr, S. M., Strauss, S., Gewurz, H. & Mold, C. C3 nephritic factor and hypocomplementaemia in a clinically healthy individual. Clin. Exp. Immunol. 54, 253–258 (1983).
Fremeaux-Bacchi, V. et al. Hypocomplementaemia of poststreptococcal acute glomerulonephritis is associated with C3 nephritic factor (C3NeF) IgG autoantibody activity. Nephrol. Dial. Transplant. 9, 1747–1750 (1994).
Sissons, J. G. et al. The complement abnormalities of lipodystrophy. N. Engl. J. Med. 294, 461–465 (1976).
Sethi, S. et al. C3 Glomerulonephritis: clinicopathologic findings, complement abnormalities, glomerular proteomic profile, treatment and follow-up. Kidney Int. 82, 465–473 (2012).
Bomback, A. S. et al. Eculizumab for dense deposit disease and C3 glomerulonephritis. Clin. J. Am. Soc. Nephrol. 7, 748–756 (2012).
Sethi, S. et al. Proliferative glomerulonephritis secondary to dysfunction of the alternative pathway of complement. Clin. J. Am. Soc. Nephrol. 6, 1009–1017 (2011).
Pickering, M. & Cook, H. T. Complement and glomerular disease: new insights. Curr. Opin. Nephrol. Hypertens. 20, 271–277 (2011).
Chen, Q. et al. Combined C3b and factor B autoantibodies and MPGN type II. N. Engl. J. Med. 365, 2340–2342 (2011).
Appel, G. B. et al. Membranoproliferative glomerulonephritis type II (dense deposit disease): an update. J. Am. Soc. Nephrol. 16, 1392–1403 (2005).
Radhakrishnan, S. et al. Eculizumab and refractory membranoproliferative glomerulonephritis. N. Engl. J. Med. 366, 1165–1166 (2012).
Smith, R. J. et al. New approaches to the treatment of dense deposit disease. J. Am. Soc. Nephrol. 18, 2447–2456 (2007).
Servais, A. et al. Acquired and genetic complement abnormalities play a critical role in dense deposit disease and other C3 glomerulopathies. Kidney Int. 82, 454–464 (2012).
Skerka, C. et al. Autoimmune forms of thrombotic microangiopathy and membranoproliferative glomerulonephritis: Indications for a disease spectrum and common pathogenic principles. Mol. Immunol. 46, 2801–2807 (2009).
Noris, M. & Remuzzi, G. Atypical hemolytic-uremic syndrome. N. Engl. J. Med. 361, 1676–1687 (2009).
Maga, T. K., Nishimura, C. J., Weaver, A. E., Frees, K. L. & Smith, R. J. Mutations in alternative pathway complement proteins in American patients with atypical hemolytic uremic syndrome. Hum. Mutat. 31, E1445–E1460 (2010).
Boyer, O. et al. Complement factor H deficiency and posttransplantation glomerulonephritis with isolated C3 deposits. Am. J. Kidney Dis. 51, 671–677 (2008).
Lorcy, N., Rioux-Leclercq, N., Lombard, M. L., Le Pogamp, P. & Vigneau, C. Three kidneys, two diseases, one antibody? Nephrol. Dial. Transplant. 26, 3811–3813 (2011).
Smith, R. J., Harris, C. L. & Pickering, M. C. Dense deposit disease. Mol. Immunol. 48, 1604–1610 (2011).
Schifferli, J. A., Ng, Y. C. & Peters, D. K. The role of complement and its receptor in the elimination of immune complexes. N. Engl. J. Med. 315, 488–495 (1986).
Bao, L., Haas, M. & Quigg, R. J. Complement factor H deficiency accelerates development of lupus nephritis. J. Am. Soc. Nephrol. 22, 285–295 (2011).
Alexander, J. J. et al. Mouse podocyte complement factor H: the functional analog to human complement receptor 1. J. Am. Soc. Nephrol. 18, 1157–1166 (2007).
Bridoux, F. et al. Glomerulonephritis with isolated C3 deposits and monoclonal gammopathy: a fortuitous association? Clin. J. Am. Soc. Nephrol. 6, 2165–2174 (2011).
Sethi, S. et al. Dense deposit disease associated with monoclonal gammopathy of undetermined significance. Am. J. Kidney Dis. 56, 977–982 (2010).
Sandhu, G. et al. C3 Glomerulopathy masquerading as acute postinfectious glomerulonephritis. Am. J. Kidney Dis. http://dx.doi.org/10.1053/j.ajkd.2012.04.032.
Halbwachs, L., Leveille, M., Lesavre, P., Wattel, S. & Leibowitch, J. Nephritic factor of the classical pathway of complement: immunoglobulin G autoantibody directed against the classical pathway C3 convertase enzyme. J. Clin. Invest. 65, 1249–1256 (1980).
Nasr, S. H. et al. Dense deposit disease: clinicopathologic study of 32 pediatric and adult patients. Clin. J. Am. Soc. Nephrol. 4, 22–32 (2009).
Kidney Disease: Improving Global Outcomes (KDIGO) Glomerulonephritis Work Group. KDIGO Clinical Practice Guideline for Glomerulonephritis. Kidney Int. Suppl. 2, 139–274 (2012).
Fakhouri, F. et al. Treatment with human complement factor H rapidly reverses renal complement deposition in factor H-deficient mice. Kidney Int. 78, 279–286 (2010).
Hillmen, P. et al. The complement inhibitor eculizumab in paroxysmal nocturnal hemoglobinuria. N. Engl. J. Med. 355, 1233–1243 (2006).
Kose, O., Zimmerhackl, L. B., Jungraithmayr, T., Mache, C. & Nurnberger, J. New treatment options for atypical hemolytic uremic syndrome with the complement inhibitor eculizumab. Semin. Thromb. Hemost. 36, 669–672 (2010).
Vivarelli, M., Pasini, A. & Emma, F. Eculizumab for the treatment of dense-deposit disease. N. Engl. J. Med. 366, 1163–1165 (2012).
Daina, E., Noris, M. & Remuzzi, G. Eculizumab in a patient with dense-deposit disease. N. Engl. J. Med. 366, 1161–1163 (2012).
McCaughan, J. A., O'Rourke, D. M. & Courtney, A. E. Recurrent dense deposit disease after renal transplantation: an emerging role for complementary therapies. Am. J. Transplant. 12, 1046–1051 (2012).
Lorenz, E. C. et al. Recurrent membranoproliferative glomerulonephritis after kidney transplantation. Kidney Int. 77, 721–728 (2010).
Karakayali, F. Y. et al. Recurrent glomerular diseases after renal transplantation. Transplant. Proc. 38, 470–472 (2006).
Saxena, R., Frankel, W. L., Sedmak, D. D., Falkenhain, M. E. & Cosio, F. G. Recurrent type I membranoproliferative glomerulonephritis in a renal allograft: successful treatment with plasmapheresis. Am. J. Kidney Dis. 35, 749–752 (2000).
Mache, C. J. et al. Complement inhibitor eculizumab in atypical hemolytic uremic syndrome. Clin. J. Am. Soc. Nephrol. 4, 1312–1316 (2009).
Nester, C. et al. Pre-emptive eculizumab and plasmapheresis for renal transplant in atypical hemolytic uremic syndrome. Clin. J. Am. Soc. Nephrol. 6, 1488–1494 (2011).
Acknowledgements
The authors of this manuscript are supported by the Center for Glomerular Diseases at Columbia University, New York, USA.
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of this manuscript.
Corresponding author
Ethics declarations
Competing interests
A. S. Bomback declares an association with the following company: Alexion Pharmaceuticals (grant/research support).
G. B. Appel declares an association with the following company: Alexion Pharmaceuticals (consultant; grant/research support).
Rights and permissions
About this article
Cite this article
Bomback, A., Appel, G. Pathogenesis of the C3 glomerulopathies and reclassification of MPGN. Nat Rev Nephrol 8, 634–642 (2012). https://doi.org/10.1038/nrneph.2012.213
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneph.2012.213
This article is cited by
-
Diagnose und Therapie glomerulärer Erkrankungen mit einem membranoproliferativen Läsionsmuster (MPGN) – 2023
Wiener klinische Wochenschrift (2023)
-
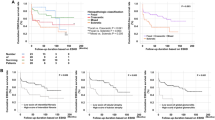
Therapy and outcomes of C3 glomerulopathy and immune-complex membranoproliferative glomerulonephritis
Pediatric Nephrology (2021)
-
C3-glomerulonephritis in New Zealand – a case series
BMC Nephrology (2020)
-
An update to the pathogenesis for monoclonal gammopathy of renal significance
Annals of Hematology (2020)
-
Characteristics of membranoproliferative glomerulonephritis based on a new classification at a single center
Clinical and Experimental Nephrology (2019)