Key Points
-
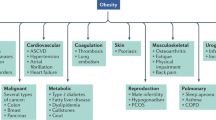
Obesity is a complex disease that is rapidly increasing in the Western world and is inextricably linked to type 2 diabetes, heart disease, inflammatory diseases and cancer.
-
There are two long-term treatments for obesity: sibutramine, which acts centrally by suppressing appetite; and orlistat, which acts on a peripheral target that is involved in dietary fat absorption.
-
The hydrolysis, transport and de novo synthesis pathways that are involved in lipid homeostasis present a pool of enzymes and transporters, some of which have been shown to be druggable, including acyl CoA:cholesterol acyltransferase (ACAT) and carnitine palmitoyl transferase (CPT1). The chemical structure of the inhibitors of these enzymes could prove useful in the design of new obesity drugs.
-
Improved mobilization of fat has potential as an anti-obesity strategy, but needs to be balanced with increased fat metabolism to avoid problems with lipotoxicity.
-
The malonyl-CoA/CPT1 axis is involved in regulating fatty-acid β-oxidation and merits further investigation. The most promising target in this pathway is acyl-CoA carboxylase-2 (ACC2): knockout of this enzyme in mice results in increased fatty-acid oxidation and resistance to diabetes-induced obesity, lower fatty-acid levels and improved insulin sensitivity.
Abstract
Obesity is a complex disease that is regulated by both central and peripheral mechanisms. New medicines for the treatment and prevention of obesity will need to overcome the powerful compensatory responses of the overlapping, and often redundant, networks that have evolved to safeguard efficient energy use. Despite great progress in the identification of central signals that regulate satiety, and considerable investment in the development of appetite-controlling medications, success has been modest so far. Here we review the main enzymes that are involved in different stages of lipid metabolism — from digestion and absorption through synthesis and storage to mobilization and oxidation — which might be successfully targeted by new pharmacotherapies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
National Institutes of Health (NIH), National Heart, Lung, and Blood Institute (NHLBI). Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity: the evidence report (US Government Press, Washington DC, 1998).
Campfield, L. A., Smith, F. J. & Burn, P. Strategies and potential molecular targets for obesity treatment. Science 280, 1383–1387 (1998). This review outlines different strategies for obesity drug development by targeting both central and peripheral mechanisms.
Hill, J. O., Melanson, E. L. & Wyatt, H. T. Dietary fat intake and regulation of energy balance: implications for obesity. J. Nutr. 130, 284S–288S (2000).
Carriere, F. et al. Gastric and pancreatic lipase levels during a test meal in dogs. Scand. J. Gastroenterol. 28, 443–454 (1993).
Nordskog, B. K., Phan, C. T., Nutting, D. F. & Tso, P. An examination of the factors affecting intestinal lymphatic transport of dietary lipids. Adv. Drug Deliv. Rev. 50, 21–44 (2001).
Phan, C. T. & Tso, P. Intestinal lipid absorption and transport. Front. Biosci. 6, D299–D319 (2001).
Kawai, T. & Fushiki, T. Importance of lipolysis in oral cavity for orosensory detection of fat. Am. J. Phys. Regul. Integr. Comp. Physiol. 285, R447–R454 (2003).
Miled, N. et al. Digestive lipases: from three-dimensional structure to physiology. Biochimie 82, 973–986 (2000).
Ghishan, F. K., Moran, J. R., Durie, P. R. & Greene, H. L. Isolated congenital lipase-colipase deficiency. Gastroenterology 86, 1580–1582 (1984).
Carriere, F., Barrowman, J. A., Verger, R. & Laugier, R. Secretion and contribution to lipolysis of gastric and pancreatic lipases during a test meal in humans. Gastroenterology 105, 876–888 (1993).
Borgstrom, B. Binding of pancreatic colipase to interfaces: effects of detergents. FEBS Lett. 71, 201–204 (1976).
Bowyer, R. C., Rowston, W. M., Jehanli, A. M., Lacey, J. H. & Hermon-Taylor, J. Effect of a satiating meal on the concentrations of procolipase propeptide in the serum and urine of normal and morbidly obese subjects. Gut 34, 1520–1525 (1993).
Weibel, E. K., Hadvary, P., Hochuli, E., Kupfer, E. & Lengsfeld, H. Lipstatin, an inhibitor of pancreatic lipase, produced by Streptomyces toxytricini. I. Producing organism, fermentation, isolation and biological activity. J. Antibiot. 40, 1081–1085 (1987).
Bitou, N., Ninomiya, M., Tsujita, T. & Okuda, H. Screening of lipase inhibitors from marine algae. Lipids 34, 441–445 (1999).
Zhi, J., Mulligan, T. E. & Hauptman, J. B. Long-term systemic exposure of orlistat, a lipase inhibitor, and its metabolites in obese patients. J. Clin. Pharmacol. 39, 41–46 (1999).
Hadvary, P., Sidler, W., Meister, W., Vetter, W. & Wolfer, H. The lipase inhibitor tetrahydrolipstatin binds covalently to the putative active site serine of pancreatic lipase. J. Biol. Chem. 266, 2021–2027 (1991).
Lucas, C. P., Boldrin, M. N. & Reaven, G. M. Effect of orlistat added to diet (30% of calories from fat) on plasma lipids, glucose, and insulin in obese patients with hypercholesterolemia. Am. J. Cardiol. 91, 961–964 (2003).
Padwal, R., Li, S. K. & Lau, D. C. W. Long-term pharmacotherapy for overweight and obesity: a systematic review and meta-analysis of randomized controlled trials. Int. J. Obes. 27, 1437–1446 (2003).
Hanefeld, M. & Sachse, G. The effects of orlistat on body weight and glycaemic control in overweight patients with type 2 diabetes: a randomized, placebo-controlled trial. Diabetes Obes. Metab. 4, 415–423 (2002).
Carey, M. C., Small, D. M. & Bliss, C. M. Lipid digestion and absorption. Annu. Rev. Physiol. 45, 651–677 (1983).
Huggins, K. W., Boileau, A. C. & Hui, D. Y. Protection against diet-induced obesity and obesity-related insulin resistance in group 1B PLA2-deficient mice. Am. J. Physiol. Endocrinol. Metab. 283, E994–E1001 (2002). This study describes the role of pancreatic sPLA2 in dietary fat absorption.
Richmond, B. L. et al. Compensatory phospholipid digestion is required for cholesterol absorption in pancreatic phospholipase A(2)-deficient mice. Gastroenterology 120, 1193–1202 (2001).
Chang, T. M., Chang, C. H., Wagner, D. R. & Chey, W. Y. Porcine pancreatic phospholipase A2 stimulates secretin release from secretin-producing cells. J. Biol. Chem. 274, 10758–10764 (1999).
Ma, T. et al. Defective dietary fat processing in transgenic mice lacking aquaporin-1 water channels. Am. J. Physiol. Cell Physiol. 280, C126–C134 (2001).
Richmond, B. L. & Hui, D. Y. Molecular structure and tissue-specific expression of the mouse pancreatic phospholipase A(2) gene. Gene 244, 65–72 (2000).
Murakami, M. & Kudo, I. Phospholipase A2. J. Biochem. 131, 285–292 (2002).
Yuan, C. & Tsai, M. Pancreatic phospholipase A(2): new views on old issues. Biochim. Biophys. Acta 23, 215–222 (1999).
Mihelich, E. D. & Schevitz, R. W. Structure-based design of a new class of anti-inflammatory drugs: secretory phospholipase A(2) inhibitors, SPI. Biochim. Biophys. Acta 23, 223–228 (1999).
Niessen, H. W. M., Krijnen, P. A. J., Visser, C. A., Meijer, C. & Hack, C. E. Type II secretory phospholipase A2 in cardiovascular disease: a mediator in atherosclerosis and ischemic damage to cardiomyocytes? Cardiovasc. Res. 60, 68–77 (2003).
Yuan, C., Byeon, I. J., Poi, M. J. & Tsai, M. D. Structural analysis of phospholipase A2 from functional perspective. 2. Characterization of a molten globule-like state induced by site-specific mutagenesis. Biochemistry 38, 2919–2929 (1999).
Hajri, T. & Abumrad, N. A. Fatty acid transport across membranes: relevance to nutrition and metabolic pathology. Annu. Rev. Nutr. 22, 383–415 (2002).
Kamp, F. et al. Rapid flip-flop of oleic acid across the plasma membrane of adipocytes. J. Biol. Chem. 278, 7988–7995 (2003). This research shows that passive diffusion is an efficient process for fatty acids entering the adipocytes.
Vassileva, G., Huwyler, L., Poirier, K., Agellon, L. B. & Toth, M. J. The intestinal fatty acid binding protein is not essential for dietary fat absorption in mice. FASEB J. 14, 2040–2046 (2000).
Abumrad, N. A., el-Maghrabi, M. R., Amri, E. Z., Lopez, E. & Grimaldi, P. A. Cloning of a rat adipocyte membrane protein implicated in binding or transport of long-chain fatty acids that is induced during preadipocyte differentiation. Homology with human CD36. J. Biol. Chem. 268, 17665–17668 (1993).
Chen, M., Yang, Y., Braunstein, E., Georgeson, K. E. & Harmon, C. M. Gut expression and regulation of FAT/CD36: possible role in fatty acid transport in rat enterocytes. Am. J. Physiol. Endocrinol. Metab. 281, E916–E923 (2001).
Poirier, H., Degrace, P., Niot, I., Bernard, A. & Besnard, P. Localization and regulation of the putative membrane fatty-acid transporter (FAT) in the small intestine. Comparison with fatty acid-binding proteins (FABP). Eur. J. Biochem. 238, 368–373 (1996).
Greenwalt, D. E., Scheck, S. H. & Rhinehart-Jones, T. Heart CD36 expression is increased in murine models of diabetes and in mice fed a high fat diet. J. Clin. Invest. 96, 1382–1388 (1995).
Goudriaan, J. R. et al. Intestinal lipid absorption is not affected in CD36 deficient mice. Mol. Cell. Biochem. 239, 199–202 (2002).
Schaffer, J. E. & Lodish, H. F. Expression cloning and characterization of a novel adipocyte long chain fatty acid transport protein. Cell 79, 427–436 (1994).
Gimeno, R. E. et al. Targeted deletion of fatty acid transport protein-4 results in early embryonic lethality. J. Biol. Chem. 278, 49512–49516 (2003).
Herrmann, T. et al. Mouse fatty acid transport protein 4 (FATP4): characterization of the gene and functional assessment as a very long chain acyl-CoA synthetase. Gene 270, 31–40 (2001).
Coleman, R. A. & Lee, D. P. Enzymes of triacylglycerol synthesis and their regulation. Prog. Lipid Res. 43, 134–176 (2004). This paper provides a comprehensive review of the latest developments in lipid metabolic enzymes.
Polheim, D., David, J. S., Schultz, F. M., Wylie, M. B. & Johnston, J. M. Regulation of triglyceride biosynthesis in adipose and intestinal tissue. J. Lipid Res. 14, 415–421 (1973).
Yen, C. L., Stone, S. J., Cases, S., Zhou, P. & Farese, R. V. Jr. Identification of a gene encoding MGAT1, a monoacylglycerol acyltransferase. Proc. Natl Acad. Sci. USA 99, 8512–8517 (2002).
Cao, J., Lockwood, J., Burn, P. & Shi, Y. Cloning and functional characterization of a mouse intestinal Acyl-CoA:monoacylglycerol acyltransferase, MGAT2. J. Biol. Chem. 278, 13860–13866 (2003).
Cao, J. et al. A predominant role of acyl-CoA:monoacylglycerol acyltransferase-2 in dietary fat absorption implicated by tissue distribution, subcellular localization, and up-regulation by high fat diet. J. Biol. Chem. 279, 18878–18886 (2004). This report provides direct evidence that MGAT2 is important in dietary fat absorption and diet-induced obesity.
Cheng, D. et al. Identification of acyl coenzyme A:monoacylglycerol acyltransferase 3, an intestinal specific enzyme implicated in dietary fat absorption. J. Biol. Chem. 278, 13611–13614 (2003).
Yen, C. L. & Farese, R. V. Jr. MGAT2, a monoacylglycerol acyltransferase expressed in the small intestine. J. Biol. Chem. 278, 18532–18537 (2003).
Lockwood, J. F., Cao, J., Burn, P. & Shi, Y. Human intestinal monoacylglycerol acyltransferase: differential features in tissue expression and activity. Am. J. Physiol. Endocrinol. Metab. 285, E927–E937 (2003).
Mostafa, N., Bhat, B. G. & Coleman, R. A. Increased hepatic monoacylglycerol acyltransferase activity in streptozotocin-induced diabetes: characterization and comparison with activities from adult and neonatal rat liver. Biochim. Biophys. Acta 1169, 189–195 (1993).
Luan, Y. et al. Pathogenesis of obesity by food restriction in OLETF rats: increased intestinal monoacylglycerol acyltransferase activities may be a crucial factor. Diabetes Res. Clin. Prac. 57, 75–82 (2002).
Sudhop, T. & von Bergmann, K. Cholesterol absorption inhibitors for the treatment of hypercholesterolaemia. Drugs 62, 2333–2347 (2002).
Hideshima, T. et al. Antitumor activity of lysophosphatidic acid acyltransferase-β inhibitors, a novel class of agents, in multiple myeloma. Cancer Res. 63, 8428–8436 (2003).
Coon, M. et al. Inhibition of lysophosphatidic acid acyltransferase disrupts proliferative and survival signals in normal cells and induces apoptosis of tumor cells. Mol. Cancer Ther. 2, 1067–1078 (2003).
Thomson, A. B., Cheeseman, C. I., Keelan, M., Fedorak, R. & Clandinin, M. T. Crypt cell production rate, enterocyte turnover time and appearance of transport along the jejunal villus of the rat. Biochim. Biophys. Acta. 1191, 197–204 (1994).
Bakillah, A. & El Abbouyi, A. The role of microsomal triglyceride transfer protein in lipoprotein assembly: an update. Front. Biosci. 8, D294–D305 (2003).
Hussain, M. M. A proposed model for the assembly of chylomicrons. Atherosclerosis 148, 1–15 (2000).
Wetterau, J. R. et al. An mtp inhibitor that normalizes atherogenic lipoprotein levels in WHHL rabbits. Science 282, 751–754 (1998). This paper reports on the first generation of MTP inhibitors that are effective in lowering TAG in rodents.
Ksander, G. M. et al. Diaminoindanes as microsomal triglyceride transfer protein inhibitors. J. Med. Chem. 44, 4677–4687 (2001).
Shiomi, M. & Ito, T. MTP inhibitor decreases plasma cholesterol levels in LDL receptor-deficient WHHL rabbits by lowering the VLDL secretion. Eur. J. Pharmacol. 431, 127–131 (2001).
Robl, J. A. et al. A novel series of highly potent benzimidazole-based microsomal triglyceride transfer protein inhibitors. J. Med. Chem. 44, 851–856 (2001).
Chandler, C. E. et al. CP-346086: an MTP inhibitor that lowers plasma cholesterol and triglycerides in experimental animals and in humans. J. Lipid Res. 44, 1887–1901 (2003).
Levy, E. The genetic basis of primary disorders of intestinal fat transport. Clin. Invest. Med. 19, 317–324 (1996).
Lewis, G. F., Carpentier, A., Adeli, K. & Giacca, A. Disordered fat storage and mobilization in the pathogenesis of insulin resistance and type 2 diabetes. Endocr. Rev. 23, 201–229 (2002).
Shimomura, I. et al. Insulin resistance and diabetes mellitus in transgenic mice expressing nuclear srebp-1c in adipose tissue: model for congenital generalized lipodystrophy. Genes Dev. 12, 3182–3194 (1998).
Moitra, J. et al. Life without white fat: a transgenic mouse. Genes Dev. 12, 3168–3181 (1998).
Agarwal, A. K. & Garg, A. Congenital generalized lipodystrophy: significance of triglyceride biosynthetic pathways. Trends Endocrinol. Metab. 14, 214–221 (2003).
Hanson, R. W. & Reshef, L. Glyceroneogenesis revisited. Biochimie 85, 1199–1205 (2003).
Leung, D. W. The structure and functions of human lysophosphatidic acid acyltransferases. Front. Biosci. 6, D944–D953 (2001).
Ruan, H. & Pownall, H. J. Overexpression of 1-acyl-glycerol-3-phosphate acyltransferase-α enhances lipid storage in cellular models of adipose tissue and skeletal muscle. Diabetes 50, 233–240 (2001).
Cases, S. et al. Identification of a gene encoding an acyl CoA:diacylglycerol acyltransferase, a key enzyme in triacylglycerol synthesis. Proc. Natl Acad. Sci. USA 95, 13018–13023 (1998).
Cases, S. et al. Cloning of DGAT2, a second mammalian diacylglycerol acyltransferase, and related family members. J. Biol. Chem. 276, 38870–38876 (2001).
Ludwig, E. H. et al. DGAT1 promoter polymorphism associated with alterations in body mass index, high density lipoprotein levels and blood pressure in Turkish women. Clin. Genet. 62, 68–73 (2002).
Yu, Y. H. et al. Posttranscriptional control of the expression and function of diacylglycerol acyltransferase-1 in mouse adipocytes. J. Biol. Chem. 277, 50876–50884 (2002).
Stone, S. J. et al. Lipopenia and skin barrier abnormalities in DGAT2-deficient mice. J. Biol. Chem. 279, 11767–11776 (2003). This study shows that DGAT1 and DGAT2 have different roles in lipid metabolism.
Buhman, K. K. et al. DGAT1 is not essential for intestinal triacylglycerol absorption or chylomicron synthesis. J. Biol. Chem. 277, 25474–25479 (2002).
Smith, S. J. et al. Obesity resistance and multiple mechanisms of triglyceride synthesis in mice lacking Dgat. Nature Genet. 25, 87–90 (2000).
Chen, H. C., Ladha, Z., Smith, S. J. & Farese, R. V. Jr. Analysis of energy expenditure at different ambient temperatures in mice lacking DGAT1. Am. J. Physiol. Endocrinol. Metab. 284, E213–E218 (2003).
Chen, H. C., Jensen, D. R., Myers, H. M., Eckel, R. H. & Farese, R. V. Obesity resistance and enhanced glucose metabolism in mice transplanted with white adipose tissue lacking acyl CoA:diacylglycerol acyltransferase 1. J. Clin. Invest. 111, 1715–1722 (2003). This study illustrates that DGAT1 in adipose tissue is important in regulating energy homeostasis.
Gibbons, G. F., Islam, K. & Pease, R. J. Mobilisation of triacylglycerol stores. Biochim. Biophys. Acta 1483, 37–57 (2000).
Tomoda, H., Namatame, I. & Omura, S. Microbial metabolites with inhibitory activity against lipid metabolism. Proc. Jpn Acad. Ser. B Phys. Biol. Sci. 78, 217–240 (2002).
Holm, C., Osterlund, T., Laurell, H. & Contreras, J. A. Molecular mechanisms regulating hormone-sensitive lipase and lipolysis. Annu. Rev. Nutr. 20, 365–393 (2000).
Sztalryd, C. & Kraemer, F. B. Regulation of hormone-sensitive lipase during fasting. Am. J. Physiol. 266, E179–E185 (1994).
Large, V. et al. Decreased expression and function of adipocyte hormone-sensitive lipase in subcutaneous fat cells of obese subjects. J. Lipid Res. 40, 2059–2066 (1999).
Garenc, C. et al. The hormone-sensitive lipase gene and body composition: the HERITAGE family study. Int. J. Obes. 26, 220–227 (2002).
Lucas, S., Tavernier, G., Tiraby, C., Mairal, A. & Langin, D. Expression of human hormone-sensitive lipase in white adipose tissue of transgenic mice increases lipase activity but does not enhance in vitro lipolysis. J. Lipid Res. 44, 154–163 (2003).
Haemmerle, G. et al. Hormone-sensitive lipase deficiency in mice causes diglyceride accumulation in adipose tissue, muscle, and testis. J. Biol. Chem. 277, 4806–4815 (2002).
Sekiya, M. et al. Absence of hormone-sensitive lipase inhibits obesity and adipogenesis in Lep(ob/ob) mice. J. Biol. Chem. 279, 15084–15090 (2004).
Mulder, H. et al. Hormone-sensitive lipase null mice exhibit signs of impaired insulin sensitivity whereas insulin secretion is intact. J. Biol. Chem. 278, 36380–36388 (2003).
Osuga, J. et al. Targeted disruption of hormone-sensitive lipase results in male sterility and adipocyte hypertrophy, but not in obesity. Proc. Natl Acad. Sci. USA 97, 787–792 (2000).
Wei, Y. et al. Crystal structure of brefeldin A esterase, a bacterial homolog of the mammalian hormone-sensitive lipase. Nature Struct. Biol. 6, 340–345 (1999).
Tansey, J. T. et al. Functional studies on native and mutated forms of perilipins: a role in protein kinase A-mediated lipolysis of triacylglycerols in Chinese hamster ovary cells. J. Biol. Chem. 278, 8401–8406 (2003).
Miura, S. et al. Functional conservation for lipid storage droplet association among Perilipin, ADRP, and TIP47 (PAT)-related proteins in mammals, Drosophila, and Dictyostelium. J. Biol. Chem. 277, 32253–32257 (2002).
Tansey, J. T. et al. Perilipin ablation results in a lean mouse with aberrant adipocyte lipolysis, enhanced leptin production, and resistance to diet-induced obesity. Proc. Natl Acad. Sci. USA 98, 6494–6499 (2001).
Martinez-Botas, J. et al. Absence of perilipin results in leanness and reverses obesity in Lepr (db/db) mice. Nature Genet. 26, 474–479 (2000). References 94 and 95 show the importance of perilipin in regulating lipid metabolism.
Castro-Chavez, F. et al. Coordinated upregulation of oxidative pathways and downregulation of lipid biosynthesis underlie obesity resistance in perilipin knockout mice: a microarray gene expression profile. Diabetes 52, 2666–2674 (2003).
Sul, H. S. & Wang, D. Nutritional and hormonal regulation of enzymes in fat synthesis — studies of fatty acid synthase and mitochondrial glycerol-3-phosphate acyltransferase gene transcription. Annu. Rev. Nutr. 18, 331–351 (1998).
Park, H. et al. Coordinate regulation of malonyl-CoA decarboxylase, sn-glycerol-3-phosphate acyltransferase, and acetyl-CoA carboxylase by AMP-activated protein kinase in rat tissues in response to exercise. J. Biol. Chem. 277, 32571–32577 (2002).
Zhou, Y. T., Wang, Z. W., Higa, M., Newgard, C. B. & Unger, R. H. Reversing adipocyte differentiation: implications for treatment of obesity. Proc. Natl Acad. Sci. USA 96, 2391–2395 (1999).
Dircks, L. K. & Sul, H. S. Mammalian mitochondrial glycerol-3-phosphate acyltransferase. Biochim. Biophys. Acta 1348, 17–26 (1997).
Igal, R. A., Wang, S. L., Gonzalez-Baro, M. & Coleman, R. A. Mitochondrial glycerol phosphate acyltransferase directs the incorporation of exogenous fatty acids into triacylglycerol. J. Biol. Chem. 276, 42205–42212 (2001).
Hammond, L. E. et al. Mitochondrial glycerol-3-phosphate acyltransferase-deficient mice have reduced weight and liver triacylglycerol content and altered glycerolipid fatty acid composition. Mol. Cell. Biol. 22, 8204–8214 (2002). This paper provides evidence that GPAT1 regulates both lipid synthesis and composition.
Smith, S., Witkowski, A. & Joshi, A. K. Structural and functional organization of the animal fatty acid synthase. Prog. Lipid Res. 42, 289–317 (2003).
Jayakumar, A. et al. Human fatty acid synthase: properties and molecular cloning. Proc. Natl Acad. Sci. USA 92, 8695–8699 (1995).
Kuhajda, F. P. Fatty-acid synthase and human cancer: new perspectives on its role in tumor biology. Nutrition 16, 202–208 (2000).
Kuhajda, F. P. et al. Synthesis and antitumor activity of an inhibitor of fatty acid synthase. Proc. Natl Acad. Sci. USA 97, 3450–3454 (2000). A report on the synthesis of C75, which is one of the most commonly used FAS inhibitors.
Loftus, T. M. et al. Reduced food intake and body weight in mice treated with fatty acid synthase inhibitors. Science 288, 2379–2381 (2000).
Shimokawa, T., Kumar, M. V. & Lane, M. D. Effect of a fatty acid synthase inhibitor on food intake and expression of hypothalamic neuropeptides. Proc. Natl Acad. Sci. USA 99, 66–71 (2002).
Hu, Z. Y., Cha, S. H., Chohnan, S. & Lane, M. D. Hypothalamic malonyl-CoA as a mediator of feeding behavior. Proc. Natl Acad. Sci. USA 100, 12624–12629 (2003). References 107–109 provide comprehensive evidence that malonyl-CoA has a central role in regulating appetite.
Takahashi, K. A., Smart, J. L., Liu, H. & Cone, R. D. The anorexigenic fatty acid synthase inhibitor, C75, is a non-specific neuronal activator. Endocrinology 25, 25 (2003). This report questions the validity of C75 as an authentic FAS inhibitor.
Schlesinger, M. J. & Malfer, C. Cerulenin blocks fatty acid acylation of glycoproteins and inhibits vesicular stomatitis and Sindbis virus particle formation. J. Biol. Chem. 257, 9887–9890 (1982).
Lawrence, D. S., Zilfou, J. T. & Smith, C. D. Structure– activity studies of cerulenin analogues as protein palmitoylation inhibitors. J. Med. Chem. 42, 4932–4941 (1999).
Thupari, J. N., Pinn, M. L. & Kuhajda, F. P. Fatty acid synthase inhibition in human breast cancer cells leads to malonyl-CoA-induced inhibition of fatty acid oxidation and cytotoxicity. Biochem. Biophys. Res. Comm. 285, 217–223 (2001).
Thupari, J. N., Landree, L. E., Ronnett, G. V. & Kuhajda, F. P. C75 increases peripheral energy utilization and fatty acid oxidation in diet-induced obesity. Proc. Natl Acad. Sci. USA 99, 9498–9502 (2002).
Chirala, S. S. et al. Fatty acid synthesis is essential in embryonic development: fatty acid synthase null mutants and most of the heterozygotes die in utero. Proc. Natl Acad. Sci. USA 100, 6358–6363 (2003).
Metzger, D., Clifford, J., Chiba, H. & Chambon, P. Conditional site-specific recombination in mammalian cells using a ligand-dependent chimeric Cre recombinase. Proc. Natl Acad. Sci. USA 92, 6991–6995 (1995).
van der Leij, F. R., Huijkman, N. C. A., Boomsma, C., Kuipers, J. R. G. & Bartelds, B. Genomics of the human carnitine acyltransferase genes. Mol. Genet. Metab. 71, 139–153 (2000).
McGarry, J. D. & Brown, N. F. The mitochondrial carnitine palmitoyltransferase system — from concept to molecular analysis. Eur. J. Biochem. 244, 1–14 (1997).
Awan, M. M. & Saggerson, E. D. Malonyl-CoA metabolism in cardiac myocytes and its relevance to the control of fatty acid oxidation. Biochem. J. 295, 61–66 (1993).
Hamilton, C. & Saggerson, E. D. Malonyl-CoA metabolism in cardiac myocytes. Biochem. J. 350, 61–67 (2000).
Saddik, M., Gamble, J., Witters, L. A. & Lopaschuk, G. D. Acetyl-CoA carboxylase regulation of fatty acid oxidation in the heart. J. Biol. Chem. 268, 25836–25845 (1993).
Ruderman, N. B., Saha, A. K., Vavvas, D. & Witters, L. A. Malonyl-CoA, fuel sensing, and insulin resistance. Am. J. Physiol. Endocrinol. Metab. 39, E1–E18 (1999).
Winder, W. W. Malonyl-CoA: regulator of fatty acid oxidation in muscle during exercise. Exerc. Sport Sci. Rev. 26, 117–132 (1998).
An, J. et al. Hepatic expression of malonyl-CoA decarboxylase reverses muscle, liver and whole-animal insulin resistance. Nature Med. 10, 268–274 (2004). This paper shows that malonyl-CoA is an important regulator of peripheral energy metabolism.
Kim, J. Y., Hickner, R. C., Cortright, R. L., Dohm, G. L. & Houmard, J. A. Lipid oxidation is reduced in obese human skeletal muscle. Am. J. Physiol. Endocrinol. Metab. 279, E1039–E1044 (2000).
Dobbins, R. L. et al. Prolonged inhibition of muscle carnitine palmitoyltransferase-1 promotes intramyocellular lipid accumulation and insulin resistance in rats. Diabetes 50, 123–130 (2001). This study questions the validity of CPT1 inhibitors as a treatment for diabetes.
Sacksteder, K. A., Morrell, J. C., Wanders, R. J., Matalon, R. & Gould, S. J. MCD encodes peroxisomal and cytoplasmic forms of malonyl-CoA decarboxylase and is mutated in malonyl-CoA decarboxylase deficiency. J. Biol. Chem. 274, 24461–24468 (1999).
Gobin, S. et al. Functional and structural basis of carnitine palmitoyltransferase 1A deficiency. J. Biol. Chem. 278, 50428–50434 (2003).
Thuillier, L. et al. Correlation between genotype, metabolic data, and clinical presentation in carnitine palmitoyltransferase 2 (CPT2) deficiency. Hum. Mutat. 21, 493–501 (2003).
Lahjouji, K., Mitchell, G. A. & Qureshi, I. A. Carnitine transport by organic cation transporters and systemic carnitine deficiency. Mol. Genet. Metab. 73, 287–297 (2001).
Jackson, V. N., Zammit, V. A. & Price, N. T. Identification of positive and negative determinants of malonyl-CoA sensitivity and carnitine affinity within the amino termini of rat liver- and muscle-type carnitine palmitoyltransferase I. J. Biol. Chem. 275, 38410–38416 (2000).
Morillas, M. et al. Identification of conserved amino acid residues in rat liver carnitine palmitoyltransferase I critical for malonyl-CoA inhibition: mutation of methionine 593 abolishes malonyl-CoA inhibition. J. Biol. Chem. 278, 9058–9063 (2003).
Shi, J. Y., Zhu, H. F., Arvidson, D. N. & Woldegiorgis, G. A single amino acid change (substitution of glutamate 3 with alanine) in the N-terminal region of rat liver carnitine palmitoyltransferase I abolishes malonyl-CoA inhibition and high affinity binding. J. Biol. Chem. 274, 9421–9426 (1999).
Zhu, H. et al. Substitution of glutamate-3, valine-19, leucine-23, and serine-24 with alanine in the N-terminal region of human heart muscle carnitine palmitoyltransferase I abolishes malonyl CoA inhibition and binding. Arch. Biochem. Biophys. 413, 67–74 (2003).
Jogl, G. & Tong, L. Crystal structure of carnitine acetyltransferase and implications for the catalytic mechanism and fatty acid transport. Cell 112, 113–122 (2003).
Anderson, R. C. Carnitine palmitoyltransferase: a viable target for the treatment of NIDDM? Curr. Pharm. Des. 4, 1–16 (1998).
Giannessi, F. et al. Discovery of a long-chain carbamoyl aminocarnitine derivative, a reversible carnitine palmitoyltransferase inhibitor with antiketotic and antidiabetic activity. J. Med. Chem. 46, 303–309 (2003).
Abu-Elheiga, L., Matzuk, M. M., Abo-Hashema, K. A. & Wakil, S. J. Continuous fatty acid oxidation and reduced fat storage in mice lacking acetyl-CoA carboxylase 2. Science 291, 2613–2616 (2001). This study provides direct evidence that ACC2 has a pivotal role in regulating lipid oxidation.
Kashfi, K. & Cook, G. A. Topology of hepatic mitochondrial carnitine palmitoyltransferase I. Adv. Exp. Med. Biol. 466, 27–42 (1999).
Abu-Elheiga, L., Almarza-Ortega, D. B., Baldini, A. & Wakil, S. J. Human acetyl-CoA carboxylase 2. Molecular cloning, characterization, chromosomal mapping, and evidence for two isoforms. J. Biol. Chem. 272, 10669–10677 (1997).
Abu-Elheiga, L. et al. The subcellular localization of acetyl-CoA carboxylase 2. Proc. Natl Acad. Sci. USA 97, 1444–1449 (2000).
Zhang, L., Joshi, A. K. & Smith, S. Cloning, expression, characterization, and interaction of two components of a human mitochondrial fatty acid synthase. Malonyltransferase and acyl carrier protein. J. Biol. Chem. 278, 40067–40074 (2003).
Hardie, D. G. & Pan, D. A. Regulation of fatty acid synthesis and oxidation by the AMP-activated protein kinase. Biochem. Soc. Trans. 30, 1064–1070 (2002).
Munday, M. R. Regulation of mammalian acetyl-CoA carboxylase. Biochem. Soc. Trans. 30, 1059–1064 (2002).
Kudo, N., Barr, A. J., Barr, R. L., Desai, S. & Lopaschuk, G. D. High rates of fatty acid oxidation during reperfusion of ischemic hearts are associated with a decrease in malonyl-CoA levels due to an increase in 5′-AMP-activated protein kinase inhibition of acetyl-CoA carboxylase. J. Biol. Chem. 270, 17513–17520 (1995).
Winder, W. W. & Hardie, D. G. Inactivation of acetyl-CoA carboxylase and activation of AMP-activated protein kinase in muscle during exercise. Am. J. Physiol. 270, E299–E304 (1996).
Hopkins, T. A., Dyck, J. R. B. & Lopaschuk, G. D. AMP-activated protein kinase regulation of fatty acid oxidation in the ischaemic heart. Biochem. Soc. Trans. 31, 207–212 (2003).
Kaushik, V. K. et al. Regulation of fatty acid oxidation and glucose metabolism in rat soleus muscle: effects of AICAR. Am. J. Physiol. Endocrinol. Metab. 281, E335–E340 (2001).
Abu-Elheiga, L., Oh, W., Kordari, P. & Wakil, S. J. Acetyl-CoA carboxylase 2 mutant mice are protected against obesity and diabetes induced by high-fat/high-carbohydrate diets. Proc. Natl Acad. Sci. USA 100, 10207–10212 (2003).
Gronwald, J. W. Herbicides inhibiting acetyl-CoA carboxylase. Biochem. Soc. Trans. 22, 616–621 (1994).
Seng, T. W., Skillman, T. R., Yang, N. Y. & Hammond, C. Cyclohexanedione herbicides are inhibitors of rat heart acetyl-CoA carboxylase. Bioorg. Med. Chem. Lett. 13, 3237–3242 (2003).
Arbeeny, C. M., Meyers, D. S., Bergquist, K. E. & Gregg, R. E. Inhibition of fatty acid synthesis decreases very low density lipoprotein secretion in the hamster. J. Lipid Res. 33, 843–851 (1992).
Harwood, H. J. Jr et al. Isozyme-nonselective N-substituted bipiperidylcarboxamide acetyl-CoA carboxylase inhibitors reduce tissue malonyl-CoA concentrations, inhibit fatty acid synthesis, and increase fatty acid oxidation in cultured cells and in experimental animals. J. Biol. Chem. 278, 37099–37111 (2003). This paper reports the development of isozyme-nonselective ACC inhibitors that are effective in inhibiting fatty-acid synthesis and enhancing lipid oxidation.
Zhang, H., Yang, Z., Shen, Y. & Tong, L. Crystal structure of the carboxyltransferase domain of acetyl-coenzyme A carboxylase. Science 299, 2064–2067 (2003).
Ntambi, J. M. & Miyazaki, M. Recent insights into stearoyl-CoA desaturase-1. Curr. Opin. Lipidol. 14, 255–261 (2003).
Miyazaki, M., Man, W. C. & Ntambi, J. M. Targeted disruption of stearoyl-CoA desaturase1 gene in mice causes atrophy of sebaceous and meibomian glands and depletion of wax esters in the eyelid. J. Nutr. 131, 2260–2268 (2001).
Cohen, P. et al. Role for stearoyl-CoA desaturase-1 in leptin-mediated weight loss. Science 297, 240–243 (2002).
Ntambi, J. M. et al. Loss of stearoyl-CoA desaturase-1 function protects mice against adiposity. Proc. Natl Acad. Sci. USA 99, 11482–11486 (2002).
Volpe, J. J. & Vagelos, P. R. Mechanisms and regulation of biosynthesis of saturated fatty acids. Physiol. Rev. 56, 339–417 (1976).
Ntambi, J. M. & Bene, H. Polyunsaturated fatty acid regulation of gene expression. J. Mol. Neurosci. 16, 273–278; discussion 279–284 (2001).
Miyazaki, M., Kim, Y. C. & Ntambi, J. M. A lipogenic diet in mice with a disruption of the stearoyl-CoA desaturase 1 gene reveals a stringent requirement of endogenous monounsaturated fatty acids for triglyceride synthesis. J. Lipid Res. 42, 1018–1024 (2001).
Obici, S., Feng, Z. H., Arduini, A., Conti, R. & Rossetti, L. Inhibition of hypothalamic carnitine palmitoyltransferase-1 decreases food intake and glucose production. Nature Med. 9, 756–761 (2003).
Ashrafi, K. et al. Genome-wide RNAi analysis of Caenorhabditis elegans fat regulatory genes. Nature 421, 268–272 (2003). This study shows the power of RNA interference in obesity-target identification.
Acknowledgements
The authors would like to apologize to all authors whose work could not be cited owing to space limitations.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Y.S. is employed by Eli Lilly and Co., and P.B. is employed by Bayer Healthcare.
Related links
Related links
DATABASES
Entrez Gene
OMIM
Swiss-Prot
FURTHER INFORMATION
Encyclopedia of Life Sciences
Glossary
- DYSLIPIDAEMIA
-
Disorders in lipoprotein metabolism, which are classified as hypercholesterolaemia, hypertriglyceridaemia, combined hyperlipidaemia and low levels of high-density lipoprotein (HDL) cholesterol.
- HYPERURICAEMIA
-
A build-up of uric acid (a by-product of metabolism) in the blood.
- ANOREXIGENIC
-
Causing loss of appetite.
- OREXIGENIC
-
Stimulating appetite.
- POSTPRANDIAL TRIGLYCERIDAEMIA
-
An abnormally high level of circulating triglycerides after eating.
- EMULSIFICATION
-
Increases the surface area of the oil–water interface, which promotes the breakdown of triglycerides by pancreatic lipase.
- OROSENSORY
-
Perception of taste and smell.
- GLYCAEMIC CONTROL
-
The regulation of blood glucose.
- STEATORRHOEA
-
An excessive amount of lipid in the faeces.
- CHYLOMICRON
-
A microscopic particle of triglyceride, cholesterol esters and apolipoproteins that is produced in the intestine and which functions as a transport vehicle.
- HYPERCHOLESTEROLAEMIA
-
The presence of an abnormal amount of cholesterol in the cells and plasma of the blood; this is associated with the risk of atherosclerosis.
- ABETALIPOPROTEINAEMIA
-
An autosomal recessive disorder of lipoprotein metabolism in which lipoproteins containing apolipoprotein B (chylomicrons, very-low-density lipoproteins and low-density lipoproteins) are not synthesized; the disorder is characterized by the presence of acanthocytes in plasma, hypocholesterolaemia, progressive ataxic neuropathy, pigmentary retinal degeneration, defective intestinal lipid absorption and deficiency of fat-soluble vitamins.
- LIPODYSTROPHY
-
A collection of rare conditions resulting from defective fat metabolism and characterized by atrophy of the subcutaneous fat.
- LIPOPAENIA
-
An abnormally small amount, or a deficiency, of lipids in the body.
- HYPERGLYCAEMIA
-
An abnormally high level of glucose in the blood; this occurs when the body does not have enough insulin (insulin deficiency) or cannot use the insulin that it does have (insulin resistance) to metabolize glucose.
- HYPERINSULINAEMIA
-
Excessively high insulin levels in the blood, which can be caused by hypersecretion of a β-cell tumour (insulinoma), autoantibodies against insulin, defective insulin receptor, or the overuse of exogenous insulin or hypoglycaemic agents.
- RESPIRATORY QUOTIENT
-
The ratio of the volume of carbon dioxide expired to the volume of oxygen consumed by an organism or cell over a given period of time.
- HYPOKETOTIC HYPOGLYCAEMIA
-
Low serum ketone concentrations accompanied by low blood glucose.
- HEPATOCARDIOMUSCULAR DISEASE
-
An inherited genetic disease caused by mutation of CPT2 and characterized by hypoketotic hypoglycaemia, liver failure, cardiomyopathy, and peripheral myopathy.
- HYPERAMMONAEMIA
-
A metabolic disorder that is characterized by an elevated level of ammonia in the blood.
- HYPERPHAGIA
-
The propensity to overeat.
Rights and permissions
About this article
Cite this article
Shi, Y., Burn, P. Lipid metabolic enzymes: emerging drug targets for the treatment of obesity. Nat Rev Drug Discov 3, 695–710 (2004). https://doi.org/10.1038/nrd1469
Issue Date:
DOI: https://doi.org/10.1038/nrd1469
This article is cited by
-
Body composition changes in patients with differentiated thyroid cancer after iodine-131 treatment and short-term levothyroxine replacement and suppression therapy
Hormones (2024)
-
Identification of promising multi-targeting inhibitors of obesity from Vernonia amygdalina through computational analysis
Molecular Diversity (2023)
-
Naringin promotes fat browning mediated by UCP1 activation via the AMPK signaling pathway in 3T3-L1 adipocytes
Archives of Pharmacal Research (2023)
-
Applications and perspectives of polyphenol-loaded solid lipid nanoparticles and nanostructured lipid carriers for foods
Food Science and Biotechnology (2022)
-
Fatty acid oxidation: driver of lymph node metastasis
Cancer Cell International (2021)