Key Points
-
Breast cancer treatment-related cardiovascular disease is an established effect, although its absolute incidence is low, and these risks must be balanced with the potential for cure
-
Receiving radiation therapy is a known risk factor for developing cardiovascular disease
-
The latency period to radiation-induced cardiovascular disease was once thought to be decades, but newer evidence suggests that it can manifest within several years after treatment
-
The specific portion of the heart and the actual dose it receives are paramount to the development of radiation-induced cardiovascular disease; various technical modifications can limit cardiac exposure to radiation
-
Numerous systemic therapies for breast cancer, such as anthracyclines and trastuzumab, are known to be cardiotoxic
-
Routinely used cardiovascular medications might be effective in the prevention of chemotherapy-related cardiac injury, and their use should be considered
Abstract
Breast cancer treatments have evolved over the past decades, although several widely used treatments have adverse cardiac effects. Radiotherapy generally improves the survival of women with breast cancer, although its deleterious cardiovascular effects pose competing risks of morbidity and/or mortality. In the past, radiation-associated cardiovascular disease was a phenomenon considered to take more than a decade to manifest, but newer research suggests that this latency is much shorter. Knowledge of coronary anatomy relative to the distribution of the delivered radiation dose has improved over time, and as a result, techniques have enabled this risk to be decreased. Studies continue to be performed to better understand, prevent and mitigate against radiation-associated cardiovascular disease. Treatments such as anthracyclines, which are a mainstay of chemotherapy for breast cancer, and newer targeted agents such as trastuzumab both have established risks of cardiotoxicity, which can limit their effectiveness and result in increased morbidity and/or mortality. Interest in whether β-blockers, statins and/or angiotensin-converting enzyme (ACE)-inhibitors might have therapeutic and/or preventative effects in these patients is currently increasing. This Review summarizes the incidence, risks and effects of treatment-induced cardiovascular disease in patients with breast cancer and describes strategies that might be used to minimize this risk.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Lee, M. S., Finch, W. & Mahmud, E. Cardiovascular complications of radiotherapy. Am. J. Cardiol. 112, 1688–1696 (2013).
Darby S. C. et al. Radiation-related heart disease: current knowledge and future prospects. Int. J. Radiat. Oncol. Biol. Phys. 76, 656–665 (2010).
Cuzick, J. et al. Overview of randomized trials of postoperative adjuvant radiation therapy in breast cancer. Cancer Treat. Rep. 71, 15–29 (1987).
Cuzick, J. et al. Cause-specific mortality in long-term survivors of breast cancer who participated in trials of radiotherapy. J. Clin. Oncol. 12, 447–453 (1994).
Host, H., Brennhovd, I. O. & Loeb, M. Postoperative radiotherapy in breast cancer—long-term results from the Oslo study. Int. J. Radiat. Oncol. Biol. Phys. 12, 727–732 (1986).
Haybittle, J. L., Brinkley, D., Houghton, J., A'Hern, R. P. & Baum, M. Postoperative radiotherapy and late mortality: evidence from the Cancer Research Campaign trial for early breast cancer. BMJ 298, 1611–1614 (1989).
Rutqvist, L. E., Lax, I., Fornander, T., A'Hern, R. P. & Baum, M. Cardiovascular mortality in a randomized trial of adjuvant radiation therapy versus surgery alone in primary breast cancer. Int. J. Radiat. Oncol. Biol. Phys. 22, 887–896 (1992).
Rutqvist, L. E. & Johansson, H. Mortality by laterality of the primary tumor among 55,000 breast cancer patients from the Swedish Cancer Registry. Br. J. Cancer 61, 866–868 (1990).
Hojris, I., Overgaard, M., Christensen, J. J. & Overgaard, J. Morbidity and mortality of ischemic heart disease in high-risk breast cancer patients after adjuvant postmastectomy systemic treatment with or without radiotherapy: Analysis of DBCG 82b and 82c randomized trials. Lancet 354, 1425–1430 (1999).
Harris, E. E. et al. Late cardiac mortality and morbidity in early-stage breast cancer patients after breast conservation treatment. J. Clin. Oncol. 24, 4100–4106 (2006).
Paszat, L. F. et al. A population-based case-cohort study of the risk of myocardial infarction following radiation therapy for breast cancer. Radiother. Oncol. 82, 294–300 (2007).
Correa, C. R. et al. Coronary artery findings after left-sided compared with right-sided radiation treatment for early-stage breast cancer. J. Clin. Oncol. 25, 3031–3037 (2007).
Hooning, M. J. Long-term risk of cardiovascular disease in 10-year survivors of breast cancer. J. Natl Cancer Inst. 99, 365–375 (2007).
Borger, J. H. et al. Cardiotoxic effects of tangential breast irradiation in early breast cancer patients: the role of irradiated heart volume. Int. J. Radiat. Oncol. Biol. Phys. 69, 1131–1138 (2007).
Cvancarova, M. et al. Risk of death from cardiovascular disease in long-term breast cancer survivors: a comparison with women from the general population [abstract]. J. Clin. Oncol. 32, S5 a1534 (2014).
Clarke, M. et al. Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: an overview of the randomised trials. Lancet 366, 2087–2106 (2005).
Janjan, N. A. et al. Dose to the cardiac vascular and conduction systems in primary breast irradiation. Med. Dosim. 14, 81–87 (1989).
Nieder, C., Schill, S., Kneschaurek, P. & Molls, M. Influence of different treatment techniques on radiation dose to the LAD coronary artery. Radiat. Oncol. 2, 20 (2007).
Taylor, C. W., Nisbet, A., McGale, P. & Darby, S. C. Cardiac exposures in breast cancer radiotherapy: 1950's–1990's. Int. J. Radiat. Oncol. Biol. Phys. 69, 1484–1495 (2007).
Taylor, C. W. et al. Cardiac dose from contemporary tangential breast cancer radiotherapy in the year 2006. Int. J. Radiat. Oncol. Biol. Phys. 72, 501–507 (2008).
Nilsson, G. et al. Distribution of coronary artery stenosis after radiation for breast cancer. J. Clin. Oncol. 30, 380–386 (2012).
Darby, S. C. et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N. Engl. J. Med. 368, 987–998 (2013).
Marks, L. B. et al. The incidence and functional consequences of RT-associated cardiac perfusion defects. Int. J. Radiat. Oncol. Biol. Phys. 63, 214–223 (2005).
Bell, L. . J. Cox, J., Eade, T. & Rinks, M. & Kneebone, A. The impact of rectal and bladder variability on target coverage during post-prostatectomy intensity modulated radiotherapy. Radiother. Oncol. 110, 245–250 (2014).
de Crevoisier, R. et al. Increased risk of biochemical and local failure in patients with distended rectum on the planning CT for prostate cancer radiotherapy. Int. J. Radiat. Biol. Oncol. Phys. 62, 965–973 (2005).
Heemsbergen, W. D. et al. Increased risk of biochemical and clinical failure for prostate patients with a large rectum at radiotherapy planning: results from the Dutch trial of 68Gy versus 78 Gy. Int. J. Radiat. Oncol. Biol. Phys. 67, 1418–1424 (2007).
Michalski, J. M. et al. Preliminary report of toxicity following 3D radiation therapy for prostate cancer on 3DOG/RTOG 9406. Int. J. Radiat. Oncol. Biol. Phys. 46, 391–402 (2000).
Gyenes, G., Fornander, T., Carlens, P., Glas, U. & Rutqvist, L. E. Myocardial damage in breast cancer patients treated with adjuvant radiotherapy: a prospective study. Int. J. Radiat. Oncol. Biol. Phys. 36, 899–905 (1996).
Prosnitz, R. G. et al. Prospective assessment of radiotherapy-associated cardiac toxicity in breast cancer patients: analysis of data 3 to 6 years after treatment. Cancer 110, 1840–1850 (2007).
Ishii, J. et al. Risk stratification using a combination of cardiac troponin T and brain natriuretic peptide in patients hospitalized for worsening chronic heart failure. Am. J. Cardiol. 89, 691–695 (2002).
Perna, E. R. et al. Ongoing myocardial injury in stable severe heart failure: value of cardiac troponin T monitoring for high-risk patient identification. Circulation 110, 2376–2382 (2004).
Nellessen, U. et al. Serial analysis of troponin I levels in patients with ischemic and nonischemic dilated cardiomyopathy. Clin. Cardiol. 29, 219–224 (2006).
Nellessen, U., Zingel, M., Hecker, H., Bahnsen, J. & Borschke, D. Effects of radiation therapy on myocardial cell integrity and pump function: which role for cardiac biomarkers? Chemotherapy 56, 147–152 (2010).
Hughes-Davies, L., Sacks, D., Rescigno, J., Howard, S. & Harris, J. Serum cardiac troponin T levels during treatment of early-stage breast cancer. J. Clin. Oncol. 13, 2582–2584 (1995).
Kozak, K. R. et al. Cardiac blood biomarkers in patients receiving thoracic (chemo)radiation. Lung Cancer 62, 351–355 (2008).
Cardinale, D., Salvatici, M. & Sandri, M. T. Role of biomarkers in cardioncology. Clin. Chem. Lab. Med. 49, 1937–1948 (2011).
Christenson, E. S., James, T., Agrawal, V. & Park, B. H. Use of biomarkers for the assessment of chemotherapy-induced cardiac toxicity. Clin. Biochem. 48, 223–235 (2015).
Hancock, S. L., Tucker, M. A. & Hoppe, R. T. Factors affecting late mortality from heart disease after treatment of Hodgkin's disease. J. Am. Med. Assoc. 270, 1949–1955 (1993).
Bradley, J. D. et al. Standard-dose versus high-dose conformal radiotherapy with concurrent and consolidation carboplatin plus paclitaxel with or without cetuximab for patients with stage IIIA or IIIB non-small-cell lung cancer (RTOG 0617): a randomised, two-by-two factorial phase 3 study. Lancet Oncol. 16, 187–199 (2015).
Hardy, D., Liu, C. C., Cormier, J. N., Xia, R. & Du, X. L. Cardiac toxicity in association with chemotherapy and radiation therapy in a large cohort of older patients with non-small-cell lung cancer. Ann. Oncol. 21, 1825–1833 (2010).
Wilson, P. W. et al. Prediction of coronary heart disease using risk factor categories. Circulation 97, 1837–1847 (1998).
Grundy, S. M., Pasternak, R., Greenland, P., Smith, S. Jr & Fuster, V. AHA/ACC scientific statement: Assessment of cardiovascular risk by use of multiple-risk-factor assessment equations: a statement for healthcare professionals from the American Heart Association and the American College of Cardiology. J. Am. Coll. Cardiol. 34, 1348–1359 (1999).
Ridker, P. M., Buring, J. E., Rifai, N. & Cook, N. R. Development and validation of improved algorithms for the assessment of global cardiovascular risk in women: The Reynolds score. J. Am. Med. Assoc. 297, 611–619 (2007).
Paszat, L. F., Mackillop, W. J., Groome, P. A., Schulze, K. & Holowaty, E. Mortality from myocardial infarction following postlumpectomy radiotherapy for breast cancer: A population-based study in Ontario, Canada. Int. J. Radiat. Oncol. Biol. Phys. 43, 755–761 (1999).
Hooning, M. J. et al. Cause-specific mortality in long-term survivors of breast cancer: A 25-year follow-up study. Int. J. Radiat. Oncol. Biol. Phys. 64, 1081–1091 (2007).
Brenner, D. J., Shuryak, I., Jozsef, G., Dewyngaert, K. J. & Formenti, S. C. Risk and risk reduction of major coronary events associated with contemporary breast radiotherapy. JAMA Intern. Med. 174, 158–160 (2014).
Suter, T. M. & Ewer, M. S. Cancer drugs and the heart: importance and management. Eur. Heart J. 34, 1102–1111 (2013).
Lenihan D. J. & Cardinale, D. Late cardiac effects of cancer treatment. J. Clin. Oncol. 30, 3657–3664 (2012).
Jessup, M. et al. 2009 focused update: ACCF/AHA guidelines for the diagnosis and management of heart failure in adults: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. J. Am. Coll. Cardiol. 53, 1343–1382 (2009).
Hahn, V. S., Lenihan, D. J. & Ky, B. Cancer therapy-induced cardiotoxicity: basic mechanisms and potential cardioprotective therapies. J. Am. Heart Assoc. 3, e000665 (2014).
Zhang, S. et al. Identification of the molecular basis of doxorubicin-induced cardiotoxicity. Nat. Med. 18, 1639–1642 (2012).
Yeh, E. T. & Bickford, C. L. Cardiovascular complications of cancer therapy. Incidence, pathogenesis, diagnosis, and management. J. Am. Coll. Cardiol. 53, 2231–2247 (2009).
Jones, L. W., Haykowsky, M. J., Swartz, J. J., Douglas, P. S. & Mackey, J. R. Early breast cancer therapy and cardiovascular injury. J. Am. Coll. Cardiol. 50, 1435–1441 (2007).
Von Hoff, D. D. et al. Risk factors for doxorubicin-induced congestive heart failure. Ann. Intern. Med. 91, 710–717 (1979).
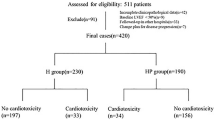
Bowles, E. J. et al. Pharmacovigilance Study Team. Risk of heart failure in breast cancer patients after anthracycline and trastuzumab treatment: a retrospective cohort study. J. Natl Cancer Inst. 104, 1293–1305, (2012).
Carver, J. R., Szalda, D. & Ky, B. Asymptomatic cardiac toxicity in long-term cancer survivors: defining the population and recommendations for surveillance. Semin. Oncol. 40, 229–238 (2013).
Crone, S. A. et al. ErbB2 is essential in the prevention of dilated cardiomyopathy. Nat. Med. 8, 459–465 (2002).
Lee, K. F. et al. Requirement for neuregulin receptor erbB2 in neural and cardiac development Nature 378, 394–398 (1995).
Harbeck, N., Ewer, M. S., De Laurentiis, M., Suter, T. M. & Ewer, S. M. Cardiovascular complications of conventional and targeted adjuvant breast cancer therapy. Ann. Oncol. 22, 1250–1258 (2011).
Ewer, S. M. & Ewer, M. S. Carditoxicity profile of trastuzumab. Drug Saf. 31, 459–467 (2008).
Halyard, M. Y. et al. Radiotherapy and adjuvant trastuzumab in operable breast cancer: tolerability and adverse event data from the NCCTG phase III trial N9831. J. Clin. Oncol. 27, 2638–2644 (2009).
Shapiro, C. L. et al. Cardiac effects of adjuvant doxorubicin and radiation therapy in breast cancer patients. J. Clin. Oncol. 16, 3493–3501 (1998).
Valagussa, P. et al. Cardiac effects following adjuvant chemotherapy and breast irradiation in operable breast cancer. Ann. Oncol. 5, 209–216 (1994).
Cardinale, D., Bacchiani, G., Beggiato, M., Colombo, A. & Cipolla. C. M. Strategies to prevent and treat cardiovascular risk in cancer patients. Semin. Oncol. 40, 186–198 (2013).
Thavendiranathan, P. et al. Use of myocardial strain imaging by echocardiography for the early detection of cardiotoxicity in patients during and after cancer chemotherapy: a systematic review. J. Am. Coll. Cardiol. 63, 2751–2768 (2014).
Tamene, A. M., Masri, C. & Konety, S. H. Cardiovascular MR imaging in cardio-oncology. Magn. Reson. Imaging Clin. N. Am. 23, 105–116 (2015).
Cardinale, D. et al. Anthracycline-induced cardiomyopathy: clinical relevance and response to pharmacologic therapy. J. Am. Coll. Cardiol. 55, 213–220 (2010).
Curigliano, G. et al. Cardiovascular toxicity induced by chemotherapy, targeted agents and radiotherapy: ESMO Clinical Practice Guidelines. Ann. Oncol. 23, S55–S66 (2012).
Telli, M. L., Hunt, S. A., Carlson, R. W. & Guardino, A. E. Trastuzumab-related cardiotoxicity: calling into question the concept of reversibility. J. Clin. Oncol. 25, 3525–3533 (2007).
Tocchetti . et al. Detection, monitoring, and management of trastuzumab-induced left ventricular dysfunction: an actual challenge. Eur. J. Heart Fail. 14, 130–137 (2012).
Mackey, J. R. et al. Cardiac management during adjuvant trastuzumab therapy: recommendations of the Canadian Trastuzumab Working Group. Curr. Oncol. 15, 24–35 (2008).
Sengupta, P. P., Northfelt, D. W., Gentile, F., Zamorano, J. L. & Khandheria, B. K. Trastuzumab-induced cardiotoxicity: heart failure at the crossroads. Mayo Clin. Proc. 83, 197–203 (2008).
Jones, A. L. et al. Management of cardiac health in trastuzumab-treated patients with breast cancer: updated United Kingdom National Cancer Research Institute recommendations for monitoring. Br. J. Cancer 100, 684–692 (2009).
Martin, M. et al. Minimizing cardiotoxicity while optimizing treatment efficacy with trastuzumab: review and expert recommendations. Oncologist 14, 1–11 (2009).
Fyles, A. W. et al. Tamoxifen with or without breast irradiation in women 50 years of age or older with early breast cancer. N. Engl. J. Med. 351, 963–970 (2004).
Hughes, K. S. et al. Lumpectomy plus tamoxifen with or without irradiation in women age 70 years or older with early breast cancer: long-term follow-up of CALGB 9343. J. Clin. Oncol. 31, 2382–2387 (2013).
Fisher, B. et al. Prevention of invasive breast cancer in women with ductal carcinoma in situ: an update of the National Surgical Adjuvant Breast and Bowel Project experience. Semin. Oncol. 28, 400–418 (2001).
Houghton, J. et al. Radiotherapy and tamoxifen in women with completely excised ductal carcinoma in situ of the breast in the UK, Australia, and New Zealand: randomised controlled trial. Lancet 362, 95–102 (2003).
Bijker, N. et al. Breast-conserving treatment with or without radiotherapy in ductal carcinoma-in-situ: ten-year results of European Organisation for Research and Treatment of Cancer randomized phase III trial 10853--a study by the EORTC Breast Cancer Cooperative Group and EORTC Radiotherapy Group. J. Clin. Oncol. 24, 3381–3387 (2006).
Holmberg, L. et al. Absolute risk reductions for local recurrence after postoperative radiotherapy after sector resection for ductal carcinoma in situ of the breast. J. Clin. Oncol. 26, 1247–1252 (2008).
Paik, S. et al. A multigene assay to predict recurrence of tamoxifen-treated, node-negative breast cancer. N. Engl. J. Med. 351, 2817–2826 (2004).
Dragun, A. E. et al. Increasing mastectomy rates among all age groups for early stage breast cancer: a 10-year study of surgical choice. Breast J. 18, 318–325 (2012).
Fisher, C. S. et al. Fear of recurrence and perceived survival benefit are primary motivators for choosing mastectomy over breast-conservation therapy regardless of age. Ann. Surg. Oncol. 19, 3246–3250 (2012).
Mahmood, U. et al. Increasing national mastectomy rates for the treatment of early stage breast cancer. Ann. Surg. Oncol. 20, 1436–1443 (2013).
Wang, X. et al. Cardiac motion during deep-inspiration breath-hold: implications for breast cancer radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 82, 708–714 (2012).
Bruzzaniti, V. et al. Dosimetric and clinical advantages of deep inspiration breath-hold (DIBH) during radiotherapy of breast cancer. J. Exp. Clin. Cancer Res. 32, 88 (2013).
Tang, X. et al. Clinical experience with 3-dimensional surface matching-based deep inspiration breath hold for left-sided breast cancer radiation therapy. Pract. Radiat. Oncol. 4, e151–e158 (2014).
Zagar, T. M. et al. Prospective assessment of deep inspiration breath hold to prevent radiation associated cardiac perfusion defects in patients with left-sided breast cancer [abstract 2027]. Presented at the ASTRO Annual meeting, San Antonio, TX (2015).
Zellars, R. et al. SPECT analysis of cardiac perfusion changes after whole-breast/chest wall radiation therapy with or without active breathing coordinator: results of a randomized phase 3 trial. Int. J. Radiat. Oncol. Biol. Phys. 15, 778–785 (2014).
Formenti, S. C., DeWyngaert, J. K., Jozsef, G. & Goldberg, J. D. Prone vs supine positioning for breast cancer radiotherapy. JAMA 308, 861–863 (2012).
Chino, J. P. & Marks, L. B. Prone positioning causes the heart to be displaced anteriorly within the thorax: implications for breast cancer treatment. Int. J. Radiat. Oncol. Biol. Phys. 70, 916–920 (2008).
Würschmidt, F., Stoltenberg, S., Kretschmer, M. & Petersen, C. Incidental dose to coronary arteries is higher in prone than in supine whole breast irradiation. A dosimetric comparison in adjuvant radiotherapy of early stage breast cancer. Strahlenther Onkol. 190, 563–568 (2014).
Mulliez, T. et al. Heart dose reduction by prone deep inspiration breath hold in left-sided breast irradiation. Radiother. Oncol. 114, 79–84 (2015).
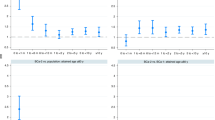
Kalay, N. et al. Protective effects of carvedilol against anthracycline-induced cardiomyopathy. J. Am. Coll. Cardiol. 48, 2258–2262 (2006).
Kaya, M. G. et al. Protective effects of nebivolol against anthracycline-induced cardiomyopathy: a randomized control study. Int. J. Cardiol. 167, 2306–2310 (2013).
Seicean, S. et al. Cardioprotective effect of β-adrenoceptor blockade in patients with breast cancer undergoing chemotherapy: follow-up study of heart failure. Circ. Heart Fail. 6, 420–426 (2013).
Nakamae, H. et al. Notable effects of angiotensin II receptor blocker, valsartan, on acute cardiotoxic changes after standard chemotherapy with cyclophosphamide, doxorubicin, vincristine, and prednisolone. Cancer 104, 2492–2498 (2005).
Cadeddu, C. et al. Protective effects of the angiotensin II receptor blocker telmisartan on epirubicin-induced inflammation, oxidative stress, and early ventricular impairment. Am. Heart J. 160, e1–e7 (2010).
Cardinale, D. et al. Prevention of high-dose chemotherapy-induced cardiotoxicity in high-risk patients by angiotensin-converting enzyme inhibition. Circulation 114, 2474–2481 (2006).
Bosch, X. et al. Enalapril and carvedilol for preventing chemotherapy-induced left ventricular systolic dysfunction in patients with malignant hemopathies: the OVERCOME trial (preventiOn of left Ventricular dysfunction with Enalapril and caRvedilol in patients submitted to intensive ChemOtherapy for the treatment of Malignant hEmopathies). J. Am. Coll. Cardiol. 61, 2355–2362 (2013).
Kalam, K. & Marwick, T. H. Role of cardioprotective therapy for prevention of cardiotoxicity with chemotherapy: a systematic review and meta-analysis. Eur. J. Cancer 49, 2900–2909 (2013).
Seicean, S., Seicean, A., Plana, J. C., Budd, G. T. & Marwick, T. H. Effect of statin therapy on the risk for incident heart failure in patients with breast cancer receiving anthracycline chemotherapy: an observational clinical cohort study. J. Am. Coll. Cardiol. 60, 2384–2390 (2012).
Acar, Z. et al. Efficiency of atorvastatin in the protection of anthracycline-induced cardiomyopathy. J. Am. Coll. Cardiol. 58, 988–989 (2011).
US National Library of Medicine. ClinicalTrials.gov [online], (2015).
Truong, J., Yan, A. T., Cramarossa, G. & Chan, K. K. Chemotherapy-induced cardiotoxicity: detection, prevention and management. Can. J. Cardiol. 30, 869–878 (2014).
Acknowledgements
We thank Sarah Darby for her thoughtful review and advice for our manuscript.
Author information
Authors and Affiliations
Contributions
All authors researched data for the article, provided substantial contributions to discussions of its content, wrote the article and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Zagar, T., Cardinale, D. & Marks, L. Breast cancer therapy-associated cardiovascular disease. Nat Rev Clin Oncol 13, 172–184 (2016). https://doi.org/10.1038/nrclinonc.2015.171
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrclinonc.2015.171
This article is cited by
-
Heart Failure in the Elderly: the Role of Biological and Sociocultural Aspects Related to Sex
Current Heart Failure Reports (2023)
-
Genome wide CRISPR/Cas9 screen identifies the coagulation factor IX (F9) as a regulator of senescence
Cell Death & Disease (2022)
-
UACA locus is associated with breast cancer chemoresistance and survival
npj Breast Cancer (2022)
-
Coronary heart disease and mortality following a breast cancer diagnosis
BMC Medical Informatics and Decision Making (2020)
-
How breast cancer treatments affect the quality of life of women with non-metastatic breast cancer one year after surgical treatment: a cross-sectional study in Greece
BMC Surgery (2020)