Abstract
Human papillomavirus (HPV) is the most common sexually transmitted infectious agent; its 14 oncogenic types are causally associated with 5–10% of all cancers. The major structural HPV protein self-assembles into immunogenic virus-like particles. Two licensed HPV vaccines—the bivalent vaccine comprising HPV types 16 and 18, and the quadrivalent vaccine comprising HPV types 6, 11, 16 and 18—have proven to be safe and efficacious against 6-month-persistent cervical infections of HPV16 and HPV18 and associated precancerous lesions, and both have efficacies of 90–100%. Among baseline HPV-negative adolescent females, vaccine efficacies against the immediate precursor of cervical cancer (intraepithelial neoplasia grade 3) irrespective of HPV type are 93.2% and 43.0% for the bivalent and quadrivalent vaccines, respectively. The quadrivalent vaccine is efficacious (>75% vaccine efficacy) against any of the more-severe precursors of vulval, vaginal and anal cancers. A strong increase in vaccine efficacy with increasing severity of the precancerous lesion is explained by accumulation of the most-oncogenic HPV types 16 and 18 in these lesions. Therefore, prophylactic HPV vaccination will exceed the best results from screening for cancer. With the extremely efficacious prophylactic HPV vaccines, the focus of organized intervention (vaccination and screening) programmes should, however, shift from reducing the HPV disease burden to controlling the prevalence of oncogenic HPV (and nononcogenic HPV) types. Eradication of the major oncogenic HPV types should be pursued.
Key Points
-
Bivalent and quadrivalent human papillomavirus (HPV) vaccines are available that are highly efficacious against persistent vaccine-type HPV infections and associated intraepithelial neoplasias
-
Efficacy against external HPV6-associated and HPV11-associated genital lesions in females and males has been documented only for the quadrivalent vaccine
-
The quadrivalent HPV vaccine protects against nonvaccine HPV type 31; cross-protective efficacy of the bivalent vaccine extends to HPV types 31, 33, 45 and 51
-
The overall efficacy of the bivalent vaccine against cervical intraepithelial neoplasia grade 3 may be better than that of the quadrivalent vaccine
-
The increased importance of vaccinating both girls and boys is underlined by the mostly low coverage of national, girls-only vaccination programmes
Similar content being viewed by others
Introduction
Human papillomavirus (HPV) causes approximately 5% of all cancers in men, and 10% of all cancers in women—most notably anogenital and oropharyngeal cancers.1 HPVs are also the cause of the highly prevalent external genital warts. Vaccines have been developed against various types of the virus, with the aim of reducing associated cancer burdens and the additional effect of preventing genital warts. The bivalent (targeting HPV16 and HPV18) and the quadrivalent (HPV6, HPV11, HPV16 and HPV18) virus-like-particle vaccines are safe, and highly immunogenic.2,3,4,5 In this Review article, we compare the efficacy of the bivalent and quadrivalent vaccines in terms of infection and lesional end points (mostly intraepithelial neoplasias). We also discuss the methods used to verify the effectiveness of HPV vaccination.
HPV infections and immune response
Genital HPV infections are rapidly acquired after sexual debut, with about half of young women and men becoming infected in 3 years.6,7,8 HPV prevalences increase almost linearly with increasing number of life-time sexual partners,9,10 despite condom use and circumcision being partially protective against transmission.11,12 Following a microtrauma, the virus can establish infection in epithelial basal cells, with replication of HPV occurring as the infected cells differentiate.13 Intact virions are released when the productively infected cells are exfoliated. These virions can establish secondary foci of infection on the host mucosa or skin and be transmitted in sexual contact that occurs in the weeks and months after initiation of the infection.14
Approximately 40 different HPV types are known to infect the anogenital tract, and are divided into low-risk and high-risk types according to their oncogenic potential. The most prevalent low-risk HPV types HPV6 and HPV11 belong to clade A10.1 Twelve HPV types are established as carcinogenic to man by the International Agency for Research on Cancer (IARC): HPV16, HPV31, HPV33, HPV35, HPV52 and HPV58 belonging to clade A9; HPV18, HPV39, HPV45 and HPV59 belonging to clade A7; HPV56 belonging to clade A6; and HPV51 belonging to clade A5.1 The cumulative prevalence of these 12 high-risk HPV types in cervical cancer exceeds 100 percent, because a variable proportion of cervical cancer specimens contain multiple types.15 In addition to the 12 high-risk types, HPV68 is classified as probably carcinogenic and HPV66 was originally, but is no longer, classified as a carcinogen.16 However, new data is emerging on the biological action of these viruses17 and evaluation of vaccine efficacy to an even wider variety of high-risk HPV types (HPV66, for example) might be warranted. Furthermore, the prevalence of HPV types 18 and 45—which infect columnar epithelial cells as well as squamous cells—might, over time, have increased in countries with organized cervical screening,18 which effectively removes precursor lesions of squamous cell origin.
In the infected epithelium, the virally encoded proteins are recognized by epithelial antigen-presenting cells (APCs, known as Langerhans cells) and by antibody-producing B cells.19 The interaction between the APCs and T cells restricts the infection to the primary focus (mediated by cytotoxic T cells), and enhances the HPV antibody response by T helper (TH) cells. Although the cell-mediated response becomes detectable within weeks and the antibody response within months after infection,14 some individuals with HPV infection do not produce any detectable antibodies against the virus.20 The antibody response after an HPV16 infection is likely to be protective against reinfection in a notable proportion (up to 50%) of infected women,21 but reinfections might occur.14,22 Consequently, HPV vaccination of women who have infection-induced HPV antibodies significantly improves their protection against new HPV infections and HPV-associated lesions.23
Up to 90% of HPV infections clear spontaneously.14 Low-risk HPV infections clear in about 4 months,1 whereas high-risk HPV types seem to cluster in three groups depending on average clearance time (Figure 1), with HPV16 being slow (18–23 months), HPV18, HPV31, HPV33 and HPV52 taking a moderate clearance time (12–18 months) and the other confirmed high-risk HPV types having fast clearance (6–7 months).24,25
Data consist of type-specific frequencies for incident infections, 6-month persistent infections and 12-month persistent infections. The frequencies correspond to a 48-month follow-up duration (testing every 6 months).25 The posterior distributions were computed for each type, and based on these distributions the clade A7 and A9 high-risk HPV types were grouped into slowly (HPV16, red), moderately (HPV18, 31, 33 and 52, orange), and rapidly (HPV35, 39, 45, 59 and 68, blue) clearing infections. Abbreviation: HPV, human papillomavirus. Permission obtained from S. Vänskä, Rolf Nevanlinna Institute, University of Helsinki, Finland.
High-risk HPV infection is a necessary factor in cervical carcinogenesis. Smoking and Chlamydia trachomatis infection are frequent (occurring in 5–35% of young women), significant co-factors that modestly increase the risk of carcinogenesis.26,27,28,29 Concomitant C. trachomatis infection obtained at about the same time as a high-risk HPV infection can considerably (up to 30-fold) increase the relative risk of developing cervical intraepithelial neoplasia grade 3 (CIN3) compared with past C. trachomatis and HPV18 or HPV45 infections,30 possibly by prolonging the duration of the HPV infection.31,32 Smoking (and associated sexual risk-taking behaviours) acts on several levels, by increasing the likelihood of acquiring genital HPV infections,33 weakening the immune response to HPV34 and impairing the healing of HPV-associated cervical lesions.35
Up to 50% of young women who have acquired a genital HPV infection will acquire at least one other infection with a different HPV type within a few years.36,37,38,39,40,41,42,43,44 The risk of acquiring another high-risk HPV infection for a high-risk-HPV-positive woman is threefold to sixfold higher than for a woman with no detectable antibodies against high-risk HPV types.37,38,39,40 The clustering of multiple HPV types in the same individual seems to be independent of host or viral factors, but rather caused by a common risk determinant of exposure, presumably risk-taking sexual behaviour.38,41,42 Compared with single high-risk HPV infections, infections with multiple high-risk HPV types have been suggested to be associated with an increased risk of high-grade squamous intraepithelial lesions.24,36,43,44
HPV vaccine immunogenicity
The two licensed, prophylactic HPV vaccines both comprise DNA-free virus-like particles (VLP), which are produced by expressing the major structural L1 gene of HPV types 6, 11, 16 and 18 in yeast (Gardasil®; Merck, Whitehouse Station, USA) or the L1 genes of HPV types 16 and 18 in insect cells (Cervarix®; GlaxoSmithKline, London, UK). Once expressed, the corresponding L1 proteins spontaneously assemble into noninfectious VLPs, which are remarkably immunogenic. After three doses of the vaccine (the second dose 1–2 months after the first, and the third dose 6 months after the first), the antibody response is orders of magnitude higher than after a natural infection and has been detectable in all vaccinated participants in sizeable phase III studies.2,4
Although the HPV VLPs are immunogenic, adjuvant agents (aluminiumhydroxy-diphoshosulfate in Gardasil® and aluminiumhydroxide supplemented with monophosphorylipid AS04 in Cervarix®) are used to enhance the antibody response.45 The aluminium derivatives enable APCs to stimulate TH cells to migrate to the injection site.46 TH2 cytokine response promotes antibody production,47 the maturation of which is enhanced by the adjuvant aluminates.48 The monophosphoryl lipid AS04 also promotes antibody production and generation of memory B cells.45
The VLP-induced antibody response is age-dependent; in children <15 years of age, both the licensed vaccines induce higher antibody responses than in those >15 years.49,50 Gender, combination of the HPV vaccines with other vaccines or smoking (in spite of its probable role in deteriorating immune surveillance of natural HPV infection) do not seem to have any major effects on the vaccine-induced antibody response.51,52,53,54,55 However, because sterilizing immunity is not achievable, the C. trachomatis-induced potential immune-perturbation effect of concomitant infection with HPV18 and HPV45 in cervical carcinogenesis30 versus vaccine-induced immune protection against HPV challenge (especially with HPV18 and HPV45) warrants investigation.
A month after the third dose, the vaccine-induced antibody levels are up to 100 times higher than the antibody levels induced by natural HPV infection.56,57 Antibody levels induced by the bivalent vaccine remain very high for up to 8.4 years;57 by contrast, the HPV18 L1 antibody levels induced by the quadrivalent vaccine decreased over 3–5 years to the level of natural infection induced HPV18 antibodies,58 even if most vaccinees had neutralizing antibodies 48 months after vaccination.59 However, one booster dose 5 years after initial vaccination readily provoked an efficient secondary response, and the ensuing HPV6, HPV11, HPV16 and HPV18 antibody levels were higher than after the initial three-dose immunization.58 Interestingly, women whose epitope-specific antibody levels had declined below the limits of detection still continued to be protected against HPV infection and associated lesions,60,61 suggesting that protective antibodies are not directed against a single epitope and/or that the lowest level of HPV-vaccine-induced antibodies required for protection might be even lower than the detection limit of current HPV serology assays. This finding is especially important because pseudovirion-based determination of neutralizing antibody levels for the clade A7 and A9 nonvaccine HPV types (HPV31, HPV33 and HPV45—against which the bivalent vaccine shows constant protective efficacy) are <1% of the extremely high levels of the corresponding vaccine-induced HPV16 and HPV18 antibody levels.62
In women, the mucosal immunity induced by the HPV VLP vaccines is mediated by serum antibodies leaking into the mucosal surfaces.63 Higher levels of neutralizing antibodies following vaccination might be evident with the bivalent vaccine than with the quadrivalent vaccine, but no significant differences in the mucosal antibody levels induced by the two vaccines were observed using ELISA.61 Mucosal antibodies are detectable 4 years after HPV16 and HPV18 vaccination in two-thirds of vaccine recipients.63 Notably, in individuals without detectable mucosal antibodies, serum antibody levels after three-dose immunization with the bivalent vaccine were continuously significantly lower than in women with detectable mucosal antibodies, possibly due to too-low amounts of exudated antibodies.63 However, at the site of the initial infection or associated microtrauma, even low (that is, undetectable) levels of serum antibodies can probably offer protection against infection.
Genital HPV infections
HPV infections are usually asymptomatic and need laboratory assays (such as PCR-based DNA detection assays) for detection. However, the detection of HPV DNA in a single laboratory assay cannot be considered proof of infection, as it can also represent environmental contamination. In fact, HPV DNA-based screening tests are designed to have a cut-off level that preferentially detects infection—because exposures that do not result in an infection are typically present as low HPV DNA levels—rather than contamination.64 That is, the cut-off values are considerably higher than for most other DNA assays. In HPV vaccinology, infection is defined as HPV DNA that has been continuously present in multiple sampling occasions (persistent positivity), usually over a 6-month period.2,4 Using 6-month HPV DNA persistence as an end point, vaccine efficacy data is available for the two licensed vaccines (Table 1 and Supplementary Table 1 online).
In baseline HPV PCR-negative (HPV6, HPV11, HPV16 and HPV18 negative for the quadrivalent vaccine and HPV16 and HPV18 negative for the bivalent vaccine) women, vaccine efficacies against 6-month persistent infections with HPV16 and HPV18 are 90–100%, and are indistinguishable between the vaccines (Table 1). The efficacies of the two vaccines against persistent HPV6 and HPV11 infections differ considerably in individuals who are PCR negative at baseline (Table 1). However, the bivalent vaccine—which does not specifically target HPV6 and HPV11—has a low (34.5%) but statistically significant efficacy against persistent infection with these virus types, presumably caused by cross-protection from the vaccine.65 The vaccine efficacy against 12-month persistent infection with the types covered by the vaccines is similar to the vaccine efficacy against 6-month persistent infection.3,5
Comparison of the vaccine against the other major nonvaccine high-risk HPV types (using the 6-month persistence definition) showed that, among baseline HPV PCR-negative women (for the HPV vaccine types), the two approved vaccines were not significantly different against HPV31 (64.7–77.1% and 46.2%) and HPV33 (32.1–43.1% and 28.7%) in terms of efficacy (overlapping 95% CI; Table 1 and Supplementary Table 1 online). Both vaccines had a similar, low efficacy against HPV52 (18.9–19.6% and 18.4%; Table 1), suggesting a relatively wide cross-protection for HPV types within clade A9. Cross-protection against HPV35 is ambiguous and HPV58 is the only clade-A9 virus that is definitely not protected against with current vaccines. Cross-protection in clade A7—presumably induced by the HPV18 component in the vaccine—was only observed with the bivalent vaccine, which had a vaccine efficacy against HPV45 of 73.0–79.0% (Table 1); the quadrivalent vaccine had no significant vaccine efficacy against HPV45 (7.8%). The bivalent vaccine had no significant vaccine efficacy against HPV types 39, 59 and 68, and the quadrivalent vaccine had no significant vaccine efficacy against HPV59. In the intention-to-treat analyses, the vaccine efficacy estimates were similarly low for both the vaccine types HPV16 and HPV18 and the cross-protected HPV types 31, 33 and 45 (Supplementary Table 1 online).
External genital lesions
Vaccine efficacies against cytological end points have not been consistently reported and—for external genital lesions (EGLs)—have only been reported for the quadrivalent vaccine (Table 2). Regardless of HPV type, the quadrivalent vaccine efficacy against EGLs has been estimated to be high to very high among those who are baseline HPV-negative, both for females and males.5,66 Very high vaccine efficacies for EGLs are associated with HPV16 and HPV18 (94% and 100% for women, and 100% and 100% for men associated with HPV16 and HPV18, respectively). Although the efficacies of the vaccines in males against EGLs associated with HPV types 6 and 11, and HPV 16 and 18 were also high, they were lower than the corresponding HPV-specific vaccine efficacies for females (Table 2). The individuals who were seropositive for HIV in the male study population could not have contributed to the lower vaccine efficacy in males because these individuals were excluded from pertinent analyses. Furthermore, immunogenicity of the quadrivalent vaccine has been adequate in HIV-positive males.67 In vaccinated individuals, breakthrough EGLs that are positive for the HPV types covered by the vaccines are rare. In the few reported cases, concomitant (multiple) infections with other, nonvaccine HPV types have been found, which suggests that the EGLs could have been caused by the concomitant nonvaccine HPV type.5
Precursors of anogenital cancers
As expected, the high vaccine efficacies against HPV infection and benign HPV-induced lesions are translating to high vaccine efficacies against the precursors of anogenital cancers that are caused by these infections. Importantly, the vaccine efficacy estimates tend to increase as the severity of the cervical, vulvar, vaginal or anal lesions increase, for both vaccines (Tables 3, 4, 5).
Cervical intraepithelial neoplasia
Results from the two phase III trials on the vaccine efficacy (irrespective of HPV type) of the quadrivalent and bivalent vaccines (FUTURE I and II and PATRICIA, respectively) that assessed the incidence of CIN1 lesions (mild dysplasia) have been 29.7%5 and 50.3%3 among baseline HPV-negative participants, and 20.3%5 and 27.7%3 among all participants in intention-to-treat analyses. The vaccine efficacies against CIN1 associated with HPV types 6, 11, 16 and 18, and HPV types 16 and 18 were remarkably similar: 97.2%68 and 96.5%3 among baseline HPV-negative participants, and 67.5%68 and 62.9%3 in the intention-to-treat analyses (Table 3).
The detection of CIN2 or CIN3 lesion (CIN2, CIN2+, CIN3 and CIN3+) has been the most important end point of the phase III HPV vaccine efficacy trials. For ethical reasons, follow up without treatment is not possible for participants who have CIN2. Although CIN3 develops from CIN2 lesions, the CIN3 lesions documented in the trials presumably arise from extraordinarily rapid development between study visits. Although CIN2 is a clinically important trial end point, it is hampered by subjective assessment with poor reproducibility69 and high likelihood of spontaneous regression.70 Distinguishing lesions that would have progressed or regressed if left untreated is impossible; thus, whether the vaccines are equally efficacious against both types of lesions is unclear. Furthermore, the two large-scale phase III trials differ in the inclusion of baseline HPV seronegative women: negative for all vaccine HPV types (HPV6, HPV11, HPV16 and HPV18 in the FUTURE study)4,5 or negative for all HPV types (in the PATRICIA trial).2,3 These caveats should be kept in mind when considering the vaccine efficacy estimates.
The phase III trials of both vaccines have reported vaccine efficacies against CIN2+, CIN3 and adenocarcinoma in situ (AIS) after 3–4 years of follow-up monitoring: 19.3%, 16.4% and 60% (for the quadrivalent vaccine),68,71, and 33.1%, 45.6% and 76.9% (for the bivalent vaccine),3 respectively, in intention-to-treat analyses (Table 3). In baseline HPV PCR-negative participants, the vaccine efficacy against CIN2+ and CIN3+ were 42.7% and 43.0%68, and 64.9% and 93.2%,3 for the quadrivalent and bivalent vaccines, respectively. Importantly, vaccine efficacies against CIN2+, CIN3+ and AIS associated with HPV16 and HPV18 were 100%, 97.2% and 100% (quadrivalent vaccine),68,71 and 99.0%, 100% and 100% (bivalent vaccine)3 among baseline HPV-negative participants.
A statistically significant difference between the two vaccines in their efficacy against any CIN3 has been shown (93.2% versus 43.0% for the bivalent and quadrivalent vaccines; Table 3). However, a proof-of-principle study using cancer-registry-based follow-up data of the quadrivalent vaccine has found a 100% (albeit insignificant) vaccine efficacy against CIN3+.72 Surveillance of early vaccination programmes is also providing evidence of the overall reduction of high-grade cervical dysplasia following quadrivalent HPV vaccination.73 The cancer-registry follow-up data covers a period of 5–10 years after vaccination or enrolment; thus, most of the identified CIN3 lesions have probably been caused by HPV16, the most prevalent and oncogenic HPV type.1 In the foreseeable future, however, sizeable Nordic phase III trial cohorts will provide population-based data on vaccine efficacies against CIN3+ and invasive cervical cancer for both the licensed HPV vaccines.74
Vulvar and vaginal intraepithelial neoplasia
Vaccine efficacies against precursors of vulvar or vaginal cancers (vulvar intraepithelial neoplasia [VIN] and vaginal intraepithelial neoplasia [VAIN]) have been reported only for the quadrivalent vaccine,68 because appropriate samples in these anatomical sites were not collected in the major efficacy trial of the bivalent vaccine. Efficacies against VIN1 or VAIN1 lesions were extremely good in participants who were negative for HPV6, HPV11, HPV16 and HPV18 at baseline (91.6% and 100%, respectively) and very good (67.6% and 87.5%, respectively) in the intention-to-treat analysis (Table 4). Furthermore, vaccine efficacies against HPV6 and HPV11-associated and HPV16 and HPV18-associated VIN2–3 or VAIN2–3 were also extremely good (>95%, Table 4) in those participants who were baseline HPV-negative.5,68 As seen for CIN lesions (Table 3), the vaccine efficacies against all VIN or VAIN lesions increased as the grade of the lesion increased—VIN1 or VAIN1 vaccine efficacy was 54.8%, whereas for VIN2–3 or VAIN2–3 the efficacy was 77.1% (Table 4).
Anal intraepithelial neoplasia
Vaccine efficacies against anal HPV16 and HPV18 infection and precursors of anal cancer (anal intraepithelial neoplasia [AIN]) have been reported only for the quadrivalent vaccine in males,75 again partially because appropriate samples in these anatomical sites were not collected in the PATRICIA trial. However, from the Costa-Rican HPV16/18 trial, vaccine efficacy estimates against anal HPV16 and HPV18 infections in women are available.76 The vaccine efficacies are remarkably similar (83.6% and 84.5%) for the quadrivalent and bivalent vaccines against anal HPV16 and HPV18 infections in men and women (Table 5).75,76 Similar to the findings for cervical and vulvar or vaginal lesions (Tables 3 and 4), the vaccine efficacies for anal lesions tended to increase by lesion severity. In baseline HPV-negative men and all trial participants, vaccine efficacies against all AIN1+ were 54.9% and 25.7%, respectively, and the corresponding vaccine efficacies against all AIN2–3 lesions were 74.9% and 54.2%, respectively (Table 5).75
Increasing efficacy with increasing severity
The strong increase in vaccine efficacy with increasing lesion severity is largely attributed to accumulation of the more-oncogenic HPV types 16 and 18.1 However, in type-restricted analyses, the vaccine efficacies tend to be higher for severe lesions than for infection-related end points;3,68 accordingly, this accumulation cannot be the whole answer. For both vaccines, protection against the accumulation (cumulative incidence) of all CIN3 or AIS cases becomes detectable 18 months after vaccination (Figure 2). Cumulative incidence is significantly lower for baseline HPV-negative vaccinated individuals than for controls by 42 months, but in the intention-to-treat population the incidence is only lower for the bivalent vaccine cohort (Figure 2). In this context, the two vaccines have not demonstrated any therapeutic effects that could explain the effects on severe lesions.3,68
a | Women who were HPV PCR-negative at baseline and who received control or Cervarix® vaccines. b | The intention-to-treat cohort who received control or Cervarix® vaccines. c | Women who were HPV6, HPV11, HPV16 and HPV18 PCR-negative at baseline and who received control or Gardasil® vaccines. d | The intention-to-treat cohort who received control or Gardasil® vaccines. All data points have 95% CI error bars marked. Abbreviations: CIN, cervical intraepithelial neoplasia; HPV, human papillomavirus. Parts a and b reproduced with permission from Elsevier Ltd © Lehtinen, M. et al. Lancet Oncol. 13, 89–99 (2012), and parts c and d reproduced with permission from Oxford University Press © Muñoz, N. et al. J. Natl Cancer Inst. 102, 325–339 (2010).
Safety
As expected, the safety of the two prophylactic HPV vaccines, comprising only one viral (L1) protein and the different adjuvant agents, has proven to be excellent in various phase II and III trials both in females and males.2,3,4,5,52,66 That the quadrivalent vaccine is part of various different combinations of viral and/or bacterial vaccines does not seem to alter its tolerability.51,53 An emerging overall issue in vaccinology, however, is to address the so-called vaccine confidence gap.77 Although conventional adverse and serious adverse-effect reporting captures the majority of the possible (long-term) sequelae of vaccinations, cohort studies exploiting population-based health registries will be more comprehensive.78,79,80,81 Comprehensive studies linking sizeable cohorts and registries of HPV-vaccinated individuals with population-based health registries are ongoing in the Nordic countries.
Prospects for the future
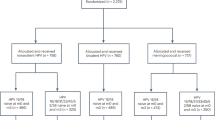
Evaluating the effectiveness of different vaccination strategies from both direct and indirect (herd-immunity derived) vaccine efficacy calls for evidence-based medicine. In controlled trials, the direct efficacy of HPV vaccines has been ≥90% against HPV infections or their sequelae in HPV-naive individuals (Tables 1, 2, 3, 4, 5). Early cost–efficacy studies reported that vaccination of both girls and boys (strategy A) was inferior to vaccination of girls only (strategy B).82 However, according to established dynamic transmission models, in moderate coverage scenarios, strategy A prevents up to three times more HPV infections than strategy B.83,84 These data imply that programmes with low-to-moderate coverage among girls only can be improved by extending vaccination to boys.25 Furthermore, the strength of the herd-immunity effect observed in Australia—that is, a reduction of genital warts in males stemming from vaccinating females only83—suggests that vaccinating boys is worth evaluating.
In the largest randomized effectiveness trial (with parental informed consent) involving 80,000 early adolescents, vaccine coverage among girls was 50% and among boys 20–30%.85 Previous experience of vaccinating 13-year old girls against rubella, and current school-based HPV vaccination programmes, suggest that reaching 70–80% vaccine coverage in girls is possible,86,87 but there are few reports of >80% general HPV vaccine coverage; marginalization of girls that remain both unvaccinated and unscreened makes the aspect of justice important for all vaccination strategies.88,89 Poor (<50%) rubella vaccine coverage resulted in increased incidence of congenital rubella syndrome in Greece, because of transfer of the epidemic peak from small and school-aged children to young adults.90 Nonorganized HPV vaccination programmes (that is, programmes that issue recommendations and provide subsidies, but do not organize the vaccinations) have had very low coverage rates (30–40%).91,92 Consequently, the possibility that nonorganized programmes trying to implement strategy B might increase social disparity should be seriously considered.
Comparing strategies A and B, equality between genders is also an important consideration—especially now that data are available on the very good (>90%) efficacy of the quadrivalent vaccine against genital HPV infection and associated lesions in males.66 Furthermore, a causal association between HPV infection and oropharyngeal and tonsillar cancer has been established.1,93 There are numerous reports of an epidemic increase in the incidence of HPV-associated oropharyngeal cancer94,95,96 and of an increasing incidence of anal cancer97,98 both in males and females. This increase underlines the fact that men are not only vectors for transmitting HPV infections to females, but a large number of HPV-associated cancers that occur in males that could be prevented by HPV vaccination. The high vaccine efficacies observed in males imply that common effort for HPV vaccination among the genders could result in control of the hitherto most-common sexually transmitted infection and the multiple diseases caused by HPV.
Conclusions
The two prophylactic HPV vaccines are highly efficacious against persistent anogenital infections, and moderately efficacious against a number of HPV types in the same clades not covered by the vaccines. For the bivalent vaccine, moderate cross-protection extends to HPV types in different clades, possibly because of conformational homology of the epitopes.99
The duration of prophylactic HPV vaccine efficacy is now approaching 10 years,100,101 but whether cross-protection will be equally long-lasting is unclear. Cancer registries are being used to monitor the long-term efficacy closely.72,74 In addition, the possible HPV-type replacement following increasing vaccination coverage is being closely monitored.102,103
With current, extremely efficacious vaccines, the focus of organized HPV vaccination programmes should change from reduction of the HPV disease burden to control of high-risk HPV (and low-risk HPV) types. The impact of herd immunity preferentially generated by vaccinating both genders has been suggested to tackle low coverage in girls-only vaccination programmes25 and will be evaluated in an upcoming (2014–2015) community randomized trial.85
Future modelling work should focus on eradicating the major high-risk HPV types. Modelling, which considers the already observed albeit varying, herd immunity following HPV vaccination85,104,105 and the dynamics of sexual transmission has implied that eradication from the general population will not be particularly difficult in both-sex vaccination scenarios.106 Even with currently available or studied bivalent to nonavalent (HPV types 6, 11, 16, 18, 31, 33, 35, 45 and 52) vaccines—and the probable broadly cross-reactive second-generation vaccines102,103eradication will be the ultimate solution to the dilemma of HPV and its high cancer burden.
Author contribution
Both authors researched data for the article, made a substantial contribution to the discussion of the content and wrote and revised the article prior to submission.
Review criteria
Published original articles reporting HPV vaccine immunogenicity or efficacy were identified using the PubMed database with the key words: “antibodies”, “cancer”, “human papillomavirus”, “sexually transmitted infections”, “sexually transmitted diseases” and “vaccine”.
Change history
11 November 2014
In the version of this Review article originally published online and in print in the July 2013 issue of Nature Reviews Clinical Oncology there were errors in the clinical data presented in Tables 2, 3 and 5. In addition, reference 68 should have been cited to support data in Table 2, and the efficacy of the bivalent vaccine in adenocarcinoma in situ was 76.9% rather than 100% as originally reported in the main text on page 405. The errors have been corrected in the HTML and PDF versions of the article.
References
International Agency for Research on Cancer. A Review of Human Carcinogens. Part B: Biological agents / IARC Working Group on the Evaluation of Carcinogenic Risks to Humans 255–314 (Lyon, France, 2009).
Paavonen, J. et al. Efficacy of a prophylactic adjuvanted L1 VLP vaccine against infection with human papillomavirus types 16 and 18 in young women: an interim analysis of a phase III double-blind, randomised controlled trial. Lancet 369, 2161–2170 (2007).
Lehtinen, M. et al. Overall efficacy of HPV-16/18 AS04-adjuvanted vaccine against grade 3 or greater cervical intraepithelial neoplasia: 4-year end-of-study analysis of the randomised, double-blind PATRICIA trial. Lancet Oncol. 13, 89–99 (2012).
The Future II Study Group. Quadrivalent vaccine against human papillomavirus to prevent high-grade cervical lesions. N. Engl. J. Med. 356, 1915–1927 (2007).
The FUTURE I/II Study Group. Four year efficacy of prophylactic human papillomavirus quadrivalent vaccine against low grade cervical, vulvar, and vaginal intraepithelial neoplasia and anogenital warts: randomised controlled trial. BMJ 341, c3493 (2010).
Collins, S. I. et al. Proximity of first intercourse to menarche and the risk of human papillomavirus infection: a longitudinal study. Int. J. Cancer 114, 498–500 (2005).
Winer, R. L. et al. Genital human papillomavirus infection: incidence and risk factors in a cohort of female university students. Am. J. Epidemiol. 157, 218–226 (2003).
Kjaer, S. K. et al. Acquisition and persistence of human papillomavirus infection in younger men: a prospective follow-up study among Danish soldiers. Cancer Epidemiol. Biomarkers Prev. 14, 1528–1533 (2005).
Dillner, J. et al. Seropositivies to human papillomavirus types 16, 18 and 33 capsids and to Chlamydia trachomastis are markers of sexual behaviour. J. Infect. Dis. 173, 1394–1398 (1996).
Koutsky, L. Epidemiology of genital human papillomavirus infection. Am. J. Med. 102, 3–8 (1997).
Winer, R. L. et al. Condom use and the risk of genital human papillomavirus infection in young women. N. Engl. J. Med. 354, 2645–2654 (2006).
Wawer, M. J. et al. Effect of circumcision of HIV-negative men on transmission of human papillomavirus to HIV-negative women: a randomised trial in Rakai, Uganda. Lancet 377, 209–218 (2011).
Doorbar, J. The papillomavirus life cycle. J. Clin. Virol. 32, S7–S15 (2005).
Moscicki, A. B. et al. Updating the natural history of human papillomavirus and anogenital cancers. Vaccine 30, F24–F33 (2012).
Clifford, G. M., Hoqwell-Jones, R. & Franceschi, S. Judging the carcinogenicity of human papillomavirus types by single/multiple infection ratio in cervical cancer. Int. J. Cancer 129, 1702–1794 (2011).
Schiffman, M., Clifford, G. & Buonaguro, F. M. Classification of weakly carcinogenic human papillomavirus types: addressing the limits of epidemiology at the borderline. Infect. Agents Cancer 4, 8 (2009).
Halec, G. et al. Biological activity of probable/possible high-risk human papillomavirus types in cervical cancer. Int. J. Cancer 132, 62–71 (2013).
Namujju, P. B. et al. Risk of being seropositive for multiple human papillomavirus types among Finnish and Ugandan women. Scand. J. Infect. Dis. 42, 522–526 (2010).
Stanley, M. HPV—immune response to infection and vaccination. Infect. Agent Cancer 5, 19 (2010).
Kjellberg, L. et al. Sexual behaviour and papillomavirus exposure in cervical intraepithelial neoplasia: a population-based case-control study. J. Gen. Virol. 80, 391–398 (1999).
Lin, S. W. et al. HPV16 seropositivity and subsequent HPV16 infection risk in a naturally infected population: comparison of serological assays. PLoS ONE 8, e53067 (2013).
Palmroth, J. et al. Natural seroconversion to high-risk human papillomaviruses (hrHPVs) is not protective against related HPV genotypes. Scand. J. Infect. Dis. 42, 379–384 (2010).
Szarewski, A. et al. Efficacy of the human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine in women aged 15–25 years with and without serological evidence of previous exposure to HPV-16/18. Int. J. Cancer 131, 106–116 (2012).
Bulkmans, N. W. et al. High-risk HPV type-specific clearance rates in cervical screening. Br. J. Cancer 96, 1419–1424 (2007).
Vanska, S., Lehtinen, M. & Auranen, K. Explaining different HPV clearance rate estimates with different proportions of persistent infections [abstract]. 28th International Papillomavirus Conference EP-412 (2012).
Anttila, T. et al. Serotypes of Chlamydia trachomatis and risk for development of cervical squamous cell carcinoma. JAMA 285, 47–51 (2001).
Lehtinen, M. et al. Chlamydia trachomatis infection and risk of cervical intraepithelial neoplasia. Sex. Transm. Infect. 87, 372–376 (2011).
Plummer, M. et al. Smoking and cervical cancer: pooled analysis of the IARC multi-centric case—control study. Cancer Causes Control 14, 805–814 (2003).
Kapeu, A. S. et al. Is smoking an independent risk factor for invasive cervical cancer? A nested case-control study within Nordic biobanks. Am. J. Epidemiol. 169, 480–488 (2009).
Luostarinen, T. et al. Order of HPV/Chlamydia infections and cervical high-grade precancer risk: a case-cohort study. Int. J. Cancer http://dx.doi.org/10.1002/ijc.28173.
Ylä-Outinen, A. et al. in Chlamydial Infections (eds Stamm, W. E. et al.) 323–326 (Cambridge University Press, New York, 1990).
Silins, I. et al. Chlamydia trachomatis infection and persistence of human papillomavirus. Int. J. Cancer 116, 110–115 (2005).
Syrjänen, K. et al. Smoking is an independent risk factor for oncogenic human papillomavirus (HPV) infections but not for high-grade CIN. Eur. J. Epidemiol. 22, 723–735 (2007).
Simen-Kapeu, A. et al. Smoking impairs human papillomavirus (HPV) type 16 and 18 capsids antibody response following natural HPV infection. Scand. J. Infect. Dis. 40, 745–751 (2008).
Szarewski, A. et al. Effect of smoking cessation on cervical lesion size. Lancet 347, 941–943 (1996).
Trottier, H. et al. Human papillomavirus infections with multiple types and risk of cervical neoplasia. Cancer Epidemiol. Biomarkers Prev. 15, 1274–1280 (2006).
Lehtinen, M. et al. Seroprevalence atlas of infections with oncogenic and non-oncogenic human papillomaviruses in Finland in the 1980s and 1990s. Int. J. Cancer 119, 2612–2619 (2006).
Kaasila, M. et al. Population dynamics of serologically defined coinfections with human papillomavirus types 11, 16, 18 and 31 in fertile-aged Finnish women. Int. J. Cancer 125, 2166–2172 (2009).
Insinga, R. P. et al. Incidence, duration, and reappearance of type-specific cervical human papillomavirus infections in young women. Cancer Epidemiol. Biomarkers Prev. 19, 1585–1594 (2010).
Merikukka, M. et al. Differences in incidence and co-occurrence of vaccine and nonvaccine human papillomavirus types in Finnish population before human papillomavirus mass vaccination suggest competitive advantage for HPV33. Int. J. Cancer 128, 1114–1119 (2011).
Vaccarella, S. et al. Clustering of multiple human papillomavirus infections in women from a population-based study in Guanacaste, Costa Rica. J. Infect. Dis. 204, 385–390 (2011).
Vaccarella, S. et al. Clustering of human papillomavirus (HPV) types in the male genital tract: the HPV in men (HIM) study. J. Infect. Dis. 204, 1500–1504 (2011).
Trottier, H. et al. Type-specific duration of human papillomavirus infection: implications for human papillomavirus screening and vaccination. J. Infect. Dis. 197, 1436–1447 (2008).
Trottier, H. et al. Human papillomavirus infection and reinfection in adult women: the role of sexual activity and natural immunity. Cancer Res. 70, 8569–8577 (2010).
Calabro, S. et al. Vaccine adjuvants alum and MF59 induce rapid recruitment of neutrophils and monocytes that participate in antigen transport to draining lymph nodes. Vaccine 29, 1812–1823 (2011).
Serre, K. et al. IL-4 directs both CD4 and CD8 T cells to produce Th2 cytokines in vitro, but only CD4 T cells produce these cytokines in response to alum-precipitated protein in vivo. Mol. Immunol. 47, 1914–1922 (2010).
Dauner, J. G., Pan, Y., Hildesheim, A., Harro, C. & Pinto, L. A. Characterization of the HPV-specific memory B cell and systemic antibody responses in women receiving an unadjuvanted HPV16 L1 VLP vaccine. Vaccine 28, 5407–5413 (2010).
Giannini, S. L. et al. Enhanced humoral and memory B cellular immunity using HPV16/18 L1 VLP vaccine formulated with the MPL/aluminium salt combination (AS04) compared to aluminium salt only. Vaccine 24, 5937–5949 (2006).
Pedersen, C. et al. Immunization of early adolescent females with human papillomavirus type 16 and 18 L1 virus-like particle vaccine containing AS04 adjuvant. J. Adolesc. Health 40, 564–571 (2007).
Perez, G. et al. Safety, immunogenicity, and efficacy of quadrivalent human papillomavirus (types 6, 11, 16, 18) L1 virus-like-particle vaccine in Latin American women. Int. J. Cancer 122, 1311–1318 (2008).
Wheeler, C. M. et al. Safety and immunogenicity of co-administered quadrivalent human papillomavirus (HPV)-6/11/16/18 L1 virus-like particle (VLP) and hepatitis B (HBV) vaccines. Vaccine 26, 686–696 (2008).
Petäjä, T. et al. Immunogenicity and safety of human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine in healthy boys aged 10–18 years. J. Adolesc. Health 44, 33–41 (2009).
Vesikari, T. et al. An open-label, randomized, multicenter study of the safety, tolerability, and immunogenicity of quadrivalent human papillomavirus (types 6/11/16/18) vaccine given concomitantly with diphtheria, tetanus, pertussis, and poliomyelitis vaccine in healthy adolescents 11 to 17 years of age. Pediatr. Infect. Dis. J. 29, 314–318 (2010).
Giuliano, A. R. Human papillomavirus vaccination in males. Gynecol. Oncol. 107, S24–S26 (2007).
Kapeu, A. Epidemiological Study of Tobacco Use and Human Papillomavirus Thesis, University of Tampere (2009).
Villa, L. L. et al. High sustained efficacy of a prophylactic quadrivalent human papillomavirus types 6/11/16/18 L1 virus-like particle vaccine through 5 years of follow-up. Br. J. Cancer 95, 1459–1466 (2006).
Roteli-Martins, C. M. et al. Sustained immunogenicity and efficacy of the HPV-16/18 AS04-adjuvanted vaccine: up to 8.4 years of follow-up. Hum. Vaccin. Immunother. 3, 390–397 (2012).
Olsson, S. E. et al. Induction of immune memory following administration of a prophylactic quadrivalent human papillomavirus (HPV) types 6/11/16/18 L1 virus-like particle (VLP) vaccine. Vaccine 25, 4931–4939 (2007).
Roberts, C., Swoyer, R. & Bryan, J. Evaluation of the HPV 18 antibody response in Gardasil® vaccinees after 48 mo using a pseudovirion neutralization assay. Hum. Vaccin. Immunother. 4, 431–434 (2012).
Joura, E. A. et al. HPV antibody levels and clinical efficacy following administration of a prophylactic quadrivalent HPV vaccine. Vaccine 26, 6844–6851 (2008).
Einstein, M. H. et al. Comparison of the immunogenicity and safety of Cervarix and Gardasil human papillomavirus (HPV) cervical cancer vaccines in healthy women aged 18–45 years. Hum. Vaccin. 10, 705–719 (2010).
Draper, E. et al. Neutralization of non-vaccine human papillomavirus pseudoviruses from the A7 and A9 species groups by bivalent HPV vaccine sera. Vaccine 29, 8285–8290 (2011).
Petäjä, T. et al. Long-term persistence of systemic and mucosal immune response to HPV-16/18 ASO4-adjuvanted vaccine in preteen/adolescents girls and young women. Int. J. Cancer 129, 2147–2157 (2011).
Cuzick, J. et al. Comparing the performance of six human papillomavirus tests in a screening population. Br. J. Cancer 108, 908–903 (2013).
Szarewski, A. et al. Efficacy of the HPV-16/18 AS04-adjuvanted vaccine against HPV types associated with genital warts [abstract]. EUROGIN 2012 Congress SS 12–2 (2012).
Giuliano, A. R. et al. Efficacy of quadrivalent HPV vaccine against HPV infection and disease in males. N. Engl. J. Med. 364, 401–411 (2011).
Wilkin, T. et al. Safety and immunogenicity of the quadrivalent human papillomavirus vaccine in HIV-1-infected men. J. Infect. Dis. 202, 1246–1253 (2010).
Muñoz, N. et al. Impact of human papillomavirus (HPV)-6/11/16/18 vaccine on all HPV-associated genital diseases in young women. J. Natl Cancer Inst. 102, 325–339 (2010).
Carreon, J. D. et al. CIN2 is a much less reproducible and less valid diagnosis than CIN3: results from a histological review of population-based cervical samples. Int. J. Gynecol. Pathol. 26, 441–446 (2007).
Castle, P. E., Schiffman, M., Wheeler, C. M. & Solomon, D. Evidence for frequent regression of cervical intraepithelial neoplasia-grade 2. Obstet. Gynecol. 113, 18–25 (2009).
Kjaer, S. K. et al. A pooled analysis of continued prophylactic efficacy of quadrivalent human papillomavirus (Types 6/11/16/18) vaccine against high-grade cervical and external genital lesions. Cancer Prev. Res. (Phila.) 2, 868–878 (2009).
Rana, M. M. et al. Understanding long-term protection of human papillomavirus vaccination against cervical carcinoma: cancer registry-based follow-up. Int. J. Cancer 132, 2833–2838 (2013).
Brotherton, J. M. et al. Early effect of the HPV vaccination programme on cervical abnormalities in Victoria, Australia: an ecological study. Lancet 377, 2085–2092 (2011).
Lehtinen, M. et al. Chapter 28: Studies to assess long-term efficacy and effectiveness of HPV vaccination in developed and developing countries. Vaccine 24 (Suppl. 3), 233–241 (2006).
Palefsky, J. M. et al. HPV vaccine against anal HPV infection and anal intraepithelial neoplasia. N. Engl. J. Med. 365, 1576–1585 (2011).
Kreimer, A. R. et al. Efficacy of a bivalent HPV 16/18 vaccine against anal HPV16/18 infection among young women: a nested analysis within the Costa Rica Vaccine Trial. Lancet Oncol. 12, 862–870 (2011).
Larson, H. J., Cooper, L. Z., Eskola, J., Katz, S. L. & Ratzan, S. Addressing the vaccine confidence gap. Lancet 378, 526–535 (2011).
Hviid, A., Steffeld, M., Wohlfahrt, J. & Melbye, M. Childhood vaccination and type 1 diabetes. N. Engl. J. Med. 350, 1398–1404 (2004).
Pasternak, B. et al. Vaccination against pandemic A/H1N1 2009 influenza in pregnancy and risk of fetal death: cohort study in Denmark. BMJ 344, e2794 (2012).
Wacholder, S. et al. Risk of miscarriage with bivalent vaccine against human papillomavirus (HPV) types 16 and 18: pooled analysis of two randomised controlled trials. BMJ 340, c712 (2010).
Chao, C. et al. Surveillance of autoimmune conditions following routine use of quadrivalent human papillomavirus vaccine. J. Intern. Med. 271, 193–203 (2010).
Kim, J. J. & Goldie, S. Cost effectiveness analysis of including boys in a human papillomavirus vaccination programme in the United States. BMJ 339, b3884 (2009).
Barnabas, R. V. et al. Epidemiology of HPV 16 and cervical cancer in Finland and the potential of vaccination: mathematical modelling analyses. PLoS Med. 3, e138 (2006).
Regan, D. G., Philp, D. J., Hocking, J. S. & Law, M. G. Modelling the population-level impact of vaccination on the transmission of human papillomavirus type 16 in Australia. Sex. Health 4, 147–163 (2007).
Lehtinen, M., French, K. M., Dillner, J., Paavonen, J. & Garnett, G. Sound implementation of human papillomavirus vaccination as a community-randomized trial. Therapy 5, 289–294 (2008).
Peltola, H. et al. Mumps and rubella eliminated from Finland. JAMA 284, 2643–2647 (2000).
Brabin, L. et al. Uptake of first two doses of human papillomavirus vaccine by adolescent schoolgirls in Manchester: prospective cohort study. BMJ 336, 1056–1058 (2008).
Lehtinen, M. & Paavonen, J. Impact of human papillomavirus vaccination depends on effective vaccination strategy. Int. J. Cancer 125, 1490–1491 (2009).
Malmqvist, E., Natunen, K., Lehtinen, M. & Helgesson, G. Just implemention of human papillomavirus vaccination. J. Med. Ethics 38, 247–249 (2012).
Panagiotopoulos, T., Antoniadou, I. & Valassi-Adam, E. Increase in congenital rubella occurrence in Greece: retrospective survey and systematic review. BMJ 319, 1462–1467 (1999).
Rouzier, R. & Giordanella, J. P. Coverage and compliance of human papilloma virus vaccines in Paris: demonstration of low compliance with non-school-based approaches. J. Adolesc. Health 47, 237–241 (2010).
Taylor, R., Hariri, S., Sterberg, M., Dunne, E. F. & Markowitz, L. E. Human papillomavirus vaccine coverage in the United States: National Health and Nutrition Examination Survey. Prev. Med. 52, 398–400 (2011).
Mork, J. et al. Human papillomavirus infection as a risk factor for squamous-cell carcinoma of the head and neck. N. Engl. J. Med. 344, 1125–1131 (2001).
Shiboski, C. H., Schmidt, B. L. & Jordan, R. C. Tongue and tonsil carcinoma: increasing trends in the U.S. population ages 20–44 years. Cancer 103, 1843–1849 (2005).
Näsman, A. et al. Incidence of human papillomavirus (HPV) positive tonsillar carcinoma in Stockholm, Sweden: an epidemic of viral-induced carcinoma? Int. J. Cancer 125, 362–366 (2009).
Brewster, D. H. & Bhatti, L. A. Increasing incidence of squamous cell carcinoma of the anus in Scotland, 1975–2002. Br. J. Cancer 95, 87–90 (2006).
Grulich, A. E., Jin, F., Conway, E. L., Stein, A. N. & Hocking, J. Cancers attributable to human papillomavirus infection. Sex. Health 7, 244–252 (2010).
Lehtinen, M. & Paavonen, J. Sound efficacy of prophylactic HPV vaccination: basics and implications. Oncoimmunology 1, 995–996 (2012).
Koutsky, L. A. et al. A controlled trial of a human papillomavirus type 16 vaccine. N. Engl. J. Med. 347, 1647–1651 (2002).
Romanowski, B. Long term protection against cervical infection with the human papillomavirus: review of currently available vaccines. Hum. Vaccin. 7, 161–169 (2011).
Palmroth, J. et al. Occurrence of vaccine and non-vaccine HPV types in adolescent Finnish females 4 years post-vaccination. Int. J. Cancer 131, 2832–2838 (2012).
Söderlund-Strand, A. & Dilner, J. High-throughput monitoring of human papillomavirus type distribution. Cancer Epidemiol. Biomarkers Prev. 22, 242–250 (2013).
Donovan, B. et al. Quadrivalent human papillomavirus vaccination and trends in genital warts in Australia: analysis of national sentinel surveillance data. Lancet Infect. Dis. 11, 39–44 (2011).
Leval, A. et al. Quadrivalent human papillomavirus vaccine effectiveness: a Swedish national cohort study. J. Natl Cancer Inst. 105, 469–474 (2013).
Baandrup, L. et al. Significant decrease in the incidence of genital warts in young Danish women after implementation of a national human papillomavirus vaccination program. Sex. Transm. Dis. 40, 130–135 (2013).
Garnett, G. P. Role of herd immunity in determining the effect of vaccines against sexually transmitted disease. J. Infect. Dis. 191, S97–S106 (2005).
Stanley, M. Prospects for new HPV vaccines. Curr. Opin. Infect. Dis. 1, 70–75 (2010).
Nieto, K. et al. Development of AAVLP (HPV16/31L2) particles as broadly protective HPV vaccine candidate. PLoS ONE 7, e39741 (2012).
Herrero, R. et al. Prevention of persistent human papillomavirus infection by an HPV16/18 vaccine: a community-based randomized clinical trial in Guanacaste, Costa Rica. Cancer Discov. 1, 408–419 (2011).
Wheeler, C. M. et al. Efficacy of the HPV-16/18 AS04-adjuvanted vaccine against cervical infection and precancer caused by oncogenic HPV types: 4-year end-of-study analysis of the randomised, double-blind PATRICIA trial. Lancet Oncol. 13, 100–110 (2012).
Brown, D. R. et al. The impact of quadrivalent human papillomavirus (HPV; types 6, 11, 16, and 18) L1 virus-like particle vaccine on infection and disease due to oncogenic nonvaccine HPV types in generally HPV-naive women aged 16–26 years. J. Infect. Dis. 199, 926–935 (2009).
Acknowledgements
The financial support of Nordic Cancer Union and EU FP7 PREHDICT Network is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
M. Lehtinen and J. Dillner have received grants to their institutions to conduct clinical trials and follow-up studies of HPV vaccines from Merck & Co, GlaxoSmithKline Biologicals (ML) and Sanofi-Pasteur MSD (J. Dillner). J. Dillner has participated in the steering group of a phase III vaccination trial sponsored by Merck.
Supplementary information
Supplementary Table 1
Reported efficacies of two licensed human papillomavirus (HPV) vaccines against 6 month persistent cervical HPV infection in women negative for HPV PCR at study entry (Baseline negative) or in all participating women (Intention-to-treat). Data from end-of-study analyses. (PDF 330 kb)
Rights and permissions
About this article
Cite this article
Lehtinen, M., Dillner, J. Clinical trials of human papillomavirus vaccines and beyond. Nat Rev Clin Oncol 10, 400–410 (2013). https://doi.org/10.1038/nrclinonc.2013.84
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrclinonc.2013.84
This article is cited by
-
HPV-Impfung und das Risiko eines invasiven Zervixkarzinoms
Der Onkologe (2021)
-
Measuring vaccine effectiveness against persistent HPV infections: a comparison of different statistical approaches
BMC Infectious Diseases (2020)
-
Impact of HPV vaccination on cervical screening performance: a population-based cohort study
British Journal of Cancer (2020)
-
Peak neutralizing and cross-neutralizing antibody levels to human papillomavirus types 6/16/18/31/33/45/52/58 induced by bivalent and quadrivalent HPV vaccines
npj Vaccines (2020)
-
Assessing the cost-effectiveness of HPV vaccination strategies for adolescent girls and boys in the UK
BMC Infectious Diseases (2019)