Abstract
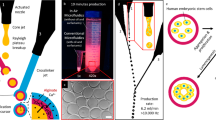
Microengineering human “organs-on-chips” remains an open challenge. Here, we describe a robust microfluidics-based approach for the differentiation of human pluripotent stem cells directly on a chip. Extrinsic signal modulation, achieved through optimal frequency of medium delivery, can be used as a parameter for improved germ layer specification and cell differentiation. Human cardiomyocytes and hepatocytes derived on chips showed functional phenotypes and responses to temporally defined drug treatments.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Huh, D., Torisawa, Y., Hamilton, G.A., Kim, H.J. & Ingber, D.E. Lab Chip 12, 2156–2164 (2012).
Ghaemmaghami, A.M., Hancock, M.J., Harrington, H., Kaji, H. & Khademhosseini, A. Drug Discov. Today 17, 173–181 (2012).
Huh, D. et al. Science 328, 1662–1668 (2010).
Lee, S.-A. et al. Lab Chip 13, 3529–3537 (2013).
Jang, K.-J. et al. Integr. Biol. 5, 1119–1129 (2013).
Grosberg, A., Alford, P.W., McCain, M.L. & Parker, K.K. Lab Chip 11, 4165–4173 (2011).
Sasai, Y. Nature 493, 318–326 (2013).
Eiraku, M. et al. Nature 472, 51–56 (2011).
Discher, D.E., Mooney, D.J. & Zandstra, P.W. Science 324, 1673–1677 (2009).
Przybyla, L.M. & Voldman, J. Proc. Natl. Acad. Sci. USA 109, 835–840 (2012).
Moledina, F. et al. Proc. Natl. Acad. Sci. USA 109, 3264–3269 (2012).
Figallo, E. et al. Lab Chip 7, 710–719 (2007).
Villa-Diaz, L.G. et al. Lab Chip 9, 1749–1755 (2009).
Korin, N., Bransky, A., Dinnar, U. & Levenberg, S. in Proc. SPIE 6416, 64160N (2006).
Giobbe, G.G. et al. Biotechnol. Bioeng. 109, 3119–3132 (2012).
Inui, M. et al. Nat. Cell Biol. 13, 1368–1375 (2011).
Xu, R.-H. et al. Cell Stem Cell 3, 196–206 (2008).
Yusa, K. et al. Nature 478, 391–394 (2011).
Manyike, P.T., Kharasch, E.D., Kalhorn, T.F. & Slattery, J.T. Clin. Pharmacol. Ther. 67, 275–282 (2000).
Watkins, P.B. et al. J. Am. Med. Assoc. 296, 87–93 (2006).
Luni, C., Michielin, F., Barzon, L., Calabrò, V. & Elvassore, N. Biophys. J. 104, 934–942 (2013).
Warren, L. et al. Cell Stem Cell 7, 618–630 (2010).
Zatti, S. et al. Mol. Ther. Methods Clin. Dev. 1, 1–9 (2014).
Rashid, S.T. et al. J. Clin. Invest. 120, 3127–3136 (2010).
Chambers, S.M. et al. Nat. Biotechnol. 27, 275–280 (2009).
Camnasio, S. et al. Neurobiol. Dis. 46, 41–51 (2012).
Kouskoff, V., Lacaud, G., Schwantz, S., Fehling, H.J. & Keller, G. Proc. Natl. Acad. Sci. USA 102, 13170–13175 (2005).
Hay, D.C. et al. Proc. Natl. Acad. Sci. USA 105, 12301–12306 (2008).
Lian, X. et al. Proc. Natl. Acad. Sci. USA 109, E1848–E1857 (2012).
Hay, D.C. et al. Stem Cells 26, 894–902 (2008).
Levy, L. et al. Mol. Cell. Biol. 27, 6068–6083 (2007).
Slager, H.G., Freund, E., Buiting, A.M.J., Feijen, A. & Mummery, C.L. J. Cell. Physiol. 156, 247–256 (1993).
Martewicz, S. et al. Integr. Biol. (Camb) 4, 153–164 (2012).
Zambon, A., Zoso, A., Luni, C., Frommer, W.B. & Elvassore, N. Integr. Biol. (Camb) 6, 277–288 (2014).
Livak, K.J. & Schmittgen, T.D. Methods 25, 402–408 (2001).
Acknowledgements
This research was supported by Progetti di Eccellenza Cassa di Risparmio di Padova e Rovigo (CARIPARO), Progetti di Eccellenza Giovani Ricercatori of Ministero della Salute and Progetto Strategico Università di Padova. We acknowledge Miltenyi Biotec for kindly providing the mRNA reprogramming kit. We thank L.Vallier (Cambridge University) and the Cambridge NIhR BRC hIPSC core facility for providing us A1ATD and corrected hiPS cell lines, and M. Oshimura (Department of Biomedical Science, Institute of Regenerative Medicine and Biofunction, Tottori University, Japan.) for the ADHF#1 hiPS cell line.
Author information
Authors and Affiliations
Contributions
G.G.G., F.M. and N.E. designed the research; G.G.G. and F.M. performed the experiments; S.M. performed cardiac functional tests; S.G. helped in microfluidic platform set-up and microfluidic cell culture; S.G. and C.L performed reprogramming experiments; S.D. helped in TGF-β experiments; A.F. supervised hepatic differentiation experiments; N.E. coordinated the project; G.G.G., F.M. and N.E. wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Integrated supplementary information
Supplementary Figure 1 Frequency-dependent signaling model output.
Temporal profiles of normalized Ex and En factors concentrations in the microfluidic channel at increasing frequencies (top). Gene transcript (Gt) concentration profile plotted versus corresponding transcription factor (Tf) variation during a single medium perfusion cycle at increasing perfusion frequencies. C tilde represents normalized concentration.
Supplementary Figure 2 Discontinuous vs. continuous perfusion culture conditions in microfluidic channels.
(a) Cell colonies morphology and nuclei distribution of hES2 cells were compared after 3 days of culture in discontinuous perfusion (f = 2 d-1) and continuous perfusion (flowrate 8 nL/min). Same overall amount of medium (12 µL per day) was used to ensure proper comparison between the two conditions. High inhomogeneity of cell growth along the channel, with higher growth at the inlet compared to the outlet, was observed only in continuous perfusion condition, although uniform OCT4 and NANOG expression. Scale bar, 100 μm. (b) Quantification of cell colony diameters at the inlet, in the center and at the outlet of micro-channels confirms high inhomogeneity only in continuous perfusion, with statistically significant differences between each of the paired conditions. Data are shown as mean ± s.d. (n = 12); ANOVA **P ≤ 0.01.
Supplementary Figure 3 Pluripotency markers expression of hPSCs cultured in micro-channels with f = 2d−1.
Homogeneous OCT4 and SOX2 expression was observed along the micro-channels with no upstream and downstream effects (quantitative analysis of OCT4 and SOX2 mean fluorescence intensity between inlet and outlet show differences smaller than 10%) in both HES2 (a) and ADHF#1 cells (b). Scale bars, 400 μm.
Supplementary Figure 4 Glucose and metabolites (ammonia and lactate) analyses.
Glucose, ammonia and lactate concentrations were analyzed on conditioned media collected from hESCs cultured in microfluidic channels, compared to static culture in Petri dish. HES2 cells were plated into microfluidic platforms and in standard Petri dish with the same cell density and cultured up to 5 days. Conditioned media were sampled from Petri dish after 24 h every day and from microfluidic channels after every perfusion cycle. Specifically, 8 μL exhaust medium were collected from each channel every 3, 12 or 24 h corresponding to f = 8, 2, 1d−1 for 5 days from cells seeding. Fresh medium was used as positive (for glucose) or negative (for ammonia and lactate) control. (a) Glucose concentration of medium inside a microfluidic channel (with no cells seeded) is equivalent to fresh medium. Interestingly only a 25% statistical decrease of glucose concentration was observed for low frequencies f = 2d−1 and f = 1d−1, compared to standard condition in Petri Dish. (b) Ammonia and lactate concentrations result equal or lower than those measured in static culture for every condition analyzed. Surprisingly, ammonia concentration (left) results statistically lower in media collected from micro-channels than that collected in static condition. This is probably due to the high ammonia diffusion through PDMS, which causes ammonia depletion from micro-channels. Lactate concentration (right) in exhaust medium of micro-channels is comparable or lower than the one observed in standard Petri dish. Data are shown as mean ± s.d. (n = 6) t-test **P ≤ 0.01.
1. Provin, C. & Fujii, T. Lab. Chip 11, 2948–2954 (2011).
Supplementary Figure 5 Determination of the optimal conditions to detect TGF-β ligands present in conditioned media.
TGF-β ligands are secreted from cells in a latent form that is not able to bind and activate TGF-β receptors. To measure its biological activity, it is thus necessary to release TGF-β ligands from the latency-associated peptide (LAP), either by heat treatment or medium acidification2,3,4,5. (a) We first checked which method was less detrimental for the activity of recombinant TGF-β1 (i.e. of the ligand in absence of LAP), by using active recombinant TGF-β1 (1ng/mL), either untreated (NT) or treated (95°C or acid pH). Media were then added to HaCaT cells bearing the stable SMAD2/3 CAGA12-luciferase reporter. Addition of the TGF-β receptor inhibitor SB431542 (10μM, +SB) to untreated medium sets the reporter background in absence of any SMAD activation. Acid treatment was detrimental for exogenous recombinant Tgfβ activity and excluded from further analyses. (b) E7 medium without exogenous TGF-β1 was conditioned by HES2 cells, cultured in standard Petri dishes in feeder-free conditions, and used to treat HaCaT CAGA12-luciferase cells for 8h. Untreated conditioned medium (E7) was barely active; heat-treatment of the same medium (95°C) instead released latent TGF-β ligands and caused a strong activation of the SMAD2/3 reporter. Addition of the TGF-β receptor inhibitor to the heat-activated medium (+SB) ensures that luciferase activation depends on extracellular factors. Data are normalized on total protein content, determined through Bradford assay. Data are shown as mean ± s.d. (n = 3).
2. Brown, P. D., Wakefield, L. M., Levinson, A. D. & Sporn, M. B. Growth Factors Chur Switz. 3, 35–43 (1990).
3. Gleizes, P.-E. et al. STEM CELLS 15, 190–197 (1997).
4. Slager, H. G., Freund, E., Buiting, A. M. J., Feijen, A. & Mummery, C. L. J. Cell. Physiol. 156, 247–256 (1993).
5. Lyons, R. M., Keski-Oja, J. & Moses, H. L. J. Cell Biol. 106, 1659-1665 (1988).
Supplementary Figure 6 HiPSCs spontaneous differentiation in static and microfluidics.
QRT-PCR analysis of endoderm markers. EOMES, FOXA2 and SOX17 expression of hiPSCs after spontaneous differentiation for 5 days on chip at f = 8 d−1 compared to Petri dishes (static). Data normalized on GAPDH and shown as mean ± s.e. (n = 3) t-test * P ≤ 0.05, ** P ≤ 0.01.
Supplementary Figure 7 Germ layer specification with conditioned media in microfluidics.
(a) Experimental design. HES2 cells were plated in microfluidic chips, cultured for 3 days and induced to differentiate into early germ-layers under spontaneous differentiation conditions for 4 days as reported in experiment of Fig.2a. During spontaneous differentiation, fresh medium was perfused with f = 1 d−1 and f = 8 d−1. Conditioned medium was collected from the f = 1 d−1 experiment, diluted at a 1:1 ratio with fresh medium and used to differentiate cells with f = 8 d−1, as schematically shown. (b) Expression of representative genes for each germ layer (OTX2 for ectoderm, T and EOMES for meso-endoderm) measured through qRT-PCR analysis. Consistently with data reported in Fig.2a, OTX2 is expressed at a lower perfusion frequency. Conversely, a higher perfusion frequency promotes T and EOMES marker expression. By using conditioned medium, a significant 2.5-fold increase in OTX2 expression and a 3-fold decrease in T expression were observed. These data support the hypothesis that conditioned medium containing a higher accumulation of cell-secreted endogenous factors induces a cell-fate switch between ectoderm and meso-endoderm commitment, even at a high perfusion frequency. Data are shown as mean ± s.e.m. (n = 6); t-test *P ≤ 0.05, **P ≤ 0.01.
Supplementary Figure 8 Uniform hepatic differentiation of hESCs along microfluidic channels.
HES2 differentiation at f = 4 d−1 in micro-channels. Top, at day 5 of endoderm induction cells show high and homogenous AFP expression (quantitative analysis of AFP mean fluorescence intensities between inlet and outlet show differences smaller than 15%, which is within experimental variability). Bottom, at day 10 hepatic epithelium is visible, with cells showing polygonal epithelial shape along microfluidic channel, and homogenous cell distribution. Scale bars, 400 μm.
Supplementary Figure 9 Endoderm differentiation in static vs. microfluidic culture condition.
HES2 cells were seeded in 24-well plates or microfluidic channels and induced to differentiate into endoderm after 3 days. Six different differentiation protocols were tested in order to demonstrate possible advantages of microfluidic environment in terms of cells vitality (final number of cells/initial number of cells) and efficiency of 5-days endoderm specification. Basal medium for endoderm commitment contain high concentration of Activin-A (100ng/mL) and Wnt3a (50ng/mL) for the first 2 days and Activin-A (100ng/mL) for the following 3 days. f = 4 d−1 was used for microfluidic differentiation. Different basal medium supplementations include B27-supplement, FBS (not chemically defined) and KSR at two different concentrations, i.e. 0.5 and 5%. Efficiency of endoderm specification after 5 days was determined by double immunostaining with endoderm-specific markers SOX17 and FOXA2. B27-supplement with sodium buthyrate (NaB) was previously used for specific endoderm commitment (Fig.2c), ensuring high efficiency (near 100%) both in static and microfluidic condition. However, addition of NaB, which is recognized to promote homogeneous hepatocyte differentiation and, if combined with Activin-A, an efficient definitive endoderm commitment6, causes dramatic cell death upon treatment both in static and microfluidic condition, whereas NaB removal allows increased cell survival and reduced efficiency. Nevertheless, a statistical significant 4-fold increase of SOX17+FOXA2+ cells was observed in microfluidic channels compared to standard Petri dish. Low concentration FBS-supplemented medium is widely employed for endoderm commitment, as higher concentrations inhibit endoderm commitment, even though promoting cell survival7. Consistently, increasing FBS concentration promotes cell survival and proliferation, whereas reducing efficiency in static condition. Surprisingly, intermittent perfusion allows increased proliferation compared to Petri dish and efficiency comparable with that obtained in low-serum condition. Particularly, a significant 4-fold increase of SOX17+ FOXA2+ cells in microfluidic compared to static condition was observed, when 0.5% FBS supplementation is used. Knock out serum replacement (KSR) is also recognized to inhibit hESCs differentiation and promote self-renewal, by means of PI3K signaling activation8. Again, a significant 3-fold increase of SOX17+ FOXA2+ cells in microfluidic compared to static condition was observed, with 0.5% KSR supplementation. No significant differences were observed with higher concentration of KSR. Scale bars, 100μm. Data are shown as mean ± s.e. (n = 6) t-test * P ≤ 0.05, ** P ≤ 0.01.
6. Hay, D. C. et al. STEM CELLS 26, 894–902 (2008).
7. Sui, L., Bouwens, L. & Mfopou, J. K. Int. J. Dev. Biol. 57, 1–12 (2013).
8. McLean, A. B. et al. Stem Cells Dayt. Ohio 25, 29–38 (2007).
Supplementary Figure 10 Frequency-dependent microfluidic hPSC differentiation into cardiomyocytes and hepatocyte-like cells.
(a) Microfluidic cardiomyocyte differentiation protocol and morphology changes from pluripotent state to differentiated cell type. Scale bars, 50 μm. (b) Hepatic differentiation protocol and cell change in morphology up to hepatocyte-like cells. Hepatocyte-like cells show characteristic polygonal cell shape in late stages. Scale bar, 100 μm.
Supplementary Figure 11 Microfluidic hepatic differentiation of various hPSCs.
Immunofluorescence panel shows cell morphology (bright field and F-ACTIN) and hepatic markers (CK-18 and ALBUMIN) expression of HES2 and differently derived hiPSCs: ADHF#1, A1ATZ/Z deficiency and A1ATR/R corrected (retrovirus-derived), Send#1 (Sendai virus-derived), mRNA#1-2-3-4 (modified mRNAs-derived). Scale bar, 50 μm.
Supplementary Figure 12 Albumin ELISA of hPSC-derived hepatocyte-like cells.
Graph shows quantification of secreted human albumin from differently derived hPSCs at day 16 of hepatic differentiation. Data are shown as mean ± s.d. (n = 3).
Supplementary Figure 13 Hepatic differentiation of hESCs in static and microfluidic conditions.
Immunostaining of HES2-derived hepatocyte-like cells show similar expression of CK-18 in static and microfluidic conditions, and higher expression of ALB and CYP3A in microfluidic compared to static condition. Scale bar, 40 μm.
Supplementary Figure 14 Acetaminophen-induced cytotoxicity in HepG2 cell line.
(a) HepG2 cells were exposed for 24 h to different concentrations of acetaminophen and analyzed through live and dead assays to quantify cell death in response to drug treatment. Cells cultured in medium with DMSO 1% (drug solvent) were used as control. No notable differences in the dead cells fraction were observed between static and microfluidic (f = 2d−1) conditions. (b-c) Nuclear size analysis in cells treated with different acetaminophen concentrations for 24 h. Nuclear areas of HepG2 cultured in Petri dish and in microfluidic condition were calculated and represented as probability density function (b) and cumulative density function (c). Cell nuclei area diminishes at higher acetaminophen concentrations in response to growing cell cytotoxicity (50 mM static data is missing because of cell detachment). The reduction in nuclear area at growing drug concentrations is more notable in microfluidic-cultured cells compared to static control cells.
Supplementary Figure 15 Acetaminophen-induced cytotoxicity in hESC-derived hepatocyte-like cells in a microfluidic platform.
HES2 cells were differentiated into functional hepatocytes expressing albumin, as revealed by immunostaining, in microfluidic channels. At day 22 of differentiation they were treated for 24 h with different acetaminophen concentrations, by using f = 2 d−1. Immunofluorescence shows F-actin staining for cell morphology. At increasing drug concentrations, cell morphology is disrupted in response to acetaminophen cytotoxicity, especially at 25 mM with almost complete loss of cell structure and function. Scale bar, 30 μm.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–15, and Supplementary Notes 1 and 2 (PDF 2869 kb)
HESC-derived cardiomyocytes on a chip
Spontaneous contraction of HES2-derived cardiomyocytes differentiated in a microfluidic channel (day 13). (MOV 497 kb)
HiPSC-derived cardiomyocytes on a chip
Spontaneous contraction of ADHF#1-derived cardiomyocytes differentiated in a microfluidic channel (day 16). (MOV 824 kb)
Channel view of HESC-derived cardiomyocytes on a chip
Beating monolayer of HES2-derived cardiomyocytes differentiated in a microfluidic channel (day 16). (MOV 5683 kb)
Rights and permissions
About this article
Cite this article
Giobbe, G., Michielin, F., Luni, C. et al. Functional differentiation of human pluripotent stem cells on a chip. Nat Methods 12, 637–640 (2015). https://doi.org/10.1038/nmeth.3411
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nmeth.3411
This article is cited by
-
A quantitative meta-analysis comparing cell models in perfused organ on a chip with static cell cultures
Scientific Reports (2023)
-
Evaluating the antioxidant potential of resveratrol-gold nanoparticles in preventing oxidative stress in endothelium on a chip
Scientific Reports (2023)
-
A microfabricated multi-compartment device for neuron and Schwann cell differentiation
Scientific Reports (2021)
-
Highly parallelized human embryonic stem cell differentiation to cardiac mesoderm in nanoliter chambers on a microfluidic chip
Biomedical Microdevices (2021)
-
Modular operation of microfluidic chips for highly parallelized cell culture and liquid dosing via a fluidic circuit board
Microsystems & Nanoengineering (2020)